Thyroidectomy refers to the surgical procedure in which your thyroid is removed.
While the surgical portion of the procedure is usually fairly easy, the aftermath as it relates to your serum thyroid levels may be a different story entirely.
Learn more about Thyroidectomy in this guide, including the basics of the procedure, the long-term consequences of having your thyroid removed, information on the recovery side of things, and how to feel like yourself after the procedure:
Thyroidectomy Basics
If you are reading this post then chances are high you either have gone through a thyroidectomy or it has been recommended as the next step in your treatment.
In either event, you are in the right place.
In this post, we will dive into the basic and more complex aspects of getting a thyroidectomy.
One of the major issues with getting a thyroidectomy is that it is treated as a routine procedure similar to getting your appendix removed.
From a surgical standpoint, this is definitely true (1).
But from a hormonal standpoint, this couldn’t be farther from the truth.
And one thing you may not realize, walking into the procedure, is that no matter how hard you try you will never experience “normal” thyroid levels again after your thyroid is removed.
Much of this has to do with how complex the thyroid system is in your body.
Your thyroid pumps out thyroid hormone based on the demand of your tissues all the time.
Your body is converting T4 into T3 based on the needs of the tissues and it has the ability to either slow down or speed up thyroid hormone production based on the needs (3) of your body.
But once you remove your thyroid, the ability to tightly control and regulate your thyroid is gone.
Instead, you will be placed on thyroid hormone medication (usually once per day) and told that this will be enough to control your thyroid.
While it may be enough to keep your lab tests in the normal range, it may not be sufficient to keep you at an “optimal” level.
Because of this, it’s not uncommon for patients, post-thyroidectomy, to experience side effects such as weight gain (on average 10-20 pounds), depression, hair loss, and so on (4).
We will discuss these topics in detail below, but for now, just realize that they do exist and they may be a “complication” that some patients experience.
But back to thyroidectomy basics for a minute…
The term thyroidectomy is the name of the procedure which is used to describe the surgical operation that completely removes the thyroid gland from your body.
The surgical procedure itself is fairly straightforward provided you have a good surgeon doing the operation.
There are a few potential side effects related to the surgical procedure itself (such as damage to certain nerves or the potential for the removal of your parathyroid glands) but most people do not have issues with these.
Instead, the complications tend to come afterward when thyroid hormone replacement is initiated.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Who should get a Thyroidectomy?
Thyroidectomy is often recommended for patients who suffer from diseases that cause hyperthyroidism.
Conditions such as Graves’ disease or toxic multinodular goiter are common diseases that may warrant the removal of your thyroid gland.
Patients who have hyperthyroidism may have alternate options, instead of getting a thyroidectomy, such as taking anti-thyroid medications or radioactive iodine ablation.
Some other disease states, such as thyroid cancer, do not leave many options in terms of treatment.
Patients with thyroid cancer should undergo a thyroidectomy because, in most cases, it allows for the complete removal of cancer cells in your body.
Some other conditions such as goiter (enlargement of the thyroid gland) or multiple nodules may also warrant a thyroidectomy, but these are not as common as the other disease states listed above.
The main idea here is that you don’t want to get a thyroidectomy unless it is absolutely necessary for your body.
If you have other options, such as the use of medications, it may be wise to consider these therapies prior to getting a thyroidectomy.
Occasionally, thyroidectomy is recommended as a surgical option for treating hyperthyroidism simply because it is felt to be easier to manage hypothyroidism with medication as opposed to hyperthyroidism.
This may work for some people, but for many others taking out their thyroid prematurely may cause more harm than good.
As always, this should be evaluated on a case-by-case basis.
Thyroidectomy Recovery & Side Effects
What can you expect in terms of recovery after your thyroidectomy?
The first thing to realize is that after your thyroid is removed you will be reliant upon thyroid medication for the rest of your life.
Once your thyroid is removed your body is no longer capable of producing thyroid hormone in any real capacity.
This means that you must supplement with thyroid hormone replacement medications such as levothyroxine and Synthroid, for the rest of your life.
And this is incredibly important because the lack of thyroid hormone can lead to mix-edema coma and even death.
This is something that you should discuss with your Doctor prior to your procedure.
In terms of surgical recovery, most patients recover very quickly.
Patients are usually back at work within 2 weeks and pain from the operation is usually gone within 2-3 months.

This surgical recovery is usually not an issue when compared to the thyroid hormone effects of the procedure, which tend to be long-lasting.
Remember:
Once your thyroid is removed you will be on thyroid medication for the rest of your life.
But what does this mean for you?
It means you will need to take thyroid medication each morning and you will need to evaluate your blood work every 6-12 weeks to make sure you are getting sufficient thyroid hormone replacement.
Negative side effects related to thyroidectomy tend to occur due to problems with thyroid hormone replacement.
The issue here is that most Doctors take a very standardized approach to thyroid hormone replacement.
They tend to treat with Synthroid or Levothyroxine and adjust dosing based on the TSH.
This is the conventional thought and way of treatment, but more recent studies have come out which show that optimizing thyroid treatment based on the TSH alone may cause low free thyroid hormone concentrations in the serum.
This low free thyroid hormone concentration in the serum may be one of the causes of depression, weight gain, hair loss, fatigue, and so on that many patient’s experience after the procedure.
If you go into your procedure overweight then you are much more likely to gain weight after the procedure.
If you are at a normal weight going into the procedure then you have a much lower risk of gaining weight afterward.
The good news is that optimizing your thyroid medication may be the first step in treating this issue (more on that below).
Complications Related to the Surgical Operation
While most patients who undergo thyroidectomy will not suffer any long-term side effects related to the operation, some patients may experience 1 of 2 major problems.
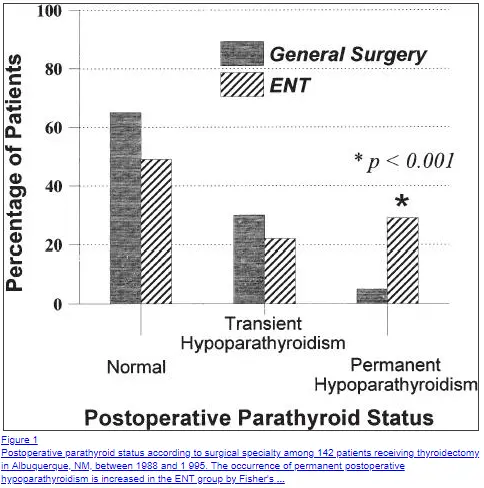
The first has to do with the accidental removal of your parathyroid glands.
Your parathyroid glands (4 of them) sit on the lobes of your thyroid gland and they are very tiny and sometimes “stuck” to the thyroid capsule.
Your surgeon is very aware that they exist and will do his/her best to try not to damage or remove them.
But occasionally, they can be removed by accident or perhaps out of necessity if they are compromised due to cancer or some other issue.
Permanent damage to the parathyroid gland occurs at a rate of about 1.9% of all patients who undergo this procedure (6) (making it rare).
Once removed your body will no longer be able to adequately regulate serum calcium levels on its own.
This usually results in VERY low calcium levels after surgery which may cause side effects such as tetany, which is the involuntary contraction of muscles in your body.
The removal of your parathyroid glands may cause chronically low calcium and/or high phosphorus levels in your serum after your procedure.
Most patients who experience this issue will be placed on calcium tablets or pills and will need close monitoring of their calcium levels with each routine blood test.
Another, less common complication, is that of damage to the recurrent laryngeal nerve during your operation (7).
This complication arises in about 1.5 to 14% of all thyroidectomy surgeries (8) (depending on the study you look at).
Injury to this nerve may cause a weakened voice or hoarseness to the voice.
In some cases, it may also result in complete loss of your voice or other issues.
This complication is very important, especially if you rely on your voice for your career (such as singers/voice actors/etc.).
Even small damage may reduce or alter the tone or pitch of your voice.
As always your surgeon will do his/her best to avoid damaging this nerve, but sometimes damage occurs despite their best efforts.
These side effects tend to be rare (occurring anywhere from 1-10% of the time) but should always be considered prior to getting your operation.
Weight Gain after Thyroidectomy
One of the most common issues that thyroidectomy patients deal with is the issue of weight gain after their procedure.
As I mentioned previously, it is common for most patients to experience some weight gain after their thyroidectomy.
This weight gain is often dismissed by the doctor or specialist who insists that the thyroid is not the cause of the weight gain, but it’s hard to believe when we know that your thyroid controls up to 60% of your metabolism (9) (or basal metabolic rate).
This weight gain after the procedure is often the result of low T3 levels secondary to taking T4-only thyroid medication such as Levothyroxine and Synthroid.
Some patients, due to a variety of reasons, have trouble taking T4 and converting it into T3 through the conversion process.
This problem may be masked or hidden while they have a thyroid (due to the body naturally compensating), but it may be unmasked after the thyroid is removed.
There is a subset of patients, around 15% of all patients (10), who have issues with converting T4 into T3.
These patients tend to not be as responsive to thyroid medications such as Levothyroxine and Synthroid and may do better on combination medications which include both T3 and T4.
In many cases, switching to a combination medication such as NDT (Armour thyroid, WP Thyroid or Nature-Throid) or adding T3 (liothyronine and/or Cytomel) may be sufficient to help with weight gain after the procedure.
For weight loss, focus on your serum total T3 and free T3 levels which have been shown to correlate with weight loss.
Do you Have to get a Thyroidectomy?
After reading this post you may be asking yourself:
Do I really need to get a thyroidectomy?
The answer really depends on your situation and why it was recommended in the first place.
Patients with difficult-to-treat hyperthyroidism (those not responsive to medications or RAI) and those with thyroid cancer may not have a choice.
But if you are suffering from Graves’ disease or another cause of hyperthyroidism and you are currently managed on medication, it may not be the best option for you.
Make sure you discuss your options with your current physician or surgeon before you undergo the operation.
In some cases, you may be able to impact your thyroid status by changing your lifestyle or integrating certain alternative medical therapies.
These therapies are not always effective, but they are worth a try prior to getting your thyroid removed.
You can explore the various conventional and natural therapies used to treat hyperthyroidism here.
Final Thoughts
If you’ve recently undergone a thyroidectomy, or if you are thinking about it, make sure that you consider all options available to you before you undergo the procedure.
Removing your thyroid gland is a relatively easy procedure from a surgical standpoint, but it may cause long-term issues as you try to juggle your thyroid hormone levels with thyroid medication.
In general, most patients benefit from the combination of T4 + T3 thyroid medications.
You can get this benefit by either adding T3 to your existing dose of medication or by switching medications to Natural Desiccated Thyroid hormone.
Using T3 may be enough to help reduce depression, help with weight loss, improve your energy and help you feel more like yourself.
Now I want to hear from you:
Are you struggling after your thyroidectomy?
Are you experiencing negative side effects?
Have you been able to manage your symptoms with certain therapies?
Is your Doctor willing to work with you?
Leave your comments below so we can share the knowledge with others who are in a similar situation!



I am at a loss where to get me a doctor that understands thyroid in Ohio. I had Graves Disease, and my Dr. said I would die if I did not drink the radiation drink that destroyed almost all of my thyroid. Then I read this year it only lasts an average of 15-18 years and then clears up. He did not tell me that. I’d rather take hormone to decrease it than to deal with what I do not. He only wants to go by the TSH. I have never felt good again and am 115 pounds heavier. I gained 65 a few years ago when he reduced my medication 2 levels in 8 months and then about 9 more. I was up set and he said I did not understand it and never will, but I argued I know how I feel and being so tired you just sit and fall asleep all the time and all my hair is falling out. I also seem to have a bloated stomach. He retired and the next Doctor started and he reduced it to .100 mcg. It was 125. I believe that’s 2 more lower. I am so upset and depressed. I cry all the time and know summer is coming and I am started a pound already in one week. There is a End can’t remember the rest specialist they want to send me to. The go by the TSH too. What am I to do and What type of Doctor should I be looking for. I feel awful and have every since this started years ago. I would have been just about over it by now and instead feel worse than ever and so tired. I have no energy whatsoever. Please help me, I don’t know where to turn, I’ll have to go further away to where they have better Doctors buy I don’t think they seem to care much any more. I’m over 55 and past the menopause that was horrible on me. But am worse feeling I have ever felt in my whole life. I can watch the weight go on. If I eat anything at all I gain weight. I try to eat next to nothing. I did have almost nothing buy vitamins for 2 months and breakfast drink for 2 months and still only lost 10 lbs. and soon as I ate they came right back with a couple more. I am ready to stop eating altogether. I don’t know what else to do and am over the 200 mark now. I hate myself and very upset with the Doctor that put me through this. I am allergic to more medications than I can take due to every side effect you can get and then some extra on some. I have Fibromyalgia on top of some chronic pains. I have Osteo- arthritis. One knee replaced, 3 bulging disks and some other thing sticking out. Deteriorating disks in my neck, 4 in T8-T9, L3-L4. Perminant damage to my sciatica nerve in my left leg. A foot operation for a very sensitive place on my foot, ended up screws came out and replaced but I swear my Big toe in not attached it just bounces up and down. It made it worse not better and I was told I had so many blood clots in my lungs, I could only say about 2-3 words at a time. I kept telling the Doctor for 3 weeks I was getting so out of breath. My leg had a cramp in it and I said can I at least try and stretch out my leg it has a constant charlie horse in it. He never once said anything about me having a blood clot. I even ask him and he said I’d have a fever. So I called my regular Dr. and told him I couldn’t breath and should I get an x-ray or something. It took like 5 more days to hear there was nothing there and he made me drive 15 miles back when I asked if there was any other test I could take, I had my Mother there for a test anyway. The nurse told me to call from there, because something was bad wrong with me. I told her I couldn’t breathe. I went to the office and was told, I don’t know how you are walking around. There were a large one in each lung and so many others they couldn’t count them. I had a big one behind my left leg and several still in my legs. He said to go back to the hospital for a lung scan and to stay there and not leave without talking to him. I didn’t get to go home. Said I lived through what I should have died from, will take care and disolve the rest at the hospital. Then I took Coudimin for 6 months afterward. I never did get where I could breathe again. He said I needed arobic exercise. I asked how I was to do that with a bummed up shoulder from a fall. And just went through surgery twice on my foot. I hurt from head to my toes. If I woke up and didn’t hurt I’d think I’d died. I dream about the areas hurting in my sleep. They say I have sleep apnea, and not COPD but allergic to the medicine. I have low blood pressure and it went sky high, my face was all red and swollen, my pain mgmt doctor made me call my lung doctor. I told her I am allergic to Predisone, but she was hoping going right into the lungs it would not give me as many side effects. It took 8 days to get it down to 83 on the bottom. What am I to do. I don’t like a lot of foods and never have been a big eater and taken vitamins my whole life because I was anemic 3 times when in my teens. I have taken them since. I think the blood clots damaged my lungs. My Doctor when that happened to me he took off to another State. I seen another Dr. in his office and my step is not right now. The bone under my big toe and right in the middle take all the blunt of walking and has a big callus under my big toe. One leg and one foot hurts to walk, but I do anyway. I am in pain all the time. I will not take higher than the lowest dose of pain medication because there are 21 pain medications I can’t take. Nsaids made a sore in the base of my esophagus. Ended up with gerds and got a hyena-hernia. I seen where you had a diet, I do terrible with them. I also have IBS and my stomach if I don’t even like the smell of something I will get sick at my stomach. I’s rather not eat at all. I am about to that point. What kind of Doctor should I see. And then I am going to call and ask what they base their determination on. Please help me. I’m begging for something. Your information sound very close to what I am dealing with. If you have almost no thyroid why is it such a mess to determine what you need. I also was told if the TSH was to high it was because it was to low because one of the other Free T’s wasn’t right. Because there isn’t anything to work with it try to make a lot the effects the TSH. Is there any truth to that?
Hi Tina,
It seems like you may do better seeking out a second opinion or seeking out a physician who specializes in thyroid management. I’ve put together a resource which can help you here: https://www.restartmed.com/thyroid-doctor/
In terms of your question, the TSH will drop based on the dose of medication that you use. A high TSH, if you are using medication, is usually an indication that your dose is too low. This may or may not be indicative of a problem with free thyroid hormones.
Wow! Your journey has been an obstacle I feel for you deeply….Wake up and say I am stronger than this and take it a day at a time! Sometimes the answer is not a doctor but a team of them working together for your treatment…and remember new technology new research may change what a Dr. Has previously learned and Sometimes we as patients must pose tough questions to them for a healthier lofe….I suggest as a graves disease warrior as they say to take up some loght yoga swim therapy adjust your diet and vitimin intake and then get tests, as for the pain your in remember every pill you take has a boat of side effects and sometimes the chemicals in your system from different medications cause ailments too…be safe
Dr.
I had a total thyroidectomy
I’m told I have Hashimoto…
Surgery was 3 yrs ago. First 21/2 years I did great on Armour… lost weight and had good energy. I also have a cervical fusion around the same time and took hydrocodone for pain. Plus low back issues. Tried to get off the pain pills and took a natural pain med called Kratom…. apparently, the Kratom caused the Armor to not work. My TSH jumped to 16….. gained 20 pounds, no energy, major depression
I believe my t4 is not converting to t3…
I have ordered your reset formula. And t3 formula.
Can you tell me the best way to take these formulas? I currently take 120 mg of Armour. Dr raised from 90 to 120. But I don’t feel any better. Nails are short and peeling off. I’m getting my blood work done again this Monday 26th.
I’m thinking I should ask for Cytomel???
Please help with any advice
Carolyn Lewis
Hi Carolyn,
You can find the best way to take your supplements in the FAQ section on the product page of all of the supplements which you have purchased (on those pages I discuss how long they should be taken and how exactly to take them):
Information on how to take Thyroid Adrenal Reset Complex: https://www.restartmed.com/product/thyroid-adrenal-reset-complex/
Information on how to take T3 Conversion Booster: https://www.restartmed.com/product/t3-conversion-booster/
I am almost 66 years old and had a total thyroidectomy in December of 2016. Generally speaking, I have done quite well. I am wondering though if these issues might be related to the surgery. First, I am experiencing a very significant reduced libido. Secondly, I am very forgetful “in the moment.” I sometimes totally forget that certain events, conversations, etc. ever occurred. I occasionally do weird things like picking up a cap from a water bottle and rather than putting it on the bottle, will start to put it on a milk bottle nearby. Also, I considered myself to be pretty articulate and have always been very comfortable speaking in front of large audiences. Now I find that “losing words” is somewhat common. I know these symptoms can be related to the aging process, to dementia, etc. What I would like to know though, is whether or not there is evidence of these things occurring as a result of a thyroidectomy. Frankly, I hope so, because that would be a whole lot better than dementia. I’d appreciate your thoughts.
Since the thyroid is key to hormone regulation, potential for effect on libido is very real.
100%. Thyroid dysfunction can and does impact libido.
Thank you for your article on having a thyroid removed. Mine was removed due to nodules that surrounded the gland and the biopsy seemed ‘suspicious’. In time it was determined that the nodules were benign. However my weight gain is almost 100 lbs., I have many issues that may or may not be related to this surgery: ie. fibromyalgia, sleep apnea. R/A, Neuropathy, Type 2 Diabetes, Pituitary Adenoma, 30% kidney use (nephritis since the early 70’s) and I am currently 70 years young. I am on 14 medications and I believe that my doctors no longer ‘see’ me. I want to make some changes but have no idea how to find a physician who does not tell me I am a ‘challenge’. I know you are no longer accepting new patients and do not give out recommendations however any new research, clinical trials or medications that can help those of us who have many ‘challenges’ with their issues would be very helpful. Thank you for the work you do!
Hi Barbara,
I’m glad you find the information helpful! Currently, I’m not sure that I have any new research (aside from what is already cited on my site) that I haven’t discussed as of late. I will keep an eye out though and post anything new. You are probably right though about your current situation. Once patients get on 10+ medications, management becomes more about medication management and side effect management than disease management. It’s very unfortunate but that is the current state of conventional care it seems.
Hi I’m 26 and got my thyroid removed 10 days ago due to thyroid cancer.I stayed in the hospital for a total of 5 days since my calcium levels are so low.Im still taking calcium and magnesium calcitrol and levothyroxine 88 mcg. I’ve been feeling really sensitive and cry easily. Extremely tired in the mornings and it’s hard for me to sleep at night I end up going to sleep at 2 or 3 am every night. I was always very active and now it’s hard to even think of making breakfast for my toddler everything just makes me so tired. I have also been feeling bloated. I weigh 120 and I’m 5’3 and I just look pregnant. I’m starting to think I’m going crazy are these symptoms normal? are they going to go away soon? Is it my medication ? This was just never discussed with me prior to surgery.
Hi Ana,
I wouldn’t say they are normal but they are not necessarily unexpected either. They should resolve once you get your medication in order.
I am 6 weeks out from my total thyroidectomy, due to cancer. I’m 52 and a pre k teacher. I still have numbness under my chin area. It feels like I’m wearing a choker 24-7. I’m also a singer. I’m experiencing no energy, no patience, and weight gain. I do not feel like myself at all ever since the surgery. I have no volume in my voice, so teaching is a real challenge. I feel so sad and alone.
Hi Twana,
All of those symptoms likely stem from hypothyroidism, make sure you go back to your Doctor and have them assess your thyroid function and make changes as necessary!
I had a thyroidectomy over a year ago. With every increase in Synthroid, there is another problem. It has been a constant battle with muscle and joint pain, neuropathy in my feet, tendonitis symptoms. My TSH has bounced from 19.5 to .4 to currently 8. Muscles in my back feel as if they are on fire, I cannot stand for more than 5-10 minutes without the pain and burning. MRI has been done on my back, neck and brain with only light arthritis showing. Is it possible that Synthroid is just not right for me? I’m only 46 years old. I shouldn’t feel like I’m 70.
Ho Susie,
Yes, it is very possible you don’t do well on Synthroid as monotherapy. I would at least consider the possibility of adding Cytomel and switching to Tirosint. You can read more about chronic pain and muscle pain in hypothyroidism here: https://www.restartmed.com/hypothyroidism-chronic-pain/
I feel horrible after the removal of my thyroid and have gone to 2 different doctors and explained to them with no understanding or help.
Hi Tina,
I would recommend you check out this article which may help you understand your situation better: https://www.restartmed.com/normal-thyroid-levels/
I recently (6 weeks ago) had my thyroid removed due to a cancerous nodule. The surgery went well as has recuperation. I
have noticed that I’ve put on about six pounds and that I am hungry much more than I used to be. I don’t exercise much because I have trouble with my knees/legs, but I ride a bike on a simi-regular basis. I just learned about weight gain as my doctor didn’t mention it. I am now very concerned. Should I restrict calories or check T3 levels on a regular basis? What else can I do? I am just about 67 years old and in otherwise good health.
Hi Crystal,
You can find more information on how to lose weight after thyroidectomy here: https://www.restartmed.com/weight-loss-thyroidectomy/
Should one bother looking at TSH if thyroidless?
I had a thyroidectomy 16 years ago and I have tried every possible medication and combination. I’m currently on 3 grains of Nature-throid. My free T3 is 2.5 and Free T4 .58. My TSH is <.01. Thinking I may need to increase my dose a bit, but my NP is freaked out because she just had a male patient on 3 grains who had a heart attack (she claims due to high dose). She now says my dose is too high and I should be concerned about my bones and heart. Any thoughts? Thank you!
Hi Jennifer,
You never would want to completely ignore the TSH, but it may not be the best lab test to evaluate thyroid function. You can learn more about the potential dangers of TSH suppression here: https://www.restartmed.com/suppressed-tsh/
I had stage 4 thyroid cancer in 1998. The cancer had spread to my lungs, bones, breast and lymphnodes. Right after my thyroid surgery I gained 85 pounds within 6 months. I have been on Levothryoxine since the surgery. I am not able to lose weight, it is a daily battle. I don’t get hungry, and I have to force myself to eat. I can get up in the morning, and still feel full from the dinner the night before. I know the doctors tell me I have to eat, and I do try to eat small meals through out the day. I have seen two Endos and they both tell me that I should have gastric bypass surgery, because I am obviously binging. My husband is very supportive and has explained to them, that I am not. Any thoughts on how to get help?
Hi Tiffany,
What you are experiencing is a mismatch between your physicians understanding of physiology and what happens in reality after thyroidectomy. Most endocrinologists do not believe that your thyroid has anything to do with weight or metabolism even though physiologically it is proven that they do. Much of this has to do with the current thyroid treatment paradigm which focuses entirely on the TSH and on T4 medication. It’s not until you get on T3 medication that you will probably notice an improvement.
Cancer, total thyroidectomy at Hershey, PA. Was told afterwards, it probably could have been monitored, rather than removed. But when one hears CANCER? You do what they suggest. I would still make the same decision today.
They put me on Synthroid..112 micrograms; I augment that daily, so I’m probably up to nearly 130. I can’t function at less than that. I’ve been prescribed 75 of Armour. We’ll see how that goes. I have job that requires my cognitive abilities; I can’t be compromised there.This entire scenario was caused by an HMO doctor not doing his job.
Maybe you could do more writing on this topic. I could not function following my surgery. Finding a hormone combination that minimizes my symptoms that also produces measurable TSH and in range FT3 and FT4 seems to be impossible. I have tried lots of things. Armour works but 60mg is too low (TSH 5) and 75mg is to much.(TSH close to zero). I weigh 170 lbs.
Replacing thyroid hormone following a thyroidectomy or RAI is anything but simple. Doctors need to be honest with patients about this. Is anyone doing research on how to best treat thyroidectomy patients?
Hi MJ,
Sure, I’ll add it to the list of topics to write about. And, unfortunately, no one is doing research on this particular topic because as far as most physicians are concerned the issue has been solved a long time ago (even though obviously a great many people still suffer). This is an issue with the current treatment paradigm and the unfortunate reality of many patients who do seem to fit into this paradigm and it sounds like you are one of those.
Hi-
I had a total thyroidectomy from cancer almost 3 years ago and my TSh has been <than than the lowest range the whole time. Currently, it is 0.02. I am 39 years old and up until this was relatively healthy. I am on my 3rd endocrinologist as the first two just kept decreasing my meds every 2 months and I would go through extreme roller coaster of symptoms. This third doctor has absolutely no bedside manner bust supposedly is a detective and said she thinks it is abnormal it has taken this long to get my blood normal. She decreased my dosage to 6 days a week I take .88mcg on the 7th day I take have a pill. I also take 5mg of cytomel. In the last month I have felt crazy. I feel deep depression, insane irritability and just extreme emotions. I am freezing all the time and I have the worst foggy brain to the point I can't remember simple words like dresser and end up calling everything a container. It is getting to be a challenge at my job. I am so frustrated and so tired and the thought of yet again starting over with a 4th endocrinologist makes me want to give up. I also continue to have a high cancer marker. My T3 and T4 are in range. Nobody will explain what this all means in connection to each other and I really just want to feel like a normal human. I am so open to any suggestions. This week I waited for 30 minutes in the waiting room past my End appointment time, to have her open 2 minutes in the room with me READING my chart. Then she said go get blood work and you're due for another ultrasound and left. I typically advocate for myself well but I am just not feeling like myself the last month and just couldn't do it. I appreciate you taking the time to read this. I am lost and need help.
Hi T,
Unfortunately, as long as physicians treat based off of the TSH then you can expect this type of roller coaster of symptoms and side effects. A better way is to focus on free thyroid hormones and use a combination of both T4 and T3 thyroid medications. In order to get this type of help, you will most likely need to seek out a knowledgeable physician. You can learn more about how to do that here: https://www.restartmed.com/thyroid-doctor/
mlb0312@hotmail.com
I had a thyroidectomy in 2014 due to Thyroid cancer. I’ve gained 10 to 15 lbs. I was put on Synthroid 88mcg. It was then increased to 100 mcg. For about 6 weeks. Increased to 125 mcg. I felt at my worst on that dose. Doctor reduced my dose to 100 mcg again. During that time only my TSH was tested. In 2017 I told my doctor i wanted him to reduce my Synthroid and add Cytomel. He did. We checked labs every 6 weeks. He lowered my Synthroid every 6 weeks and kept my Cytomel the same. I felt better but no weight loss. My last dosage on Synthroid was 75 mcg 5x a week and Cytomel 5mcg twice a day. On this cocktail, my labs taken on 2/11/19:
TSH: 0.165 uIU/ml
T4free: 1.25ng/dl
T3 total: 129 ng/ dl
Forward to present, I started taking Armour Thyroid 90mg March 1, 2019. Resent labs taken 4/2/19
TSH: 0.0051uIU/mL
T4 free: 1.11ng/dl
T3 total 145 ng/dl
My doctor wants to lower my Armour prescription. I am afraid that lowering my prescription would be too low. The T3 total seams to be at optimal. Don’t think my T4free is at optimal. Why is the TSH so low? Should my doctor be ordering other tests?
Thanks,
Myrna
Hi Dr. Childs, I was diagnosed with Grave’s Disease and Hyperthyroidism 2 years ago. According to my labs, I had elevated blood calcium for about 4 years and had developed proptosis from the Grave’s disease. I spent 17 months taking PTU to lower my thyroid levels and my weight consistently went up each month. They were never able to get my thyroid levels consistently into the correct zone. They eventually recommended a thyroidectomy and after an ultrasound, noticed I had a tumor on one of my parathyroid glands. Three months ago, Feb 2019, I had a complete thyroidectomy along with the removal of the tumor and one parathyroid gland. Immediately following the surgery, I no longer had a hyperthyroid nor elevated calcium and was put on 125mg of Levothyroxine. I gained another 10 lbs and was exhausted all the time. A month ago, they raised the levothyroxine dose to 150mg . I have taken 150 mg of Wellbutrin SR for many years as depression runs in my family. I feel a little better because I started taking 18mg of phentermine so I am not so exhausted all the time. I currently need to lose 45 lbs. I used to be an avid runner and have started exercising again. I am interested in intermittent fasting. I would like to figure out the correct medication and supplements that would best suit my situation and make it possible to get back to a healthy weight. I would love to meet with you if you are considering new patients. Any recommendations would be greatly appreciated.
Good afternoon,
I removed my thyroid and parathyroids plus lymph nodes in 2012. I Did RAI in 2013 and 2014. My doctor sends me for blood tests every 4 months and I have been changing my Synthroid according to the needs. Everything went well for a while but since 2017 it is been quite a roller coaster with my levels changing a lot every 3 months not even going for 4 months. I know something is happening because my heart tells me something is not right. Currently, I take only 1mg Synthroid after a reduction from two different doses per week ( 112 3 days and 1 mg 4 days) and my doctor is been decreasing the dose since 2017.
I am 63 years old., very fit, not overweight ( 1.64 meters /67kgs )
I still work full time, drive etc. and feel lots of energy and love to work. However, I get frustrated because my heart keeps fluttering and either my pulse is at 48 ( regular is 54) and can jump to 130 in minutes. And after keeps fluttering for a while even when I take aspirin. I can get dizzy and I get very cold all of a sudden. My back my hands and legs get really cold. Today I took two aspirins ( 1 blue and one 300 mg ) and took almost 3 hours to get to regular. I was at work. It is like I am in a race. After I worked my regular day but I got home exhausted. When my Doctor decreases the dose I feel good but coming to the third month I started feeling it again and I go and do my blood tests and go to Endo and he decreases the dose. I feel good again for two months or so and again… I did Blood tests on Friday and the Result was TSH 0.34 ( which is high according to my doctor) and Free T4 – 17 and Free T3 – 5. and both are high for my condition. I am sure my endo will change again the medication. What should I do to avoid my heart from fluttering so much. ( I don’t have diabetes or High Cholesterol and normal BP is 117/77 – usually toward low sometimes diastolic can be 80 or even 85 which I was told can be considered high.
which is also high. )
Thank you for the opportunity to submit my experiences with you.
Kind regards
I was only 18 years old when I was told I needed to have a thyroidectomy due to 2 thyroid storms I had. My endocrinologist and surgeon both failed to inform me that I would need to take medications for the rest of my life. I almost went into a coma because I didn’t take any thyroid med for months after the surgery. I thought it would be like removing my appendix or gallbladder “no major side effects” boy was I wrong! I developed severe anxiety and depression, every doctor kept telling me I had psychiatric issues and put me on anti depressants. I never felt like myself and I got a lot of negative side effects including suicidal thoughts. I was losing my mind while taking the anti depressants (SSRIs) and Levothyroxine. 7 years later I confronted my endocrinologist (a different one than the one who failed to inform me what my life would be like after his idiotic recommendation) and I demanded for a natural alternative. He prescribed Armour Thyroid, of course he was not happy about it and tried talking me out of it. I was so desperate I didn’t care what the side effects were, I wanted some relief. Funny enough, all “psychiatric” symptoms disappeared magically after stopping the Levothyroxine. I quit the anti depressants 5-6 years ago and suffered with anxiety until I switched my medication. I never found “life after a thyroidectomy” articles or books because they blame life for depression and anxiety without looking at thyroid issues. I’m just glad I switched to Armour Thyroid and will never switch to a synthetic medication.
I have two nodules on my left thyroid, one is 4.78 cm and the other is 1.47. The specialist told me today that he could take out just the left side of the thyroid. He said the right side is fine. After reading everything here I am concerned about weight gain after but he said the side with the nodules has to come out. Is it a good idea to leave the other right side of the thyroid or should I just have it removed at the same time.
Hi Sharon,
I would highly recommend keeping whatever fraction of your thyroid you can. Many people regret removing their thyroid gland because it’s never as easy to manage as your doctor makes it sound.
Last year (October 2021), I had a partial thyroidectomy due to a very large nodule they thought was cancerous, but turned out not to be. At that time, I was physically in the best shape of my life thanks to counting macros and strength training.
Since then, I have gained 20 lbs. I started T4/T3 meds (Tirosint/Liothyronine) in February, but it seems no matter how high or low my meds are (even being in optimal range for thyroid and iron labs), I’m having all the hypothyroid symptoms (ie. Weight gain, hair loss, brittle nails, slow digestion). Since August, I’ve been struggling with air hunger and in the past week, it has become so bad, I can hardly stand it. I’m constantly gasping for air!
I’m just so unsure what to do bc I feel like I’ve tried all the diets, supplements, treatments, med dosages, etc. and things are continuing to worsen.
I’m a 38 y/o mom of 4 and want to be able to run around with my kiddos again and focus on them, rather than my health issues all the time.
Reading many of your articles, I thought adding T3 would solve most of these issues for me, but it hasn’t.
Is there any way to get your opinion on what may be going on with me and what I can do to get back to feeling like myself again?
Hi Melissa,
I’m not seeing patients but if that ever changes I will send out an email to my mailing list! In the meantime, you can use this resource to help you find someone: https://www.restartmed.com/how-to-find-a-doctor-to-treat-your-thyroid/