It’s estimated that at least 70% of Americans take at least one prescription medication and that up to 20% of Americans take five or more medications (1).
We know, if you read this blog, that up to 15% of patients in the United States also take thyroid hormone (2) (a prescription medication) for thyroid disease.
When you start crunching these numbers it’s easy to see that there is likely considerable overlap between those taking thyroid hormone and those taking other thyroid medications.
What may surprise you is that many of these common medications may be silently interfering with your thyroid function or your thyroid medication.

What that means is that certain prescription medications, while they may be helpful for various conditions, can also reduce the amount and function of circulating thyroid hormone in your body.
And medications aren’t the only things to interfere with your thyroid medication either, even some supplements (such as calcium) can bind to and inactivate the thyroid hormone when you ingest it.
These two factors combined make it very important for you to understand the basics of thyroid function and the impact prescription medications have on it.
Ever wonder why your doctor and pharmacist give you “special instructions” on how to take your thyroid hormone medication?
They are trying to give you tips to help you increase the amount of thyroid hormone that you absorb.
Remember:
Taking thyroid hormone by mouth doesn’t automatically ensure that it will get into your body and into your cells.
In order for that to happen, it must be absorbed by your intestinal tract and then activated by your cells.
With this in mind let’s talk about some of these medications:
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Medications that Interfere with Thyroid Function (Make your Thyroid Worse)
Because thyroid physiology is quite complex so too is the way that prescription medications can interfere with thyroid function.
We can break it down into three major sections to make it easier to digest.
All of these sections represent ways that prescription medications can interfere with how thyroid hormone operates and functions in your body.
#1. The first way that medications can impact thyroid function has to do with a process known as T4 to T3 conversion.
T4 to T3 conversion is an important process in terms of thyroid physiology because it is this process that activates your thyroid hormone.
Any medication that blunts this process will result in DECREASED T3 levels in your serum and decreased thyroid function in the entire body.
Only a handful of medications fit into this class, and they are commonly used to treat a condition known as hyperthyroidism.
Hyperthyroidism is a condition that results in TOO MUCH thyroid hormone so it makes sense that the treatment for this condition would be to slow down thyroid hormone activity.
Medications that fit into this category include:
- Methimazole – These medications are used to treat hyperthyroidism but using them in your body can create a hypothyroid environment which may lead to the symptoms of hypothyroidism and lead to weight gain. It’s also important to realize that this medication blocks the release of thyroid hormone from your thyroid gland.
- PTU or Propylthiouracil (3) – Like Methimazole, PTU also blocks the release of thyroid hormone from your thyroid gland.
- Beta Blockers (Propranolol) (4) – Beta blockers are commonly used in hyperthyroid patients to reduce anxiety, heart rate, and tremors. But this class of medication is also commonly used to treat high blood pressure in people without thyroid issues.
In most cases, you will know if you are taking these medications and you will most likely feel that they are interfering with thyroid function in your body.
The exception may be beta blockers which are commonly used to treat high blood pressure.
Beta-blockers are known to cause other issues such as erectile dysfunction and depression which may be linked back to their impact on thyroid conversion.
#2. Medications can also interfere with your thyroid by altering your ability to produce TSH.
TSH is the stimulating prohormone produced by your pituitary gland which signals to your body that you need to produce more thyroid hormone.
TSH circulates from your brain where it interacts directly with your thyroid gland and “stimulates” the release of thyroid hormone.
If a medication alters your TSH level (either up or down) this will directly influence how much thyroid hormone you can produce.
These medications can complicate your clinical picture and make determining how to proceed with thyroid dosing difficult.
Medications that are known to lower your TSH include:
- Glucocorticoids (5) (which includes steroids such as prednisone) – Frequently used to treat inflammatory conditions and autoimmune diseases.
- Dopamine agonists – Often used to treat Parkinson’s disease.
- Somatostatin analogs (6) – Used in rare forms of cancer to block hormone production.
- Metformin (7) – Used to treat insulin resistance and type II diabetes mellitus.
The two biggest medications in this group include metformin and steroids because they are very commonly prescribed.
The other medication classes, while still important, are not quite as common.
Metformin is commonly used to treat insulin resistance and high blood sugar and can also be used in weight loss regimens (you can read more about that here).
Steroids, on the other hand, are frequently used to treat autoimmune diseases or inflammation “flare-ups”.
Just realize that using steroids in this way may be beneficial for inflammation but may be causing damage to your thyroid gland in the process.
You may be able to forgo using steroids to reduce inflammation by focusing on more natural ways to reduce inflammation such as diet and other supplements like Fish oil or Curcumin.
#3. The last way that medications can impact thyroid function is by reducing the amount of hormone that you produce from your thyroid gland.
Obviously, if you reduce the amount of thyroid hormone that your body can produce then you may experience the symptoms of hypothyroidism!
These medications act to directly block or inhibit the secretion of T4 and T3 directly from the thyroid gland.
Remember:
TSH is required to “stimulate” the release of thyroid hormone from your thyroid gland, but, even if TSH levels are normal, your thyroid gland must still be able to produce thyroid hormone in order for it to get out and function.
Medications that fit this category include:
- Lithium (8) – Used to treat bipolar disorder.
- Iodide (9) – Used to treat skin-related disorders and to kill off certain bugs.
- Amiodarone (10) – Used to treat certain heart rhythm disorders.
Most people know if they take these medications, that their thyroid may be in jeopardy as it is considered the standard of care to evaluate thyroid function every few weeks while taking them.
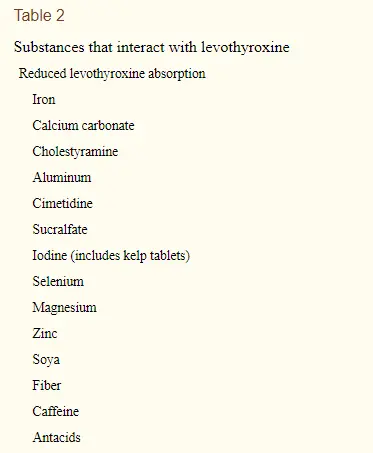
Supplements That Interfere with Thyroid Function if You Are Taking Thyroid Hormone
Even if you aren’t taking any of the medications listed above, you still may not be out of the woods yet!
It turns out that many other factors, including the supplements that you take by mouth, can also interfere with your body’s ability to absorb thyroid medication (and this applies to all types of thyroid medications).
Remember:
Most hypothyroid patients take a medication that contains T4 such as Levothyroxine or Synthroid.
These medications are notorious for being difficult to break down and absorb by hypothyroid patients.
For these reasons, you may have been given certain instructions on how to take them.
This includes the time of day that you take them and instructions to not take them with food or water.
It turns out that these recommendations are important, but let’s also talk about other factors that impact thyroid hormone absorption:
- The time of day that you take your medication – Most thyroid patients are instructed to take their medication first thing in the morning. While this may work for some people it has been shown in some studies that taking your medication at night actually increases absorption (11). This has to do with the fact that your intestinal activity is increased in the morning which may “push” your medication through your intestines too quickly. You can read more about this idea here.
- Taking your medication with food (12) – It’s generally advised to take your thyroid hormone away from meals. This has to do with the fact that absorbing thyroid medication is reduced if taken with meals. As long as you take your medication 1-2 hours after eating you should be good to do.
- Iron – Iron, if taken at the same time as thyroid hormone, can also dramatically reduce absorption levels. Many patients, especially those with Hashimoto’s, suffer from both iron deficiency and hypothyroidism. If you fall into this category try to take your thyroid medication at the opposite time of day as your iron. This can be bypassed by taking liquid levothyroxine (13).
- Cholestyramine (14) – This medication is a known binder that can bind up thyroid hormone which results in secretion through the stool. Cholestyramine is sometimes used in alternative therapies to bind toxins to help cleanse the body. If you are using it for this purpose make sure that you take it away from your thyroid medication.
- Sucralfate (15) – Sucralfate is commonly used to treat ulcers in the GI tract but it is another binder that has been shown to bind to and inactivate thyroid medication.
- Iodine – Iodine is a tricky nutrient in that it is required for proper thyroid function but overconsumption may also cause issues with thyroid hormone absorption and cellular activation. Using iodine in recommended dosages, such as 150-200mcg per day can help prevent these unwanted side effects.
- Caffeine – Caffeine acts as a stimulant to the GI tract which may increase gut “transit” and result in reduced absorption of thyroid medication. This is especially problematic in those who consume coffee or energy drinks in the morning. If you fit into this category you may benefit from taking your thyroid medication in the evening.
- Acid Blockers (16) – Acid blockers such as H2 blockers and even proton pump inhibitors work by reducing the amount of acid that your body produces naturally. This results in a change in gut bacteria and may impact your ability to break down the inactive ingredients found in thyroid hormones. If you fit into this category you can look into natural treatments for acid reflux to help you get off of these medications.
- Calcium (17) – Calcium is a “binder” found in many over-the-counter and professional supplements. It’s often included in multivitamins, protein powders, and trace mineral supplements. While calcium is important for your health you want to make sure you don’t take supplements that contain calcium around the same time as your thyroid medication.
- Estrogen (18) – Estrogen (the hormone) doesn’t impact absorption, but it can increase the amount of thyroid-binding globulin that your body produces (19). This may result in a situation where your body has sufficient thyroid hormone in the body, but much of it may be bound up by binding globulins and therefore not useful to your body or cells. Make sure you consider this as you use sex hormones for conditions such as menopause.
What to Do if you Think your Medication is Interfering with your Thyroid
What are you supposed to do if you believe that your medication may be interfering with your thyroid?
Below I’ve included a list of potential options for you to consider.
Please note that not all of these options may be available to you, however, because not everyone may be able to switch medications or stop them entirely.
It’s very possible that you are taking a medication that is necessary for your body (for some reason) and you must deal with the side effect of thyroid dysfunction as a result.
That doesn’t mean you can’t take steps to improve your thyroid function, but it does mean that you may not be able to switch medications.
#1. Try to switch to a different medication in the same (or different) class
The first option you should consider is simply switching medications or switching to a different class of medications.
Let’s use high blood pressure as an example:
There are many different types of blood pressure medications that can help drive down your blood pressure and they all act in slightly different ways.

If you are taking a beta-blocker (such as propranolol) for your blood pressure, you may be able to ask your doctor about switching to a different class of medication.
This may also work for those taking diabetic medications, blood pressure medications, and anti-seizure medications which all block thyroid function.
Make sure that you discuss potential options with your prescribing doctor before making any changes!
#2. Try natural treatments (if possible) in an attempt to wean yourself off of your medication
Another alternative is to try and use a natural approach, as opposed to conventional medication, to treat your problem.
Let’s go back to the blood pressure example again:
High blood pressure may be caused by a combination of diet, fat mass, salt intake, and other factors such as insulin resistance.
It makes sense to try and REVERSE the causes of high blood pressure as opposed to simply covering it up with medication like beta blockers.
Most patients find that as they lose weight their blood pressure falls and they no longer need their medication.
This is also true for patients who suffer from conditions such as type II diabetes or insulin resistance.
Moral of the story?
If possible, do your best to try alternative and natural treatments to try and wean yourself off of your medication.
It may surprise you to know that there are many ways to treat medical conditions outside of medications, but they may require some energy and research on your part.
#3. Take your medication away from your thyroid medication (if possible)
Another option and one that we’ve discussed briefly in this article is to take your thyroid medication as far away from your other medications as possible.
This might mean taking your thyroid medication in the morning and all other medications in the evening, or vice versa.
If you have prescription medications you NEED to take in the morning then you can swap and take all medications in the AM and your thyroid medication in the PM.
Don’t be afraid to play around with the time of day that you take your medications to find a regimen that fits your body.
In some cases, I spend a lot of time just figuring out the ideal time for patients to take medications and hormones throughout the day and it makes a huge difference.
#4. Take supplements to promote thyroid function to try and “balance” the negative effects
Lastly, you may want to consider taking supplements designed to “boost” thyroid function.
These supplements may be able to counteract some of the negative effects seen by medications and supplements by providing your body with the nutrients it needs to produce and activate thyroid hormone.
In this way, you may be able to “brute force” your way to thyroid function.
Certain supplements such as zinc, selenium, iodine, and vitamin A may help your body convert T4 thyroid hormone to T3 and help thyroid hormone work at the cellular level.
You can find supplements that fit into this category here.
Final Thoughts
It turns out that many different prescription medications and even over-the-counter supplements have the ability to interact with your thyroid medication.
These are very important to consider, especially if you are someone who is taking thyroid medication but not feeling very well.
By using the tips and tricks outlined in this article you may be on your way to improving your thyroid function without making huge changes!
Now I want to hear from you:
Are you taking medications that may interfere with your thyroid?
What about supplements?
What have you done to fix these problems?
Leave your comments or questions below!
Scientific References
#1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3191684/
#2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3267517/
#3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3475282/
#4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1714646/
#5. https://www.ncbi.nlm.nih.gov/pubmed/108922
#6. https://www.ncbi.nlm.nih.gov/pubmed/11790981
#7. https://www.ncbi.nlm.nih.gov/pubmed/27546693
#8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3568739/
#9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3754371/
#10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3474631/
#11. https://www.ncbi.nlm.nih.gov/pubmed/21149757
#12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2758731/
#13. https://www.ncbi.nlm.nih.gov/pubmed/28155174
#14. https://www.ncbi.nlm.nih.gov/pubmed/18946743
#15. https://www.ncbi.nlm.nih.gov/pubmed/8017451
#16. https://www.ncbi.nlm.nih.gov/pubmed/25040647
#17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3092723/
#18. https://www.ncbi.nlm.nih.gov/pubmed/25040647
#19. https://www.ncbi.nlm.nih.gov/pubmed/2837662




Hey Doc! How about taking thyroid medicine on an empty stomach first thing in the morning, then man can eat after 30 min to an hour?
Hi Adnan,
That should be fine, you’ll just have to monitor how you feel to make sure you are absorbing it appropriately.
For years I’ve been taking my throid meds w/ other meds and selenium in the am. I wait 0.5 hour before eating. If I eat first, I wait 2 hours before taking the thyroid meds. I’m going to try your suggestion of isolating the thyroid meds from the rest and see if things improve.
Hello again. Thank you for your replies and your dedication to this fabulous blog. I spoke with my doctor and I’m completely going off my Armour medication after 5 weeks after being on synthroid for 15 years. My blood levels are all over the place and I feel terrible so I’m going to try and see how I do on my own with my doctor’s supervision. However, I want to take an all around healthy supplement to support healthy thyroid function. I was looking at your products and reading the importance of selenium and zinc, etc. Would the thyroid adrenal reset supplement you offer be my best option? I’m very confused about what to look for when personally choosing an all around supplement to help myself!
Hi Amy,
I don’t think there’s a best all around supplement for your thyroid, but most thyroid patients tend to do well on both T3 Conversion Booster and Thyroid Adrenal Reset Complex.
Hope this helps!
What are t3 and t4? I don’t understand.
Joyce
Hi Joyce,
T3 and T4 are the different thyroid hormones in your body. You can learn more about what they do and the differences between them here: https://www.restartmed.com/t3-and-t4/
Thanks for the reply. Big help! Can you take the conversion booster and the restart supplements together or do you choose one or the other?
Hi Amy,
Most people take them together but some people do one or the other, but it’s safe to use both simultaneously.
Great. Thanks so much for your reply!! It’s so inspiring that you try to educate and help people for the right reasons. Thanks again for your expertise and response.
You’re welcome 🙂
Interesting points- but what about those on only T3?
Hi Trev,
Some of the information is still relevant, such as when you take the medication and if you take it on an empty stomach. You’ll still want to take steps to maximize absorption.
I keep my thyroid medication by my bed. I always have to get up & go to the bathroom in the middle of the night, so I take my thyroid medication then. What are your thoughts on this?
Hi April,
It shouldn’t be an issue if it’s working well for you and as long as you take it around the same time each night.
Hi Dr Childs, Great podcasts! I listend to your splitting dose. Can you take an evening dose of NDT? I thought the T3 in the NDT would make sleep more difficult? Please explain of NDT would be OK to take at before bed. PS. I have been splitting my dose to take 11/2 in the early morning and then 1/2 around 3 to make sure the half life of T3 can take me over the mid afternoon slump…
thanks!! Bonita
Bonita,
I split my dose of NDT between morning and evening and it does fine for me. My daughter takes all of her NDT at night because she says it helps her sleep better. I would say to give the split a trial of a week or so and if it keeps you awake at night then just go back to taking it during the day. Best wishes to you.
Hi… I’m wondering is it normal to always be charging the dosage of my meds. I’ve been on meds for over 2 years and its changed every time he draws my blood. which is ever 3 months. When I tell him I feel good. losing weight have energy. my periods are normal and I feel better than ever. Sure enough, my blood comes back and he changes it. I gain weight feel like crap and my periods are the worse now with every bleeding and blood clots. I’m so confused! Doc. Says my periods should have nothing to do with the meds 🙁 wish I could just get off meds altogether. Thanks for listening.
Hi Bridgette,
In general, I feel that it’s not a good idea to continually alter your dose. Physicians who chase the TSH tend to do this which causes dosage changes continually for patients.
Hi Dr. Westin! Will I have any side effects from the Adrenal booster and Pea protein powder? I take levothyroxine and liothyronine! Thanks Marilu
Hi Marilu,
Both supplements tend to be very well tolerated so it’s unlikely that you will have side effects (except for positive ones). Hope this helps!
If you take progestrone at night can you still take armour thyroid medication at night also?
Hi Carolee,
Yes, that shouldn’t be a problem.
Hello Doc, I’ve had hypothyroidism for prob a year to year in a half. Was put on levothyroxine 50mg daily then recently one of my t levels was .21. My doc said I was taking to much levothyroxine so I take one tablet of 50 mg daily but on Sundays, I split my pill and only take 25mg. I’m so tired and exhausted still even though I’m on levothyroxine. I joined a gym and usually go three to four times a week but that’s not helping the tiredness nor weight loss. Any suggestions????
Hi Tammy,
I would recommend that you take a look at this blog post which should help you understand how to approach weight loss: https://www.restartmed.com/lose-weight-hypothyroidism/
I had a total thyroidectomy and have had issues with RT3 high side also suffer with a lot of inflammation and a fatty liver high ferritin and recurring EBV I am currently taking 150 mg of levothyroxine and liothyronine 5mg twice a day when do you recommend I take them I already take zaaflex 4 mg muscle relaxer and progesterone 200 mg at bed time. Can I benefit from taking thyroid adrenal reset complex?
Hi Mary,
The answer is probably, but there’s no way to tell for sure. It sounds like you would be a great candidate though. If it doesn’t work out you can always take advantage of our 30-day guarantee. I hope this helps!
Dr. Childs, I just wanted to say thank you for writing this thorough and comprehensive article. You answered all of my questions and I learned so much that I didn’t know! I’m panicking due to the shortage of NatureThroid. It has worked so well for me I fear having to switch. NP was recommended but I read too many negative comments about it. I refused to take the synthroid/Levo drugs due to the weight gain and hair loss I saw my poor sister have to deal with, so my Naturopathic Dr. started me on Nature Throid 8 years ago due to Hashimotos. I’m on 32 mg but am thinking about cutting it in half to see if I can get by. Also, my blood pressure is really bad and has been since I was 46, I.m 54 now so it started when my Hashimotos began. I take Hawthorne and Carditone for my high bp and progesterone (Compounded) for hotflashes. Do you think any of these may be harmful along with NatureThroid? Thank you again for this great informative article.
I’m confused, on table 2, “Substances that interact with Levothyroxine” You have Zinc, Selenium, & Iodine, however under #4 “Take supplements to promote thyroid function to try and “Balance” the negative effects” You have Zinc, Selenium, Iodine & Vitamin A, so which is it, can you take these supplements or not.
Hi there,
You can absolutely take those supplements but you should NOT take them at the same time as your medication. Levothyroxine is the medication and the list you are referring to is nutrients that BLOCK thyroid hormone absorption. But, those same nutrients are required for thyroid hormone ACTIVATION inside of your body. They just shouldn’t be taken at the exact same time as your medication. This is important because many people do take them to boost their thyroid function without realizing that they can block thyroid hormone absorption.
I accidentally took double. of my Levothyroxine I take 75mcg every am. This morning I took 2. What can I expect?
Hi Shirley,
Probably nothing! You can read more about what happens here: https://www.restartmed.com/synthroid-overdose/
Hi! Thank you for taking the time to educate those of us who struggle with Thyroid issues. After reading some of your articles I realized that taking Nexium and Welbutrin at night might be affecting the absorption of my Tirosint at 6am. I purposely take it at 6am so I can have coffee after 7am. But I have erratic blood test results. Should I try taking the Tirosint only at night or take the medications midday and continue to take Tirosint in the a.m.? Again, thank you so much for your informative articles!
Hi Chris,
Tirosint is actually fairly well absorbed even in the face of using various medications and consuming it with food. But I do agree that acid blockers can cause a number of issues including bacterial gut disturbances and nutrient deficiencies.
I had thyroid surgery in 2015. I am struggling with losing weight there are times where I feel very tired fatigue and anxiety, depression. My medication is Levothyroxine which I take in the morning. But I’m also started taking collagen I wait 30 minutes after taking my meds I have also been taking multivitamins, and omega seven, I try to watch what I eat, But nothing I do is helping me lose weight I’m really struggling since my surgery in 2015. I don’t know if I should try to start taking my meds at night as I’ve been reading the article, and if I should try the T3 booster. Can really use some advice.
Hi Maria,
I would take a look at these resources for more help:
https://www.restartmed.com/hormone-mastery/
https://www.restartmed.com/supplement-guide/
https://www.restartmed.com/weight-loss-thyroidectomy/
Dr. Childs, I am so happy to read your info. I’ve been back and forth trying many types of thyroid meds. I’m now on NP 90mg. I take about 4 am. My ferritin was so bad and iodine so low. I’m not sure as to what to get. I am on your thyroid adrenal support. I read you need vit. C for absorption of iron?
I will try spreading out the calcium and iron. Please, any suggestions? My nervousness, heart beat, shakiness is past!
But I teach fitness and try to eat well. I’m confused now as to foods not good for thyroid. I see kale on the list as others. Can you clarify these foods? Thank you for your time, Vicky.
Hi Vicky,
I would take a look at this blog post for more information on which foods you should be eating/avoiding if you have thyroid issues: https://www.restartmed.com/thyroid-foods-to-avoid/
Also, you can take a look at this one as well: https://www.restartmed.com/thyroid-approved-foods/
Dr. Child’s, I have had to use slot of antibiotics in the last 1.5 years due to infections after ankle surgery and diverticulitis, and I’m curious if you have had patients experience more adverse hypo symptoms? I have no thyroid and use desiccated thyroid, but I’ve read somewhere that some antibiotics can interfere with absorption of the thyroid, what do you think? I literally couldn’t get off the couch, mental fog reappeared, within 5 days off the antibiotics, symptoms disappeared. Thanks for all your amazing articles. Now just to get some weight off. Lol.
Dr. Childs,
Thank you for all the great information! I feel like I’m finally on track to stopping the hair loss, the aches and pains, the fatigue and the dry skin. I’m finally starting to feel better on Armour Thyroid. I have been on Metformin and figured THAT is was interfering with my thyroid medication.
I went off Metformin and started using Berberine instead. Do you think it will also interfere with the thyroid medication, just like the Metformin did?
Dr. Childs,
Glad to see the article about getting the doctor to work with you. Had a fantastic functional GP in Australia…spoiled me with her consultative participative approach. Coming to the US, it’s been unsuccessful. AU doctor worked with me to stay of bp meds, and we monitored elevated bp for years. Here, I can’t get the doctor to stop pushing meds for bp. Weight is most of the problem (as it has been for years w/ Hashimoto’s). Good days and weeks of physical activity and bp and others I just have to ride it out. I hesitate to take my health back into my own hands, at 65. I’m sure I can do better now that I’m on Tirosint and LDN (thank you for that info as well!). Weight is slowly dropping a couple of pounds a month. I’d be interested in your thoughts on the bp…tends to hover at 140/90 or 150 over 90. Has gotten higher at times when I’m riding out inflammation. Thanks for your input.
Dr. Childs.
I’m so impressed with your knowledge and your excellence in sharing it. I’m full of gratitude for you.
I’m 79 years old and have been under hypo thyroid treatment since 2012.
I’m on Compounded Sustained Release T3 after trying every other thyroid medication and combination in existence.
My present dosage being T3 18mcg + T4 2.5mcg SR Q12 hrs.
My symptoms have gradually gone away since starting the T3 regime, including morning temperature rising to 98.4 to 98.8.
My Free T4 is now way down below normal.
Should I worry about this considering i’m feeling good.
My last TSH 1.5, Free T3 2.9 and Free T4 0.43.
Tirosint 5 mg recently was added to help boost Free T4 but it dropped my TSH 0.5 point. (That was without any addition of T3).
I think I’m getting more benefit adding T3 versus T4 to my next dose. What do you think? Is there anything that can be done to otherwise increase Free T4 without lowering TSH too far?
Any other advise is greatly appreciated!
I’m am forever indebted!
God BlessYou!
Thank you for sharing all the great information with us. I’ve read that ALA & ALCAR both seem to decrease how well thyroid hormone works and was wondering what your expert opinion is?
Thank you for your great information. I would like to ask, I have been nicely controlled by using Euthyrox 150mcg however sometimes I don’t feel great. I sometimes drink coffee in the morning over 1 hour after taking Euthyrox and I do weights in the gym in the evening, so I supplement with Creatine, Protein and multivitamins, I take creatine over 6 hours away from Euthyrox, and multivitamins 5 hours away, would that be ok? considering I take Euthyrox at first time in the morning, or should I try passing Euthyrox to the evening and multivitamins at breakfast? Also, would taking prohormones or using animal mstak from universal affect my thyroid? Thank you very much in advance.
Hello Dr Childs,
What blood pressure medicine do you recommend instead of a Beta Blocker? I take 25mg atenolol 2x/day and have for about 10 yrs. My local functional doctor recommends Arb’s.
Thank you for your time.
What order do you suggest one should take the following?
Levothyroxine
Calcium 3x
Eliquis 2x
Iron 1x
Ferrous 1
Lorsartan HcTZ 1 x
Propaphenol 3x