How do you know if neck pain is really thyroid pain?
Is thyroid pain a serious medical condition?
Will thyroid pain cause other symptoms or problems?
This post will walk you through the causes of thyroid pain including other symptoms you may experience and what you should do about it:
Neck Pain & Thyroid Pain – When is it Serious?
Thyroid pain is never a normal symptom.
But just like any other tissue in your body, your thyroid gland is subject to trauma, inflammation, infection or even autoimmune attack.
All of these conditions may result in damage or inflammation to the thyroid gland which you may feel as pain.
Under normal conditions, it sits in the front of your neck wrapped around a portion of your trachea or windpipe.
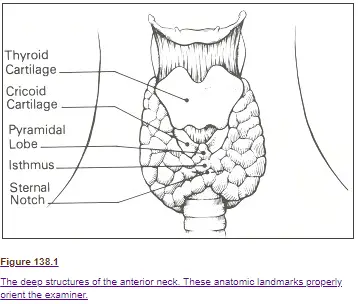
If you can feel around the lower part of your neck and it’s tender to the touch then your pain may be caused by your thyroid gland.
Other conditions, such as enlarged lymph nodes, can also cause pain in the neck, but these tend to run underneath the jawline and down the side of the neck.
Believe it or not, thyroid pain is actually a fairly UNCOMMON symptom and most diseases of the thyroid gland do not cause thyroid pain.
Conditions such as Hashimoto’s thyroiditis, Graves’ disease, postpartum thyroiditis, hypothyroidism, hyperthyroidism, and thyroid nodules typically do not present with pain in the thyroid gland.
This means that the presence of pain in your thyroid gland can give you a special clue as to what is happening in your body.
But make no mistake:
All causes of thyroid pain need to be evaluated and treated because it is never “normal”.
If you are experiencing thyroid pain then the chances are high that you are also experiencing other symptoms as well.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Other Symptoms Associated with Thyroid Pain
Conditions that cause thyroid pain also tend to cause problems with the thyroid gland itself.
Remember:
Your thyroid gland helps produce some of the most powerful hormones in your entire body: T3 and T4 thyroid hormones.
If there is any damage to the thyroid gland, either from inflammation or an infection, then the ability of your gland to produce these hormones may be compromised.
Inflammation and pain in the thyroid gland almost always come with some disruption to thyroid hormones.
This means that the chances are quite high that if you have thyroid pain then you will also have other symptoms accompanying that pain.
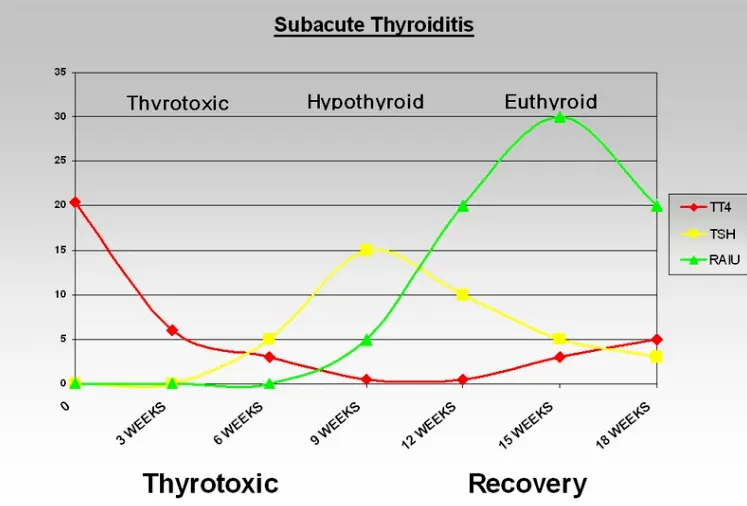
Disruption of thyroid hormones tends to follow a typical course of symptoms.
If you fall into this category then you will most likely start out feeling the symptoms associated with hyperthyroidism.
Hyperthyroidism is the result of excessive thyroid hormone production.
So when your thyroid is damaged by inflammation it responds by INCREASING the amount of thyroid hormone it produces.
This causes a “flush” in the system which temporarily causes too much thyroid hormone in your body.
During this phase, you may feel symptoms such as:
- Anxiety
- Fatigue
- Heart palpitations (feeling like your heart is going to beat out of your chest)
- Fever or hot flashes
- Diarrhea (or loose stools)
- Irritability
- Tremors of your hands
- Rapid weight loss
- And an increased body temperature
These symptoms tend to fade over a period of a few weeks to months.
It is during this time frame that you might present to your Doctor knowing that something is “off”.
If the symptoms are affecting your quality of life you can take certain medications which block the impact of thyroid hormone on your body (such as beta-blockers) (2) which should help reduce heart palpitations and so on.
Once the hyperthyroid symptoms fade you will then most likely experience the exact opposite which is known as hypothyroidism.
Hypothyroidism is the result of too little thyroid hormone in the body.
You can imagine that once your body pumps out all of the thyroid hormones it had in storage that there is little left afterward.
The reduction in thyroid hormone production in this phase may also be caused by temporary, but reversible, damage to the thyroid gland.
During this phase, you may experience the symptoms of hypothyroidism such as:
- Temporary weight gain (sometimes persistent)
- Fatigue or low energy
- Hair loss
- Dry skin
- Constipation
- Depression or other mood changes
- Not feeling like yourself
- Menstrual problems or irregularities
These symptoms are generally NOT permanent and tend to fade over time (a period of a few weeks to months depending on the cause).
It’s always a good idea to get your thyroid tested through routine bloodwork if you are experiencing these symptoms along with thyroid pain.
Conditions that Cause Thyroid Pain
There are actually many different medical conditions that may lead to thyroid pain.
It’s important to differentiate between these conditions because not all of these conditions are treated in the same way.
The good news is that the most common cause of thyroid pain is subacute thyroiditis which will generally go away on its own.
If you are experiencing thyroid pain then you should be evaluated for the following medical conditions:
#1. Subacute Thyroiditis
Subacute thyroiditis is the most common cause of neck pain among all conditions of the thyroid gland (3).
Any condition which results in inflammation of the thyroid gland may potentially result in pain in that same area.
This particular condition is usually the result of an infection but it can be an infection from a virus or bacteria or fungus.
The most common subtype of subacute thyroiditis is known as subacute granulomatous thyroiditis which is typically caused by a viral infection.
The good news is that viral infections tend to be cleared up by the immune system over time and without any intervention (all you need is rest, some anti-inflammatory supplements or medicines, and time).
Other forms of thyroiditis, such as those caused by bacteria or fungus (4), may require more heavy-duty medications such as antibiotics or antifungals.
Subacute thyroiditis, despite it being the most common cause of neck pain, is actually not very common at all.
This means that you can usually identify the type of thyroiditis that you have simply by whether or not pain is present in your thyroid gland.
If you have pain then the chances are high that your condition is subacute thyroiditis.
If you do not have pain, then the chances are high that your thyroiditis is caused by some other cause.
#2. Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is the most common cause of thyroid inflammation and its caused by an autoimmune attack on the thyroid gland.
You would think that because Hashimoto’s is so common and because it results in inflammation and damage to the thyroid gland that it would present with thyroid pain.
The truth is that MOST patients with Hashimoto’s thyroiditis do NOT have any pain, but that doesn’t mean that all patients will be pain-free.

If you have thyroid pain you can easily test for Hashimoto’s thyroiditis by checking simple thyroid antibodies on routine bloodwork.
#3. Lymphadenopathy
Lymphadenopathy refers to the enlargement or swelling of your lymph nodes.
Sometimes, the enlargement of these lymph nodes can be confused for thyroid pain.
The best way to differentiate between enlarged tender lymph nodes and pain in your thyroid gland is located.
The thyroid gland (normally) sits in the FRONT of your neck whereas your lymph nodes tend to follow down the sides of your neck and underneath the jaw/chin.
Some thyroid conditions, such as thyroid cancer or thyroid infection, may result in both thyroid pain and enlargement of your lymph nodes.
#4. Thyroid Cancer
Thyroid cancer generally does NOT cause pain but it can in some instances.
Pain related to thyroid cancer is rare but it should always be thought of.
#5. Postpartum Thyroiditis
Postpartum thyroiditis is a condition of the thyroid gland which develops after pregnancy.
Sometimes this condition can also present with pain in the thyroid gland (9).
You can identify postpartum thyroiditis because it usually is associated with OTHER symptoms (both hyperthyroid and hypothyroid symptoms) and because it tends to come after pregnancy.
Some of the symptoms of postpartum thyroiditis can mimic postpartum depression so it’s important to diagnose this condition if you feel it is present.
You can figure out if you have it by going to your Doctor and getting simple routine thyroid lab tests such as the TSH, Free T3, Free T4, and thyroid antibodies.
Treatment Options & What to do Next
Treating thyroid pain should focus on identifying and diagnosing the underlying cause.
Each treatment, for the conditions listed above, may be different.
Some conditions, such as postpartum thyroiditis and subacute thyroiditis, may go away on their own with time and simple anti-inflammatory medications.
On the other hand, some conditions, such as thyroid cancer and Hashimoto’s thyroiditis, are not likely to go away without serious treatment or intervention.
In most cases, you will probably need to take something to cool off the inflammation in your thyroid gland to help reduce the pain.
Certain supplements such as Alpha lipoic acid (10), turmeric (11), or fish oil may help (12).
Other over-the-counter medications like NSAIDs may also be effective (13).
It’s important to note that the treatment for thyroid pain will probably not alter the other symptoms that we discussed previously.
Treating these symptoms may require thyroid hormone medication or other medications to temporarily blunt thyroid hormone.
Conclusion
Thyroid pain is a relatively uncommon symptom among patients who have thyroid problems.
Having said that, it’s still a serious condition that needs to be evaluated by a physician if present.
Once you have a diagnosis you can hone in on treatment options.
Thyroid pain is often accompanied by symptoms related to changes in thyroid hormone in your body.
These symptoms may range from fatigue to weight gain to hair loss and more.
Most of the time, thyroid pain is a sign of inflammation related to an infection or your immune system which will fade on its own over time (but not always).
When in doubt make sure that you touch base with your Doctor to get the right lab tests to figure out what is going on in your body.
Now I want to hear from you:
Are you suffering from thyroid pain?
Do you know why you have it?
Have you been able to find relief?
Are you also experiencing the symptoms of thyroid hormone dysfunction?
Leave your comments below!


I was diagnosed with hashimotos about 20 years ago and it’s seemed to be under control. However, after having some symptoms (heart palpitations, choking sensation, especially after eating, racing thoughts, plus aches and pains beyond the usual) I had blood work done. T3 and t4 were low levels of normal, tsh was 29.5 (Dr says 4.5 is high range of normal). Is this thyroid resistance? I’ve started taking supplements and changed my diet (cut out artificial sweeteners), but my thyroid gland pulses and constricts after I eat or drink alcohol.
Hi Karen,
Thyroid resistance is generally felt to be where the body is resistant to thyroid hormone. It sounds like you are probably experiencing hypothyroid/Hashimoto’s inflammation-related symptoms.
I have Hashimotos and significant thyroid pain that started after a sinus infection about 6 years ago. I have routine ultrasounds which demonstrate several nodules but none greater than .8mm so doctors won’t biopsy. Can I have a chronic infection for 6 years that would cause pain this long? Or is this related to the Hashimotos? I have not been treated for Hashimotos as per doctors my TSH is “fine”. It is 2.98. I have run my own test and my reverse T3 is elevated at 36. Should I be on medication and would this help reduce the pain?
Hi Jenn,
Your sinus infection should not cause thyroid related issues, but it would be a really good idea to check for antibodies. Having a normal TSH is not a reason to avoid testing for thyroid antibodies as many patients have “normal” thyroid lab tests with Hashimoto’s.
Yes, Dr. Childs, I do have thyroid antibodies. My TPO is 117. My thyroglobulin antibody came back under 1.0 this time but has been elevated in the past. So is my pain just directly related to the hashimotos? From your article it appeared that most individuals with Hashimotos do not have pain. Maybe I am one of them? And with subacute thyroiditis I probably wouldn’t have the pain this long. Am I correct? Thank you for your time.
I have been hypo for 20 years or so, diagnosed with Hashimoto’s a year ago… now my thyroid is so painful, my blood work and ultrasound do not show anything… I feel a sensation of pressure and swelling but nothing is visible. So uncomfortable.
Hi Rowena,
Inflammation in the thyroid gland may be causing some of your symptoms. You can read more about it here: https://www.ncbi.nlm.nih.gov/pubmed/25636252
Are you suffering from thyroid pain? I believe so, but the thyroid tests tell my doctor I am okay
Do you know why you have it? No. I did have bronchitis about five months ago. I do have hypothyroidism for which I take medication for daily.
Have you been able to find relief? No. Ice helps a little. It comes and goes though too. It can be very mild to almost nonexistent to so bad my neck starts to hurt from being tense. Swallowing can be difficult at times as well.
Are you also experiencing the symptoms of thyroid hormone dysfunction? Still overweight, but losing due to being not able to eat much the last month or so (being treated for Gastritis also). Hypothyroidism is doing good with levothyroxine.
Hi,
I have been experiencing discomfort in my r ear with crackling sounds etc for over 12 months, I have had this looked at however I am told I have a dysfunctional tube. at about this time last year the front r side of my neck was sore to touch Dr ran tests for thyroid and said everything is fine. ear issues continue and now currently my neck is again excruciating to touch around the thyroid area and travelling up into my jaw line. I have not been ill or had any infections, I have been told by an ENT to live with the issues of my ear however I am concerned about the thyroid. I have had scans that did not show anything other than a few nodules. I have no trouble swallowing or eating but do have a metallic taste in my mouth almost constantly. Your advice would be appreciated
See a specialist it took me having many scans done under my jaw and neck line and they found the nodules I’m asking to get a biopsy in a few weeks to make sure it’s nothing serious tell them you want it done ! And you want the nodules out of you
Hi Dr. I was diagnosed with subacute thyroiditis on July 2nd I ended up at the hospital with fever even though I had been prescribed with antibiotics because the walking clinic doctor thought it was and ear infection that transfer from my neck to my ear.
I got a referral to see the endocrinologist my T4 leves were at 29/30 and he said with time things were going to get better but it was the opposite I started with 38.5 fever almost every day for a week I called the specialist and he sent me for blood work T4 results came back at 70 so almost 2 months with pain symptoms neck ear jaw feeling hot no energy
I started beta blockers and methimazole
Is this a normal process for subacute thyroiditis?
I was diagnosed with auto immune thyroiditis and after asking my GP whether that was Hashimoto’s he said, well, yes. Thanks for that! Anyway, he did a broad range of tests initially for auto immune diseases because I had inflammation everywhere and sore feet and heels, burning and pain in my hip, pings in my leg that caused jabbing pain in the bottom of my hell when bending and extreme pain in my arms and inability to open my middle fingers on both hands to mention just a few symptoms. He sent me for ultrasounds of my thyroid which revealed nodules, non cancerous, thankfully. However, I have been experiencing pain and difficulty swallowing and the nodules seem to swell up when this happens. I also have glands along my neck and at the edge of my jaw that get swollen and sore. He doesn’t seem to have an answer for this. I have been on Eutroxsig (levothyroxine sodium) initially 50 m/g but after 3 months I asked to increase it and he had me take 1.5 tablets. I have gone gluten free, dairy free, soy free (unless it is hidden) and try to limit my sugar from natural sources and only use raw for baking. I have also stopped any highly processed foods and no deli meats at all (sob), so no lovely pepperoni or Italian sausage. I have lost weight due to the dietary changes and the bloating in my stomach is mostly gone. I am still getting inflammation in my feet and soreness in my fingers, elbows, hip, weakness in muscles and pain on the side of my knee (burning also) if I kneel on them. The nodule pain I am assuming it is a result of inflammation as I often get what I initially thought were hot flushes after the pain or before it. I currently am not on any additional supplements and have an appointment next month with an endocrinologist. Initially Free T4 6.0 then 13.7 one month after medication and TSH 105.27 then 23.94. They could barely draw blood from me for these two lots of blood tests but the second draw was better and they didn’t need a syringe to get it. Then had a test for Vitamin D and had a normal blood draw after 2 months (at my request). The GP said it was low (20 nmol/L) and said to get more sun?!? Do you have any solution for the nodule pain since your articles say pain is rare?
Hi Angele,
Getting sun is definitely a good idea (if it’s possible at your latitude) but you can definitely also add in a D3 supplement as well. In terms of the nodules, the best approach is to try and shrink them as that will probably reduce the pain.
I’m from Germany. Maybe it’s more a case report (strange pain).
More than 20 years ago (in my 30s) I got a severe bronchitis and I didn’t fully recover, feeling exhausted, tired. So I got my thyroid checked. TSH was 6,5 at that time. I got L-Thyroxine… Now my TSH is 11,6 without medication.
I took 125 mcg. But suddenly (menopause/estrogen?) I got live threatening hypertension (240). Nothing helped so I stopped L-Thyroxine.
And: Changed my diet from High Carb to Low Carb. My BP is normal and I re-started L-Thyroxine.
It started last year: Sudden, short (1-3 mins),extreme! pain in the neck. Exactly where the thyroid is situated. I was shocked, could hardly speak and hoped that it wasn’t a heart attack.
After some month that pain came back. Now very 2 weeks.
And concentrating on the thyroid I have the impression that there is a constant minor pain there.
So weird. I started searching online. But no article mentions this kind of pain. I found one article. The MD said that thyroid inflammations often get activated in springtime in people – like me – with pollen allergies.
My allergies got this spring so bad that I have to take antihistamines. My skin is itching (maybe urticaria facticia). These AH meds make me very tired/sleepy and depressed. So I try to take less than one tablet. Trying to cover the symptoms a tiny bit.
Hi Onyx,
Have you been evaluated for subacute thyroiditis? https://www.restartmed.com/subacute-thyroiditis/