Would it surprise you to know that it takes at least 13 different nutrients to properly create and convert thyroid hormone to its active form?
Or that by replacing these nutrient deficiencies with thyroid supplements you may be able to reduce your symptoms of hypothyroidism?
You’re not alone…
If you are considering taking supplements to boost your thyroid function to help you feel better there are some things you need to know first.
Not all supplements are created equal and everyone out there claims to have the “best product”.
Which is why I created this guide.
I‘ve been helping hypothyroid patients for years and I’ve found certain supplements help thyroid patients feel better and I want to share these with you.
In this article, I’m going to go over the top 9 thyroid supplements that you should consider using if you want your help your thyroid function the way it was designed to function…
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Do Supplements Actually Help Thyroid Function?
Let’s get this out of the way:
Yes, supplements can definitely help boost your thyroid function, but not how you think…
Many run-of-the-mill thyroid supplements contain all of the nutrients that MIGHT help thyroid function, but that’s the wrong approach.
A better one is to find what your body is deficient in and then give back what it needs.
And it just makes sense, right?
If your body lacks zinc, for instance, then your immune system will function less optimally (1) until you restore that nutrient back to normal levels.
And, this isn’t made up guys, there are many studies showing how common nutrient deficiencies are and what kind of symptoms to expect with those deficiencies.
But, unfortunately, you have articles like these floating around sowing confusion:
These articles would have you believe that taking supplements isn’t helpful and, in fact, might be harmful.
And I would probably agree with that, assuming you don’t know how to use supplements correctly.
But that isn’t going to be a problem for you because I’m going to discuss how to tell which supplements to use and how to use them safely starting right now:
9 Thyroid Supplements to Help Improve Your Thyroid
Remember when I said it takes at least 13 different nutrients for proper thyroid hormone production and conversion?
I wasn’t kidding:
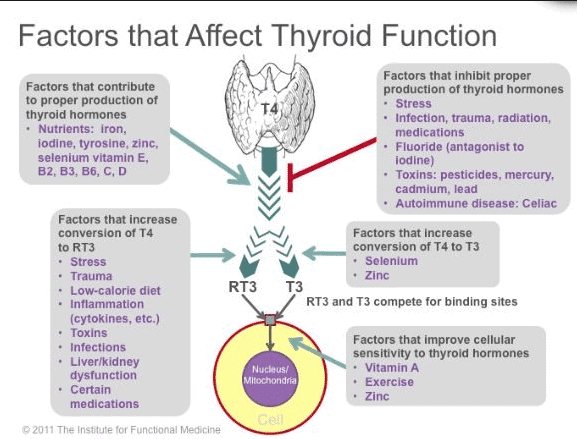
The following nutrients are required for proper thyroid hormone production:
- Iron -> Needed for thyroid hormone production.
- Iodine -> Required for creating thyroid hormone.
- Tyrosine -> Also needed for creating thyroid hormone.
- Zinc -> Needed for thyroid hormone cellular binding.
- Selenium -> Needed to convert T4 into T3 and to protect the thyroid gland from damage.
- Vitamin E (2) -> Protects the thyroid from cellular damage.
- Vitamin A -> Needed for thyroid hormone cellular signaling.
- Vitamin B2 (3)
- Vitamin B3 (4)
- Vitamin B6
- Vitamin C
- Vitamin D -> Protects against thyroid cancer and thyroid autoimmune disease.
Does that mean you should just blindly take these nutrients?
The answer to that is obviously no, and taking that approach may lead to problems…
Instead, my goal here is to walk you through how to properly and safely use targeted supplements to help naturally improve your thyroid.
The 9 nutrients below have been hand-picked by me because I think they are the most beneficial for thyroid patients.
This is based on my own personal experience helping thousands of thyroid patients over the last 7 years and providing over 80,000+ thyroid patients with thyroid support supplements over a similar time period.
#1. Vitamin B12
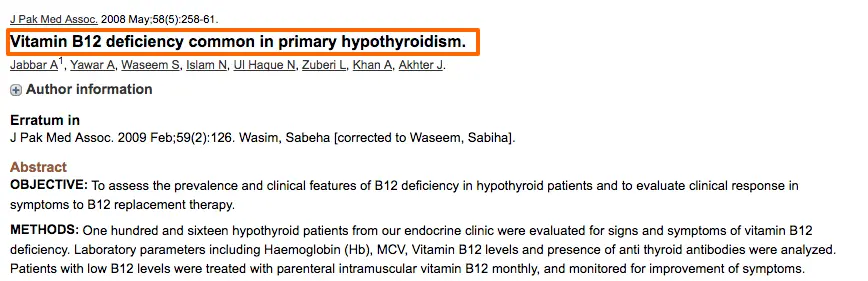
Vitamin B12 is the first vitamin we are going to talk about today and for good reason:
Based on studies as many as 40% of patients with hypothyroidism are ALSO vitamin B12 deficient (5).
And that’s very concerning when you consider the symptoms of B12 deficiency:
- Fatigue
- Shortness of Breath
- Anemia
- Neurological changes which can mimic dementia (6)
- Difficulty with concentration or brain fog
Do you see the problem here?
Many of these symptoms are also symptoms of hypothyroidism so you may be walking around with both issues.
This means that you may be taking the right type and dose of thyroid medication but your symptoms may persist if you don’t also replace your low vitamin B12.
How do you know if you should supplement with B12?
How to Tell If You Need B12
You might be tempted to just order some lab tests to figure out if you need to supplement, but it’s not quite that straightforward.
One major problem with B12 testing is most tests are not accurate.
Without getting too much into the weeds here, you should know that there are 3 basic ways to test for B12 and each one has faults.
The most accurate test is also the most expensive and it really doesn’t make sense to order it because it’s cheaper to just purchase a B12 supplement than it is to pay for the test.
Given the fact that so many thyroid patients don’t have enough B12 in their system and that testing is inaccurate and that supplementing is cheap and safe, I think shotgun supplementing makes the most sense.
The question is, what type and form of B12 should you use?
For thyroid patients, the answer is usually pretty straightforward:
The Best Form of B12 For Thyroid Patients
Due to the impact that low thyroid has on stomach acid and the absorption of vitamin B12, getting your B12 from shots is usually the best source.
If you don’t like the idea of getting shots, or if you can’t find someone to provide them to you then oral B12 in capsule form or sublingual B12 will do the job as well.
No matter what way you choose to get your B12, you should make sure that you are getting a pre-methylated and pre-activated form of B12.
Cheap forms of vitamin B12 like cyanocobalamin require extra steps to become activated by the body and even result in the creation of goitrogenic compounds.
For this reason, you will want to look for methylcobalamin, adenosylcobalamin, or hydroxycobalamin.
These forms are ready to be used, will not result in the creation of toxic byproducts, and are safe for those with MTHFR genetic mutations.
You can see an example of the type, form, and dose of vitamin B12 you should be looking for as a thyroid patient in this supplement.
#2. Adrenal Support
Many hypothyroid patients suffer from both thyroid and adrenal problems.
Adrenal support refers to the use of nutrients and vitamins which help your adrenal glands produce powerful and important hormones such as cortisol.
Cortisol is a hormone released in times of stress which helps thyroid hormone (and other hormones) function.
By repeatedly taxing your adrenals (through stress or through thyroid dysfunction) you can cause adrenal-related issues which create a cascade of very specific symptoms.
This is important for your thyroid because we know that thyroid hormone is intricately linked to adrenal function.
As your TSH increases (hypothyroidism) your cortisol levels will rise as well (7) leading to the symptoms of adrenal fatigue.
This connection explains why so many thyroid patients also suffer from the symptoms of adrenal fatigue.
But perhaps even more important is the fact that treating yourself with thyroid hormone may not be sufficient to “heal” your adrenal glands.
I mentioned that the symptoms of adrenal fatigue are very specific, and that’s true. You can find a list of the symptoms associated with adrenal dysfunction below:
- Constant fatigue despite sleeping 8 hours at night
- Feeling “wired but tired”
- Experiencing a crash around 2-3 pm each day
- Getting your “second wind” at night around 10 pm
- Difficulty falling asleep
- Racing mind and thoughts
- Inability to tolerate stressful events
- Cravings for salty/sugary foods
- Always getting sick or having a weakened immune system
The presence of these symptoms indicates a disruption in cortisol. This disruption can either be at the cellular level or it can be in the absolute concentration of cortisol in your serum.
Adrenal Glandulars vs Adrenal Adaptogens for Thyroid Support
There are two ways to approach fixing adrenal problems with supplements and vitamins. You can use adrenal glandulars (#1) or adrenal adaptogens (#2) or a combination of both.
Even though we are going to primarily focus on the supplements today (that’s the purpose of this article, after all) you should be aware that other lifestyle therapies should also be employed if you have adrenal issues.
Dietary changes, meditation, stress reduction techniques, improving your sleep, and so on should all be considered mandatory elements of your treatment plan if you have adrenal issues.
Once you have determined you have cortisol-related issues you can determine how to proceed with treatment.
For instance:
Low cortisol can be addressed with adrenal glandulars and adrenal adaptogens, while high cortisol can be addressed with phosphatidylserine (8) and adrenal adaptogens.
Note: It isn’t always necessary to check for your cortisol prior to using adrenal supplements as sometimes your cortisol level may not “match” your symptoms.
Adrenal adaptogens are plant-based compounds that help you increase your stress tolerance by “nourishing” the adrenals.
They are often combined with vitamins and nutrients which form the building blocks for hormones such as cortisol and adrenaline.
Of the adaptogens, Rhodiola Rosea may be the most stimulating for the body which peaks around 30 minutes after ingestion (9).
Adaptogens can also be used in combination with adrenal glandulars which is one of my preferred methods for treatment.
Adrenal glandulars, or desiccated adrenal glands, contain portions of animal adrenal glands that contain hormone precursors and vitamins specific to the adrenal gland.
Don’t let this information confuse you, though, because you can’t go wrong in using either adrenal adaptogens or adrenal glandulars.
I’ve found, based on my experience, that most people do exceptionally well when combining both together.
I’ve had great success using this supplement which includes both adrenal adaptogens and adrenal glandular in the optimal ratio.
Treating your adrenals has a compounding effect in which it can potentially improve both your thyroid function and your adrenal function simultaneously.
#3. Zinc
Zinc is perhaps one of the most important and often missed, nutrient deficiencies found among hypothyroid patients.
In fact, there is a good chance that you have sub-optimal levels of zinc present in your body as you are reading this.
And this doesn’t bode well for your thyroid, given how many thyroid processes zinc is involved in.
One of the most important of these functions is the role that zinc plays in the conversion of T4 to T3.
Because zinc is required for thyroid conversion (T4 to T3 conversion), low levels of zinc may predispose you to develop high levels of reverse T3 and which may limit thyroid function (10).
These changes can also be identified through lab tests as low free T3 and low total T3.
But that’s not all zinc does…
The other benefits of zinc, as it relates to your thyroid, include:
- Enhanced immune function (11) – This is particularly important if you have Hashimoto’s thyroiditis or other autoimmune diseases.
- Increases T4 to T3 conversion – This helps normalize your free thyroid hormone levels (required for weight loss and symptom management)
- Acts as an anti-inflammatory agent – Helpful in those with Hashimoto’s or other causes of thyroiditis.
- Plays a role in reducing oxidative stress.
A severe deficiency in zinc may result in hypothyroid symptoms which can be reversed with supplementation (12).
Zinc deficiency is also associated with hair loss and alopecia, a troubling symptom that many hypothyroid patients face despite taking thyroid medication.
The real benefit to using zinc is that supplementing may help to improve thyroid function (if you are deficient) and help to reduce hair loss and improve hair quality.
Testing for zinc in the serum or plasma is generally not recommended as many people with “normal” values still present with the symptoms of zinc deficiency.
This idea was highlighted in this study which showed that the best way to confirm and treat zinc deficiency is with a trial of zinc supplementation, in fact, this is considered to be the “gold standard” (13).
If you suspect that sub-optimal zinc levels may be contributing to your hypothyroid symptoms then a trial of zinc may be appropriate.
Combining Zinc with Selenium
Zinc is an incredibly important mineral if you have hypothyroidism, but I’ve found that most thyroid patients experience superior results when they combine zinc with other nutrients.
This benefit is most likely related to the synergistic effect that multiple nutrients have on thyroid function.
It’s probably also due to the fact that many people with zinc deficiency probably also have other nutrient deficiencies.
If you combine zinc with selenium (and other nutrients) the total dose necessary for either will decrease and you will obtain the same benefit at a smaller dose.
Dosing Zinc
The dosage of zinc necessary to improve thyroid function is usually somewhere between 5 and 15mg of zinc per dose.
If you are severely zinc deficient then you may benefit from using a higher dose for 1-2 months. This will allow you to build up your zinc ‘storage’.
Once you have repleted zinc stores in your body, you can safely back down to a smaller daily dose which is just as effective in helping to improve thyroid function.
The most effective forms of zinc to use for thyroid support include zinc chelate, zinc monomethionine, zinc gluconate, zinc acetate, and zinc citrate.
If you are not using one of these forms then you will want to switch to one!
These formulations of zinc tend to be better absorbed compared to other formulations.
If you want to get the correct form of zinc in the right dose, then check out this supplement.
#4. Iron
I know I sound like a broken record here but Iron is another huge player when it comes to your thyroid.
But it is also unique among the nutrients that I am going to discuss in this article because it’s not something that you want to take unless you are sure you are deficient.
Other nutrients such as vitamin B12, zinc, selenium, etc. are considered to be incredibly safe nutrients that you should be able to take and tolerate without issue.
Iron, on the other hand, can potentially be harmful to your body if you use it without a documented deficiency.
It’s certainly safe to use, but it should only be used if you know you are deficient.
Now, with that warning out of the way, let’s go back to how iron impacts your thyroid.
It’s so important I’ve dedicated an entire post to it that you can read here, which outlines how hypothyroidism is worse in the presence of iron deficiency.
In a nutshell:
Iron is involved in the production of thyroid hormone from your thyroid gland.
Low levels of iron, therefore, worsen existing thyroid function (make your symptoms worse) (14).
In addition, as thyroid levels fall (even slightly) your body will have a difficult time absorbing iron in the intestinal tract.
This sets you up for further iron deficiency and worsening thyroid function.
Do you see the vicious cycle here?
What makes matters worse is that most physicians don’t treat iron deficiency unless it also is causing anemia (low red blood cells).
It’s certainly possible to have an iron deficiency that doesn’t cause anemia but which still impairs thyroid function in your body (15).
Identifying iron deficiency is actually quite easy and can be tested with routine blood work (more on that below) and combined with your symptoms.
To identify this problem all you need to do is ask for basic “iron studies” with your next set of blood work.
Once you have these labs you will want to focus on your ferritin level which tells you how much iron you have stored in your body.
Low levels of ferritin are associated with iron deficiency and impaired thyroid function.
You can also identify the presence of iron deficiency by assessing your clinical symptoms.
List of symptoms associated with Iron deficiency:
- Fatigue and weakness
- Shortness of breath (worse with exertion or exercise)
- Pale skin (especially in the creases of the hands)
- Dizziness or a sensation of lightheadedness
- Intolerance to exercise
- Cold hands and cold feet
- Brittle nails and hair loss (Iron deficiency is a VERY common cause of hair loss)
Again, notice the similarities between iron deficiency symptoms and the symptoms of hypothyroidism.
Often times it’s difficult to differentiate between these nutrient deficiency syndromes and hypothyroid symptoms unless you know to CHECK and understand your labs.
Don’t make the mistake of assuming that your doctor will understand this information, you may need to be an advocate for your own health, especially when it comes to using vitamins and supplements.
Once you have identified the presence of low iron you can begin treatment with over-the-counter iron supplements (but just be sure to do this with physician supervision as too much iron can be harmful).
Diagnosing Iron Deficiency
Testing for iron deficiency is quite easy and can be done by ordering the following tests and ensuring that they match with the “optimal” range provided below:
- Serum Iron – Middle of the reference range
- Ferritin – 70-80 is the “optimal” range (low ferritin is associated with hair loss)
- Percent Saturation – 35-38%
- TIBC – Middle of the reference range
You may find that your labs are considered “normal” but they may not be optimal. As a thyroid patient, you really need these results in the “optimal” range otherwise you may not feel improvement.
You can see an example of iron studies in a patient with thyroid disease below:
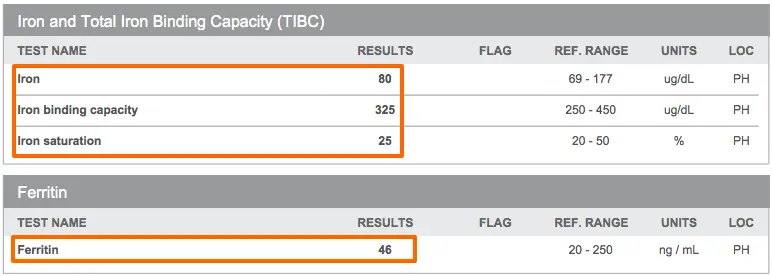
You can see that while these lab tests are within the “normal” range, they are not in the new “optimal” range that I’ve listed above.
For instance:
This patient has a normal iron of 80, but you can see that this iron level is certainly on the low end of the normal range.
In addition, her ferritin of 46, while normal, is not optimal for thyroid function or hair growth.
Ensuring that your ferritin is in the 50-60 ng/mL range will help with hair growth and symptom management.
Liquid Iron vs Iron Capsules/Tablets
One downside to using iron supplements is that they often cause constipation and/or abdominal pain.
This is a well-known and documented side effect but it is usually only seen when using prescription iron tablets and capsules.
Because hypothyroidism already causes constipation it’s not ideal to worsen existing gut motility if at all possible.
The good news is that you can take iron without experiencing constipation if you use liquid iron instead of iron tablets.
Liquid iron also contains certain cofactors required for the absorption of iron in the intestinal tract (16) which can make it more effective than just taking iron by itself.
Iron is also notorious for disrupting the absorption of nutrients and even medications if you take them both at the same time.
And this extends to those who take iron for iron deficiency and thyroid medication for hypothyroidism.
Taking iron at the same time as your thyroid medication can inactivate your thyroid hormone and reduce how much makes it into your body!
You can avoid this issue by ensuring that you take your thyroid medication at least 2-4 hours AWAY from your iron supplement.
Because of this interaction, I usually recommend that patients take iron at the opposite time of the day as their thyroid medication.
If you take your thyroid medication at night then take your iron in the morning or vice versa.
You can also ensure better iron absorption by consuming Vitamin C or a glass of lemon water when you take your iron supplement.
If you are deficient, taking 1-2 teaspoons of liquid iron should be sufficient to help improve your iron levels.
You can see an example of liquid iron here and an example of iron capsules that you might want to consider if you can’t get down the liquid version due to taste or some other issue.
#5. Magnesium
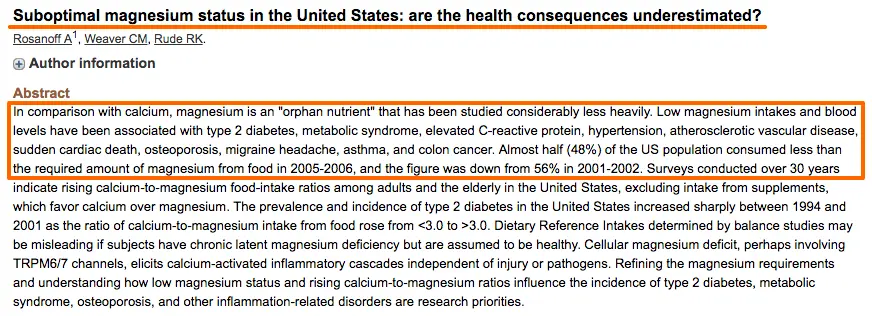
Magnesium is another big player for hypothyroid patients because hypothyroidism causes dysregulation of magnesium metabolism.
Hypothyroid patients may actually have normal serum and RBC magnesium levels but studies have shown decreased intracellular amounts of magnesium (17) in these patients.
That means you can’t always trust our limited laboratory tests when evaluating if you are deficient! (The same can be true of other serum ‘nutrient’ tests, which is why I don’t always rely on them).
These studies also show that both magnesium and zinc appear to be lower in hypothyroid patients due to increased clearance of both nutrients in the kidneys (18).
One thing is for sure:
You really don’t want to be deficient in this nutrient because a deficiency can cause a number of symptoms ranging from heart problems (19) (arrhythmia) to nervous system disorders.
What’s more concerning is that many patients in the USA, even those without thyroid issues, have suboptimal levels of this nutrient (20):
So how do you know if you should supplement with Magnesium or if you are deficient?
Follow the signs…
Symptoms of Magnesium deficiency include:
- Muscle cramps or eye twitches
- Anxiety or agitation
- Restless leg syndrome
- Sleep disorders ranging from insomnia to REM disturbances
- Poor nail growth
- See the full list here
Testing for Magnesium
I’m not a huge fan of magnesium testing simply because it is highly inaccurate, but if you prefer this route you are welcome to test for it.
The two most basic ways to test magnesium include:
- Serum magnesium – if using this test, you’ll want your results somewhere between 2.0 and 2.2 mg/dL.
- RBC magnesium – if using this test, you’ll want to ensure your results are somewhere between 6.0 and 6.8 mg/dL.
Both give you a general idea as to how much magnesium is floating around in your bloodstream but they don’t necessarily tell you if that magnesium is entering your cells (which is where you want it).
Because magnesium is so safe to use, it’s probably better to assume deficiency if you are symptomatic and to treat based on that knowledge.
Dosing Magnesium
Dosing magnesium is actually quite easy.
Most people do well and can sustain normal serum magnesium levels with a dose somewhere between 100mg and 200mg per day.
Some individuals may need less and some more, but somewhere in that range will work for 95+% of people reading this.
Reasons to increase your dose may include persistent symptoms of magnesium deficiency or chronic constipation.
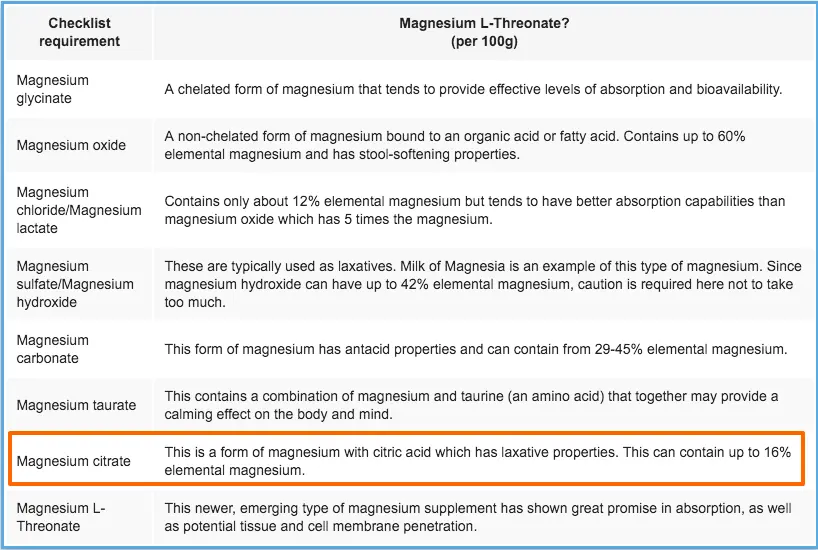
Types of Magnesium Available
There are many different types of magnesium supplements available for over-the-counter use.
The formulation that you want to stick to if you have thyroid disease is magnesium glycinate (a runner-up would be magnesium citrate).
Magnesium glycinate is highly absorbed and is ideal for getting enough magnesium into your body in a short period of time.
Glycinate should also not cause loose stools (like other forms of magnesium).
If you suffer from chronic constipation, however, you may want to consider using magnesium citrate.
This formulation leaves more magnesium in your GI tract which stimulates your bowels.
That means less magnesium will make it into your body, but it may help treat constipation.
When in doubt, start with 100 to 200mg of magnesium glycinate per day!
I would recommend getting your daily magnesium dose with your other thyroid support nutrients in something like this but you can also take a dedicated magnesium supplement if you feel you need even higher doses.
#6. Selenium
I’m sure you’ve heard about selenium if you have hypothyroidism and especially if you have Hashimoto’s thyroiditis.
Why?
Because not only is selenium involved in the T4 to T3 conversion process (21), but there are also some studies that show that supplementing with selenium can help reduce TPO antibodies (22).
How does selenium help improve these processes?
Selenium is a trace mineral that forms the backbone of a specific set of proteins known as selenoproteins.
These proteins catalyze important functions such as the creation of thyroid hormones and the creation of anti-oxidants in the thyroid gland (23).
Insufficient selenium levels may impair the function of these proteins and predispose you to develop low thyroid hormone and thyrocyte damage (damage to your thyroid cells).
Studies have shown that supplementing with selenium may help improve thyroid function and reduce thyroid antibodies by providing your body with this important mineral.
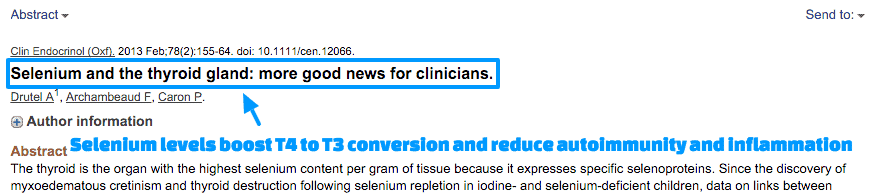
Sound pretty good right?
And, that’s not all…
Selenium is also a powerful anti-inflammatory agent (24) and using this nutrient may potentially help reduce inflammation (and autoimmunity) in certain patients.
You can find more information about symptoms of selenium deficiency and in-depth analysis here and how selenium helps improve your thyroid here.
Dosing Selenium
All patients with hypothyroidism and Hashimoto’s thyroiditis should be evaluated for selenium deficiency and treated if necessary.
Like zinc, a trial of selenium may be the best way to determine if you will benefit from using it.
Doses of at least 100 mcg per day have been shown to be effective (25).
But what about your dose?
Most of the nutrients we have discussed up until this point are fairly safe, even if used in large amounts.
But selenium is not one that you want to take more than necessary.
Doing so may cause negative symptoms such as hair loss, diarrhea, fatigue, and nail issues.
You can avoid these symptoms by keeping your daily dose between 70 mcg to 150 mcg per day.
As a thyroid patient, you will probably get better results by combining selenium with other minerals such as zinc and iodine.
For ease, combining your zinc, iodine, and selenium into one supplement makes a lot of sense.
You can always take them individually but just be sure you are getting the right doses and the right formulations of each.
#7. Probiotics
I think probiotics are a potentially easy and great way to boost your thyroid naturally.
But what do Probiotics and Thyroid function have in common?
A lot, it turns out.
For starters, about 20% of T4 to T3 conversion occurs in the gut (26).
What this means for you is that intestinal issues (more on those below) can negatively impact this percentage.
This may mean less free T3 and total T3 for your body.
In addition, inflammatory conditions in the gut (27) predispose the body to develop autoimmune diseases and worsening thyroid function.
So how do thyroid function and the gut play together?
It turns out that thyroid hormone helps the body produce stomach acid (which helps with digestion) and stimulates peristalsis, the slow movement of the GI tract.
Low thyroid hormone promotes low stomach acid which promotes intestinal issues, nutrient deficiencies, and the overgrowth of certain bacteria and fungi.
Low thyroid hormone also promotes a sluggish GI tract which predisposes the body to develop constipation, SIBO, and yeast overgrowth syndromes (like Candida).
Both syndromes cause inflammation which can promote autoimmunity and thus either directly damage the thyroid or lead to decreased T4 to T3 conversion.
Do you see the cycle here?
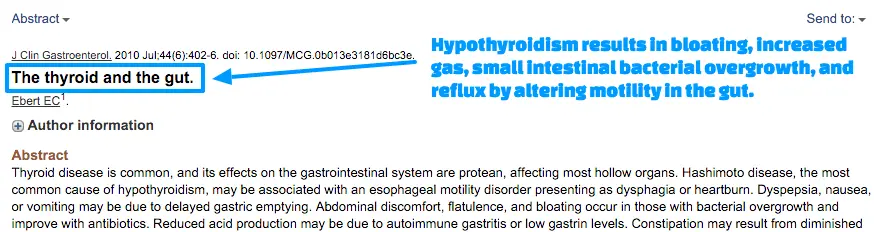
This is exactly why it’s so critical to evaluate and treat any GI-related issues that you may have because they are either caused by hypothyroidism and/or they are making your thyroid function WORSE.
Gut Issues that May Impact Thyroid Conversion
It’s easy to assume that your gut health is fine and is not dragging down your thyroid, but is that really the case?
You might assume that you have no intestinal issues, but it would be a good idea to really define what a healthy “gut” actually looks like.
If you have any of these symptoms (or conditions) then you may have gut issues limiting thyroid conversion:
- Gas or bloating
- Diarrhea
- Constipation
- Abdominal pain
- Acid reflux
- SIBO/SIFO (Small intestinal bacterial overgrowth, small intestinal fungal overgrowth)
- Inflammatory bowel disease
- Irritable bowel syndrome
- Increased intestinal permeability (Leaky gut)
- Multiple food sensitivities
- Celiac disease
Dosing & Frequency of Probiotics
I’d be lying if I said that taking probiotics will cure your GI problems, but they are certainly a good place to start.
Ultimately, you will probably need to alter your diet, change how frequently you are eating your food, and take additional supplements to fix your gut.
Probiotics play an important role in helping to regulate your intestinal bacterial concentrations, restoring gut lining integrity, and promoting appetite and hormone balance.
The use of specific probiotics can help improve or resolve many of these issues if you have them.
The key to using probiotics effectively is to use probiotics that contain the right species of probiotics at the right concentration (dose).
I’ve found the best success in thyroid patients by combining soil-based organisms, lacto and bifido species, and beneficial yeast.
You can see a perfect example of one that contains all 3 here.
This strategy is ideal for those with weight issues, multiple hormone imbalances, immune issues, Hashimoto’s thyroiditis, and other thyroid issues.
Ensure that your probiotic has several species of bifidobacteria (28) and lactobacilli species (29) as these species are the most well-studied.
#8. Proteolytic Enzymes
Enzymes make their way into the list because of how important they can be in helping your body break down nutrients but also medications.
As you already know, low thyroid = low stomach acid (30) = poor digestion.
But what you might not be aware of is how difficult it can be to break down certain medications (even thyroid hormone) when you have low stomach acid.
For this reason, in patients who have BOTH hypothyroidism (or Hashimoto’s) plus GI-related issues, I recommend that they also take enzymes to help with digestion.
In fact, I have seen some patients with Hashimoto’s who start taking NDT cause a temporary spike in antibodies as a result of this poor digestion.
Remember:
The inability to break down food products completely results in abnormal absorption of particles that your body isn’t used to seeing which may influence autoimmunity (31).
How to tell if you need it
I generally recommend a trial of enzymes with every meal (and in between meals) if you have Hypothyroidism or Hashimoto’s PLUS gut issues (GERD, IBS, IBD, chronic constipation, SIBO, or yeast overgrowth).
It’s also worth mentioning that taking enzymes in between meals can help promote the breakdown of immune complexes (30) in the bloodstream.
So take enzymes WITH food and WITHOUT.
You can get a comprehensive set of enzymes in this supplement.
#9. Iodine
Iodine is another nutrient that deserves a lot more attention than we can give it here (for more info please see this article) but I should at least mention its importance.
Stating that iodine is involved in thyroid hormone production is an understatement.
The iodine moiety on the thyroid hormone backbone is what makes it active.
In fact, 4 iodine molecules help create T4 and the removal of 1 iodine moiety by deiodinase enzymes can either activate or inactive thyroid hormone.
These deiodinases help regulate the conversion of T4 to T3 and help maintain cellular T3 activation (or inhibition).
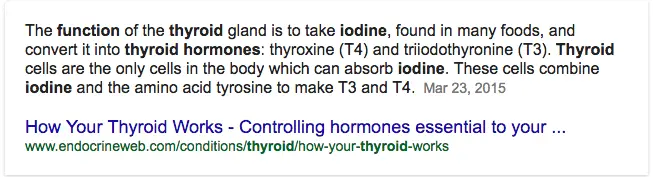
It should come as no surprise then that if you are deficient in iodine you will have problems creating thyroid hormone.
If you can’t produce enough thyroid hormone then you will experience the symptoms of hypothyroidism.
Iodine is an essential nutrient that humans MUST get from their diet (or supplements). We can not create it ourselves and we need it to function.
Insufficient iodine is associated with hypothyroidism and low IQ in newborns if the mother is deficient.
This is why the government places iodine in certain foods (such as salt).
The problem doesn’t come with knowing its importance but with understanding how to supplement it correctly.
Taking excessive iodine can be harmful to your thyroid gland while taking an insufficient amount can be damaging as well.
Iodine, like iron, is another nutrient you don’t want to have too much of, just like you don’t want to have too little.
Finding that balance can be difficult.
Another problem with Iodine supplementation is that it can displace other halides (31) which stick to thyroid hormone molecules but inactivate the thyroid hormone.
I’m talking about fluoride, bromide, and chloride.
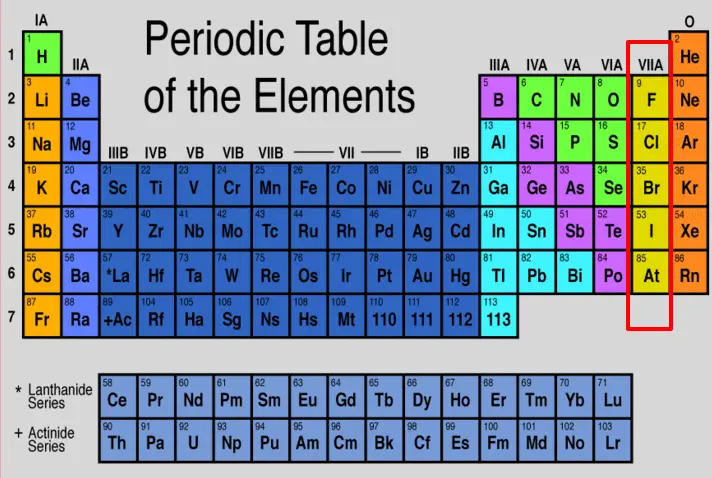
You can see from the image above that iodine, fluoride, chloride, and bromide all share a similar structure in terms of their electron outer shell.
What that means to you is that these other chemicals can displace iodine on thyroid hormone and cause cellular hypothyroidism with “normal” thyroid labs.
And, when you give a patient who has this issue iodine, it may displace the other chemicals and cause a detox reaction.
The detox reaction shares the symptoms of bromoderma and bromism (but usually not as severe).
The detox reaction can present as worsening thyroid symptoms, acne, pustules in the face, nausea/vomiting, irritability, etc.
These symptoms are often confused with a negative reaction to the iodine itself when in fact the symptoms are due to the detoxification of the other halides in the body.
Dosing Iodine & Safety for Thyroid Patients
Some people are hesitant to use iodine because they believe it is dangerous and that it may make their thyroid function worse.
This fear is largely unfounded, provided you use the appropriate dose of iodine.
There are several stories, even some on this blog, of patients reporting that taking high doses of iodine triggered Hashimoto’s in their bodies.
Some clinical studies also confirm that there is a relationship between the development of Hashimoto’s and iodine use (32).
My personal opinion is that iodine is not necessarily causing Hashimoto’s in these individuals but accelerating the disease which probably would have eventually established itself at some point in the future.
This potential outcome, while rare, can be avoided by taking iodine with other thyroid-protective nutrients such as selenium.
You can also protect against negative outcomes by taking a low to moderate dose of iodine and by avoiding excessively high doses.
Some people are able to take 25 to 50mg (milligrams) per day without any issues. These people often recommend that everyone takes doses in this range.
To put this into perspective, 1mg is equal to 1,000 mcg. So 25 mg of iodine is equal to 25,000 mcg or roughly 125x the dose that I recommend.
You may be able to titrate up to that dose without harm, but the potential negative effects outweigh the small potential benefit in my opinion.
Stick to doses of 75 mcg to 300 mcg per day and take your iodine with selenium and zinc and you shouldn’t have any issues.
Negative Iodine Reactions in Hashimoto’s Patients
Based on my experience, when iodine is dosed correctly, abnormal reactions are very rare.
While this is anecdotal evidence, it may calm your mind to know that out of thousands of people who have taken iodine very few reacted negatively to it.
If you start with a low dose (100-300 mcg per day) then you can easily reduce or stop taking iodine quite easily.
If you experience the side effects of bromism or bromoderma, then cut your dose and try again after several days.
Experiencing acne or a rash after taking iodine does not mean you don’t need iodine, but it may mean your dose is too high.
Thyroid Supplements are only Part of Treating your Thyroid
As I’ve mentioned above, these supplements can definitely offer therapeutic benefits to many patients…
But they shouldn’t be used alone.
Thyroid supplements should be used as part of a treatment plan that attempts to remove all negative stressors from life and put back in the things which your body lacks.
That means proper diet, stress reduction techniques, the right amount of sleep, and exercise are all JUST as (if not more important) than replacing these lost nutrients.
For more info on where to start adding in these other areas please see my post here.
To wrap it up:
These 9 Thyroid supplements, if used in the right scenario, can help boost thyroid function and help reduce your symptoms:
- Vitamin B12 (Remember you need either sublingual or injections)
- Adrenal support (Thyroid function and adrenal function are linked)
- Zinc
- Iron (You need just the right amount – not too much and not too little)
- Magnesium (Magnesium citrate for constipation, glycinate for hypothyroidism, and threonate for anxiety/depression)
- Selenium (Very helpful in patients with Hashimoto’s)
- Probiotics (Put preference on soil-based organisms, bifido and lacto strains, and beneficial yeast)
- Proteolytic enzymes (Helpful in digesting food and breaking down immune complexes)
- Iodine
Now it’s your turn:
Have you tried the supplements on this list?
If so, have they helped improve your thyroid? Why or why not?
Are you planning on using any of the supplements listed here? Why or why not?
Leave your questions or comments below!
Scientific References
#1. http://ajcn.nutrition.org/content/68/2/447S.abstract
#2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1395247/
#3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5015041/
#4. https://www.ncbi.nlm.nih.gov/pubmed/7776715
#5. http://www.ncbi.nlm.nih.gov/pubmed/18655403
#6. http://www.ncbi.nlm.nih.gov/pubmed/15681626
#7. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3520819/
#8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2503954/
#9. https://www.ncbi.nlm.nih.gov/pubmed/16261511
#10. http://www.ncbi.nlm.nih.gov/pubmed/8834378
#11. http://www.ncbi.nlm.nih.gov/pubmed/9701160
#12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746228/
#13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746228/
#14. https://www.ncbi.nlm.nih.gov/pubmed/29033409
#15. https://www.ncbi.nlm.nih.gov/pubmed/28634965
#16. https://www.ncbi.nlm.nih.gov/pubmed/6940487
#17. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC292768/pdf/jcinvest00264-0105.pdf
#18. http://www.ncbi.nlm.nih.gov/pubmed/3336286
#19. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4455825/
#20. http://www.ncbi.nlm.nih.gov/pubmed/22364157
#21. http://www.ncbi.nlm.nih.gov/pubmed/8834378
#22. http://www.ncbi.nlm.nih.gov/pubmed/11932302
#23. https://www.ncbi.nlm.nih.gov/pubmed/22009156
#24. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2721352/
#25. https://www.ncbi.nlm.nih.gov/pubmed/16837619?dopt=Abstract
#26. http://www.ncbi.nlm.nih.gov/pubmed/3049061
#27. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4036413/
#28. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4908950/
#29. https://www.ncbi.nlm.nih.gov/pubmed/28866243
#30. http://www.ncbi.nlm.nih.gov/pubmed/20351569
#31. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3266166/
#32. https://www.ncbi.nlm.nih.gov/pubmed/11751062/