This post will walk you through all of the causes of thyroid problems including Hyperthyroidism, Hypothyroidism, Goiter, Thyroid Cancer, and Nodules which all potentially may impact thyroid function in the body.
Thyroid disorders are incredibly common among individuals and any changes to thyroid function may result in serious symptoms that reduce the quality of your life.
Various symptoms such as weight gain, depression, fatigue, and hair loss may result from thyroid dysfunction.
We will also discuss the pitfalls of diagnosing and treating thyroid-related problems and why many people still remain symptomatic despite taking thyroid medication.
Let’s dive in:
Types of Thyroid Disorders
Why do we even care about thyroid disorders?
Because your thyroid could be considered the “master hormone” in the body which regulates and helps control various other hormones and metabolic functions.
Thyroid hormone is produced through an endocrine gland that sits in your neck.
It produces thyroid hormone which enters the bloodstream and impacts almost every cell in your body.
Small changes to circulating thyroid hormones in the bloodstream may result in big symptoms in your body.
One of the big issues with thyroid-related problems is that they are incredibly common with up to 1 in 5 people in the United States experiencing some type of thyroid-related issues (1).
So what types of symptoms might you experience if you have thyroid problems?
The symptoms can certainly vary but because the thyroid hormone helps regulate your body weight one of the most common symptoms is that patients with thyroid problems experience changes in their weight.
This could be manifested as an increase in weight (usually the result of low thyroid hormone) or a decrease in weight (usually the result of excess thyroid hormone).
Patients also may experience changes to how they tolerate certain conditions such as cold or heat and they may experience cosmetic changes such as hair loss, dry skin, and damage to their nail beds.
The bottom line is that thyroid hormone helps control how you feel on the inside and how you look on the outside – making it one of the most important hormone systems in the body.
With that in mind let’s discuss the various types of thyroid problems that can exist and which symptoms may be associated with these conditions.
(I’ve only given you a brief outline of SOME of the symptoms associated with thyroid disease above)…
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Hypothyroidism
One of the most common types of thyroid problems is hypothyroidism.
Hypothyroidism is a thyroid problem that is the result of LOW circulating thyroid hormone in the blood and the body.
Hypothyroidism is often referred to as having a “sluggish thyroid” or a “slow thyroid” and these are all names for the same condition.
We will talk more about what causes hypothyroidism below (because it is the most common cause of thyroid problems) but for now, just realize that there are many conditions that may result in a decreased production of thyroid hormone in the body.
When thyroid hormone in your blood starts to decrease your body compensates by increasing another prohormone known as TSH or thyroid stimulating hormone.
Most patients are diagnosed with hypothyroidism based off of this blood test (TSH).
The confusing part about TSH is that it tends to INCREASE when the thyroid hormone in the blood DECREASES.
It’s not necessarily intuitive but this has to do with the feedback loops that exist in the body (2).
You can think of this scenario in the following way to help it make sense:
When thyroid hormone levels fall (because your thyroid can’t produce enough hormone) your body reacts by increasing the TSH in an attempt to “scream” at the thyroid gland to make more hormone.
But if the thyroid is damaged (for any reason) then obviously it isn’t able to produce enough hormone even though the pituitary gland is yelling at it to make more.
This results in a low thyroid hormone and some very nasty symptoms that often lead patients to the doctor’s office.
Symptoms of Hypothyroidism:
- Weight gain
- Fatigue or low energy
- Dry skin
- Skin Rashes
- Acne
- Low heart rate
- Low body temperature
- Cold extremities
- Constipation
- Cold intolerance
- Menstrual irregularities
- Infertility
- Depression
- Chronic pain or muscle aches
- Hair loss
- Fingernail damage
Believe it or not, this isn’t even a complete list of symptoms.
Because thyroid hormone (remember it’s the master hormone) has an action on almost every cell in your body the symptoms of low thyroid hormone tend to be widespread.
Another important point is that these symptoms almost always vary between individuals.
What I mean is this:
Let’s say 2 people have hypothyroidism and they are both experiencing weight gain as a result of this condition.
The first person may only experience a small weight gain of 5-10 pounds while the other person may experience a weight gain of 30-40 pounds.
This has to do with the DEGREE and the amount of damage that exists in their body.
You can consider thyroid hormone function on a spectrum from 0% to 100%.
In this model, you can have only a slight reduction in thyroid hormone (something like 90%) and still feel relatively normal.
On the other hand, you can have a severe reduction in thyroid hormone (something like 20-30%) and feel terrible.
The bottom line is that each person is unique and different and the quality and severity of their symptoms may vary.
Hypothyroidism Treatment
Because hypothyroidism is the result of low thyroid hormone in the blood it makes sense that the treatment for this condition would be with additive thyroid hormone taken by mouth.
Thyroid hormone medication (more on that below) is the treatment of choice if you are suffering from LOW thyroid function or hypothyroidism.
The amount of thyroid hormone that you take, the dosage, and what time of day you take your medication depends on a number of factors and it’s not something we will go into here but you can read more about using the various types of thyroid medication below:
- T4-only thyroid medication such as Synthroid, levothyroxine and Tirosint
- NDT medications such as Armour thyroid, WP thyroid, and Nature Throid
- T3-only medication such as Cytomel or liothyronine
Hyperthyroidism
Another important cause of thyroid disease among patients is hyperthyroidism.
You can think of hyperthyroidism as the exact opposite of hypothyroidism.
In this condition, your body actually creates TOO much thyroid hormone which means that there is an excess of circulating thyroid hormone (3) floating around in your bloodstream.
This excess of thyroid hormone causes overstimulation of your cells and thyroid receptors which results in specific and characteristic symptoms.
You may find that these symptoms are almost the exact opposite of those associated with hypothyroidism and that makes sense given the pathophysiology of the disease.
Another important point about hyperthyroidism is that lab tests tend to be the opposite of hypothyroidism as well.
Hyperthyroid patients often experience low or suppressed TSH (very close to zero).
They often experience elevated free serum T3 (compared to hypothyroid patients who generally have low T3 in the serum).
Hyperthyroidism is not as common as hypothyroidism and is most often caused by the autoimmune condition Graves’ disease.
This disease results in the production of antibodies (known as thyroid-stimulating immunoglobulins) which sit on and “activate” thyroid hormone production in the body.

Other common causes include toxic multinodular goiter and certain types of thyroid cancers that produce thyroid hormones.
Hyperthyroidism Treatment
In many cases, the treatment for hyperthyroidism is to attempt to block the effect of thyroid hormone on the tissues or to simply remove the source of thyroid hormone production.
If you suffer from difficult-to-treat Graves’ disease or other causes of hyperthyroidism then the treatment may include the complete removal of your thyroid gland through surgical means or the ablation of your thyroid gland with radioactive iodine – both treatments result in a reduction in thyroid hormone production.
The interesting part of hyperthyroidism treatment is that most therapies actually render the patient hypothyroid (5)!
This concept can be confusing for some patients but don’t let it be for you.
If you remove your thyroid gland, the primary source of thyroid hormone in your body, doesn’t it make sense that you will then require thyroid hormone medication?
And if you go back to our treatment of hypothyroidism you will notice that the treatment for hypothyroidism is with thyroid medication.
Symptoms of Hyperthyroidism:
- Weight loss
- Heat intolerance
- Rapid heart rate
- Heart palpitations
- Exercise intolerance
- Shortness of breath
- Increased sweating
- Hair loss
- Dry brittle hair
- Diarrhea
- Anxiety
- Insomnia
- Menstrual irregularities
- Panic attacks
- Increased appetite
- Feeling flushed or hot flashes
Thyroid Goiter
The term goiter is used as a term simply to describe the SIZE of your thyroid.
It’s not an illness by itself and it can be seen in patients who have completely normal thyroid function (patients who fit into this category are called “euthyroid”).
An enlarged thyroid gland (goiter) is also seen in patients who have both hypothyroidism and hyperthyroidism.
So more than a diagnosis by itself, it’s more of a way to describe the size or shape of your thyroid gland and doesn’t necessarily give you enough information by itself.
It’s still important to talk about because it is a thyroid condition, but just realize that it is not a specific disease by itself.
In addition, it is also an incredibly common condition that may be silently present in your body until you undergo a physical exam by a Doctor.
Some studies show that up to 20-30% of people may have a Goiter (6) (usually the result of a benign thyroid nodule).
A goiter is often felt or “palpated” by your doctor during a physical exam of your neck.
It can also be seen as an enlargement of your neck or even cause difficulties in swallowing or speech (depending on the size).
Despite the condition being prevalent there is a surprisingly small amount of research and knowledge on this topic.
We know that the following conditions cause goiter:
- Iodine deficiency (7) (probably the most well-known, understood, and preventable cause of Goiter)
- Thyroid Cancer
- Autoimmune Thyroiditis
- Inflammatory causes of Thyroiditis
- Thyroid Cysts
You can see that pretty much any condition that increases the size of the thyroid gland will cause the Goiter condition.
Beyond the causes listed above, it seems that certain individuals (through genetic variations) seem to be more susceptible to developing goiter than others.
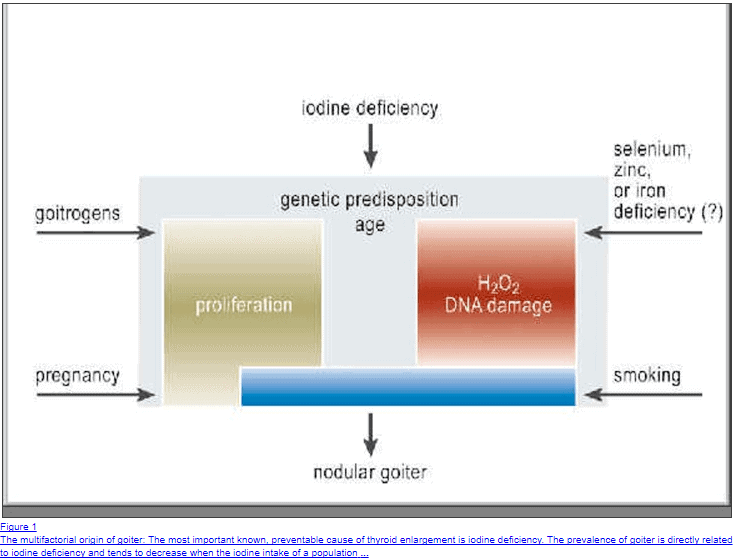
It also seems that the condition is usually multifactorial in origin which means that multiple conditions probably cause enlargement of the thyroid gland.
Symptoms of Thyroid Goiter:
- Not necessarily symptomatic by itself unless it is very large in which case it might cause swelling in the neck or difficulty with swallowing
- May be associated with conditions that cause both the symptoms of hyperthyroidism and hypothyroidism (depending on the cause of the goiter)
- Symptoms may vary from individual to individual
- Size and symptoms may be able to be managed with the use of natural therapies (to a variable degree)
Thyroiditis
Thyroiditis is a term used to describe inflammation in the thyroid gland and it can be from any cause.
Thyroiditis is really a non-specific term and not really a diagnosis in of itself and instead of focusing on the fact that there is inflammation present in the gland you should focus on the CAUSE of that inflammation.
Believe it or not inflammation, or thyroiditis is actually quite common as a result of autoimmune diseases.
We’ve previously discussed both Hypothyroidism and Hyperthyroidism and the most common causes of both of these diseases are autoimmune diseases which also result in thyroiditis (inflammation of the thyroid gland).
The most common cause of thyroiditis leading to hyperthyroidism is the autoimmune disease known as Graves’ disease.
The most common cause of thyroiditis leading to hypothyroidism is the autoimmune disease known as Hashimoto’s thyroiditis.
Both of these disease states result in the production of antibodies that attack your own thyroid gland.
The end result of this attack is inflammation and damage to the thyroid gland.
In the case of Graves’ disease, the antibodies are called Thyroid-stimulating immunoglobulins, and these antibodies actually “stimulate” or “activate” the thyroid gland which results in the release of thyroid hormone.
The antibodies in Hashimoto’s thyroiditis are known as anti-TPO antibodies and thyroglobulin antibodies which attack a different portion of the thyroid gland.
Hashimoto’s is a serious condition that may result in permanent damage to your thyroid gland and result in reliance upon thyroid medication – it’s also the #1 cause of hypothyroidism in the United States.
The confusing part about Thyroiditis is that it can result in both HYPER and HYPO thyroid symptoms, depending on what is happening in your thyroid gland.
Inflammation itself is damaging to the thyroid gland which may cause the release of thyroid hormones and result in hyperthyroid symptoms.
On the opposite end of the spectrum, thyroiditis can also result in PERMANENT damage to the thyroid gland which results in decreased thyroid hormone production and thus hypothyroidism (take for instance the example of end-stage Hashimoto’s thyroiditis).
There are also many other causes of Thyroiditis including pregnancy-related thyroiditis, viral and bacterial infections, and so on.
I’ve only discussed the most common causes here but you can read about a more extensive list of thyroiditis causes, symptoms, and treatment here.
Symptoms of Thyroiditis:
- May alternate between Hypothyroidism and Hyperthyroidism symptoms depending on the cause of Thyroiditis and throughout the course of the disease (please see the lists above) – it’s not uncommon for patients to initially present with the symptoms of hyperthyroidism followed by the symptoms of hypothyroidism
- Occasionally Thyroiditis may result in swelling of the neck, difficulty swallowing, and even pain
Thyroiditis Treatment:
The treatment for Thyroiditis really depends on the cause and the focus is almost always on the symptoms associated with the disease.
For instance:
If you have Thyroiditis and you are experiencing the symptoms of Hyperthyroidism then a beta blocker prescription may help to reduce some of those symptoms.
On the other end of the spectrum and if you are experiencing thyroiditis which results in Hypothyroid symptoms then you may need thyroid hormone medication or thyroid hormone replacement therapy.
Remember though that many cases of Thyroiditis may resolve without any treatment whatsoever – it just depends on what is causing the inflammation.
Thyroid Cancer
Thyroid cancer is another very important cause of thyroid problems among many patients.
Thyroid cancer is the most common endocrine (meaning hormonal) malignancy and it is increasing in incidence each year.
Fortunately, the most common form of thyroid cancer is also the least aggressive and it is known as papillary thyroid carcinoma (8).
Most forms of thyroid cancer are thought to arise from thyroid nodules (discussed below) which may indicate early changes which lead to an increased risk of developing thyroid cancer.
Other thyroid conditions such as chronic inflammation, thyroiditis, and even damage to the thyroid (such as radiation) may increase the risk of developing thyroid cancer.
The good news is that the 5-year survival rate for thyroid cancer is around 97 to 98% (9).
This survival rate is thought to be due to our ability to catch thyroid cancer early with proper imaging techniques and evaluation of thyroid nodules which may be precancerous in some people.
Thyroid cancer usually doesn’t present with changes to circulating thyroid hormones in the blood and body, but it may cause other issues more typical of general cancers (such as swelling of the lymph nodes and so on).
Discussing thyroid cancer in this post is important because the typical treatment for thyroid cancer is known as complete thyroidectomy (10).
Thyroidectomy means the complete removal of the thyroid gland.
Because the thyroid gland is critical to functions such as metabolism, energy production, heart rate, and body temperature the removal of the thyroid requires the replacement of thyroid hormone through the use of medication.
So the symptoms associated with thyroid cancer tend to be secondary to the treatment OF the condition and not CAUSED by the cancer itself.
Patients who have undergone a complete thyroidectomy (meaning complete removal of the thyroid gland) will need thyroid hormone medication replacement therapy for the rest of their lives.
The reason for this is that without any thyroid hormone in your body it may lead to coma and death.
Symptoms of Thyroid Cancer:
Thyroid cancer may not cause problems directly with your thyroid gland and it may not interfere with the production of thyroid hormones.
However, if it grows large enough then it may produce symptoms which are related to swelling and local compression of various anatomical structures in your neck which may result in the following symptoms:
- A visible or palpable “mass” in the thyroid gland
- Swollen lymph nodes in the neck area
- Pain in the thyroid gland
- Pain when swallowing
- Difficulty when swallowing
- Changes to your voice or hoarseness
- Constant nonproductive cough
Thyroid Nodule
The term thyroid nodule is used to refer to a “nodule” or mass that is present on the thyroid gland itself.
This condition is actually incredibly common and it is estimated that up to 3 to 7% of the world’s population has a palpable thyroid nodule (11)!
To put this into perspective that’s anywhere between 228 million to 523 million people who may have a thyroid nodule!
Does that mean that all of these people will have thyroid problems?
No, in fact, most of them probably won’t experience any symptoms related to their nodule.
Most nodules aren’t even monitored unless they are larger than 1 cm in size.
The reason we get concerned about thyroid nodules is not necessarily because they are bad by themselves but because they can be an early sign of thyroid cancer and because they may be “active” or secrete hormones in some individuals.
It is estimated that up to 5% of all thyroid nodules may be cancerous which is about a 1 in 20 chance.
Because of this, it is important to identify if you have a thyroid nodule and get appropriate screening to monitor and make sure that it is not growing and to ensure that it doesn’t have “characteristic signs” of thyroid cancer.
The combination of history, physical exam, and thyroid lab testing can help determine how to proceed as seen below:
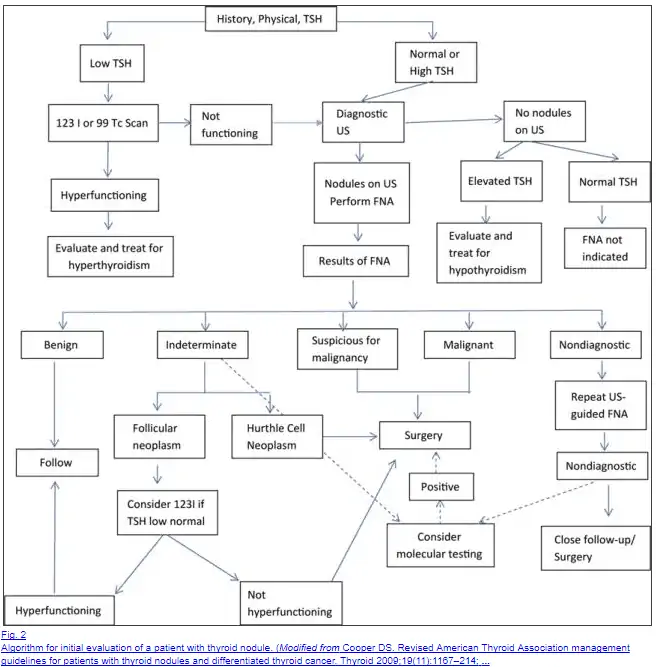
Screening can be done through imaging studies such as ultrasound and CT but some cases may require a biopsy to help determine if the nodule is cancerous or not.
Now that we understand what a Thyroid nodule is we can discuss what causes them:
You can think of thyroid nodules as an overgrowth of thyroid glandular tissue.
This type of growth can occur as a result of a nutrient deficiency (such as iodine deficiency), chronic inflammation (such as thyroiditis), physical damage to the thyroid gland (such as trauma or radiation), and even genetics.
The exact reason that you may have a thyroid nodule may not be uncovered or may be considered to be “idiopathic” which is to say we don’t know for sure.
The main goal in “treating” a thyroid nodule is to monitor its presence and to make sure that it doesn’t grow over time.
You can reduce the risk of developing a thyroid nodule by actively treating those conditions listed above which may lead to a thyroid nodule.
Symptoms of Thyroid Nodule:
- Most thyroid nodules may go unnoticed by the patient until they are palpated by a Doctor on a physical exam. Rarely thyroid nodules may be large enough to cause symptoms such as compression of the vocal cords or compression of the airway which may require treatment.
- Some thyroid nodules may actually produce thyroid hormone which may result in the symptoms of Hyperthyroidism.
Causes of Hypothyroidism (The most Misunderstood Thyroid Disorder)
We briefly discussed hypothyroidism (the first section of this post) but it’s important that we spend more time and dive into the specific causes of hypothyroidism.
The reason for this is simple:
Hypothyroidism (remember that’s the thyroid disease that results in a REDUCTION of thyroid hormone) is probably the most difficult-to-treat thyroid problem that we are discussing.
The reason for this has to do with thyroid hormone medication and replacement.
There are a number of ways to replace thyroid hormone in the body and each person will require a unique type of thyroid medication and dose.
Another important reason to discuss hypothyroidism in detail is that many of the causes of hyperthyroidism ultimately result in hypothyroidism and reliance on medication.
Consider the case of Graves’ disease which is treated with radioactive iodine ablation therapy.
This condition results in damage to the thyroid gland (intentionally) which ultimately leads to reliance upon thyroid medication because the gland no longer functions appropriately.
This is a good thing because it may help to reduce the symptoms of Graves’ disease but it may lead to other symptoms down the line.
The same concept holds true for patients who undergo a complete thyroidectomy.
Obviously, if the entire thyroid gland is removed then it will no longer function properly and that person will again require thyroid hormone replacement therapy.
So with that in mind let’s discuss the potential causes of hypothyroidism:
#1. Autoimmunity
Among the many causes of hypothyroidism, the most common cause is the autoimmune disease known as Hashimoto’s thyroiditis (12).
This disease results in inflammation (and if you recall from above that means it falls into the “thyroiditis” section) which may cause long-term, permanent and irreversible damage to your thyroid gland if not treated.
Autoimmune diseases cause damage to your own tissues because of miscommunication between your own cells and your immune cells.
There is a lot of debate as to what triggers autoimmunity but we do know that certain factors tend to increase your risk of developing these conditions.
Factors such as increased stress, environmental exposure, certain viral/bacterial infections, and changes to the intestinal microbiome all seem to increase your personal risk of developing Hashimoto’s and other autoimmune conditions.
One big problem with autoimmune disease (especially of the thyroid) is that we don’t have very good conventional treatments.
Most physicians opt to take a “wait and see” approach to treatment.
This approach is exactly as it sounds.
Physicians may opt to “watch” thyroid function over time and once the thyroid gland is destroyed they may then put the patient on thyroid medication.
Because of this, many patients have been led to alternative therapies including certain supplements, dietary changes, lifestyle changes, and other therapies which can be effective.
Some therapies are more effective than others and some have scientific reasons why they may be effective, but each person tends to respond differently to these therapies.
You can read more about natural treatments for Hashimoto’s and how to lower thyroid antibodies here.
#2. Nutrient Deficiencies
Another important cause of thyroid dysfunction is nutrient deficiencies.
It may surprise you to know that as many as 13 different nutrients are all required for optimal thyroid function in the body.
Nutrients such as zinc, selenium, and iodine are all incredibly important and deficiencies in any of these 3 nutrients may lead to decreased thyroid hormone production and peripheral thyroid conversion.
Zinc has been shown to be involved in thyroid conversion (13) and supplementation (if combined with selenium) may improve thyroid function.
Studies also indicate that zinc deficiency (14) may be more common than we think and may be one of the potential causes of subclinical hypothyroidism.
Another important nutrient required for thyroid hormone synthesis is Iodine.
Iodine helps form the structure of thyroid hormone and helps define the biological activity of each thyroid hormone.
T4 has 4 iodine moieties while T3 has 3 iodine moieties and it is the changing of these iodine subgroups that either “activate” or “inactivates” thyroid hormone in the serum.
And the primary source of Iodine for Humans is through diet (15) (which means that in order to get enough you need to be either consuming iodinated salt or consuming sea vegetables weekly!).
Because many people are not consuming sea vegetables on a regular basis many patients may have sub-optimal iodine stores in their bodies which may compromise thyroid function.
Supplementing with certain nutrients may help improve thyroid function.
You can learn more about using Zinc and selenium to potentially improve thyroid function here.
You can read more about the importance of iodine and how to supplement correctly and safely here.
#3. Medications
Medications may also be another important cause of thyroid dysfunction leading to hypothyroid-like symptoms in certain people.
Medications known to interfere with thyroid hormone in the body include blood pressure medications, anti-seizure medications, diabetic medications, and medications designed to treat depression and anxiety (16).
While you may not necessarily be able to completely eliminate the medications you are taking it may be worthwhile to discuss alternative options with your Doctor.
Sometimes even switching to a different medication to treat the same condition may improve thyroid function.
#4. Surgery/Radioactive Iodine Ablation
Another very common cause of hypothyroidism is actually secondary to treatments designed to treat hyperthyroidism, thyroid cancer, and other thyroid disorders.
Surgery designed to remove part or all of your thyroid will result in reduced thyroid function in the body.
Likewise, other procedures such as Iodine ablation therapy will also damage your thyroid gland and result in reduced thyroid hormone production.
These therapies may be necessary, but just realize that they WILL result in hypothyroidism simply because they are damaging the thyroid gland.
Another important cause of hypothyroidism is the medication methimazole which is designed to reduce peripheral T4 to T3 conversion.
#5. Pituitary Issues
Your pituitary secretes the very important hormone known as TSH (or thyroid stimulating hormone).
This is important because certain conditions may result in damage to your pituitary gland which may cause problems in TSH production.
This is an uncommon cause of hypothyroidism because most of the time the damage to your thyroid “system” is at the level of the thyroid gland, but it’s still worth discussing.
Damage to the pituitary may result in reduced TSH and therefore reduced thyroid hormone production from the thyroid gland.
Remember how the thyroid is supposed to work:
TRH is secreted from the Hypothalamus which then tells the pituitary to secrete TSH which then tells the thyroid gland to produce thyroid hormones.
Circulating thyroid hormones then circle back and help regulate the entire system.
You can basically have problems at any given point in that entire system, it just so happens that MOST problems occur directly in the gland itself.
Conditions such as prolactinomas (17), pituitary masses (18), and even trauma (19) may result in reduced TSH secretion and therefore hypothyroidism.
#6. Hypothalamic issues
Your hypothalamus is another hormone regulator found 1 step higher than the pituitary gland in the Hypothalamic-pituitary-thyroid axis.
Damage to the hypothalamus, much like the pituitary, may result in reduced TRH which then may result in reduced TSH which then may result in reduced thyroid hormone production in the body.
Hypothalamic damage is not as common as other thyroid disorders that directly damage your thyroid gland but like pituitary damage, it is included here for completeness.
Certain disorders such as Hypothalamic obesity disorder (20) may be caused by repetitive yo-yo dieting which may cause damage to your thyroid gland.
This is a relatively new condition so it is not well understood, but you can read more about how it may alter thyroid function in this post.
#7. Genetic Issues
Lastly, it’s important to realize that all of us are designed to be genetically different.
The amount of thyroid hormone that you produce is different from the amount that I produce.
The amount of thyroid hormone that YOU convert at any given time is different from the amount that I convert at any given time.
These genetic differences mean that the amount of thyroid hormone in our bodies will be slightly different.
No one disputes this fact but physicians tend to forget this genetic component when treating patients.
For instance:
This idea may explain why certain patients simply don’t respond to conventional or typical thyroid hormone treatment.
We are also beginning to discover various genetic differences and SNPs that may account for different thyroid hormone activity in each individual (22).
The idea here is that you want to make sure that your treatment is tailored to your body and your genetics which means that you may not fit the “standard” mold.
Does your Doctor “Get it”?
The complexities we have discussed here are very important because they may impact your treatment.
Unfortunately, many physicians tend to follow a very standard pattern of treatment which includes TSH testing and thyroid hormone management.
This approach may not take into account critical factors and may lead to patient dissatisfaction (23).
Does this sound like a familiar scenario…
You go to the doctor’s office because you are feeling fatigued, and constipated, you have dry skin, hair loss, and weight gain and you are sure that your thyroid is at fault.
Your doctor orders a test but assures you that your “thyroid is fine”.
Chances are high that your doctor ordered only the TSH (or thyroid stimulating hormone) and is using this as a way to evaluate the complex thyroid system in your body.
It turns out that, while TSH is important, it doesn’t accurately tell you what is going on with the thyroid in the whole body.
It only tells you what is happening to the pituitary gland.
That would be ok but the pituitary gland has important differences from the cells in your body and it is the last tissue in your body to feel the effects of low thyroid hormone (this is due to differences in deiodinase enzymes which can either “activate” thyroid hormone or “inactivate” thyroid hormone).
This means that by the time your doctor picks up on your sluggish thyroid using the TSH it is very possible that other cells in your body may have had insufficient thyroid hormone for a long time.
A better approach to thyroid patient management is to evaluate the other factors that we have discussed above including thyroid hormone conversion status, genetic issues, lifestyle issues that may contribute to thyroid dysfunction, and so on.
Evaluating your thyroid in this way requires a more comprehensive approach including more comprehensive lab testing which we will go over below:
| Symptoms of Hypothyroidism | ||
| o Fatigue | o Swelling of eyelids | o Emotional instability |
| o Lethargy | o Dry skin | o Choking sensation |
| o Low endurance | o Dry mucous membranes | o Fineness of hair |
| o Slow speech | o Constipation | o Hair loss |
| o Slow thinking | o Weight gain unexplainably | o Blueness of skin |
| o Poor memory | o Paleness of lips | o Dry, thick, scaling skin |
| o Poor concentration | o Shortness of breath | o Dry, coarse, brittle hair |
| o Depression | o Swelling | o Paleness of skin |
| o Nervousness | o Hoarseness | o Puffy skin |
| o Anxiety | o Loss of appetite | o Puffy face or eyelids |
| o Worrying | o Prolonged menstrual bleeding | o Swelling of ankles |
| o Easy emotional upset | o Heavy menstrual bleeding | o Coarse skin |
| o Obsessive thinking | o Painful menstruation | o Brittle or thin nails |
| o Low motivation | o Low sex drive | o Dry ridges down nails |
| o Dizziness | o Impotence | o Difficulty in swallowing |
| o Sensation of cold | o Hearing loss | o Weakness |
| o Cold skin | o Rapid heart rate | o Vague body aches & pains |
| o Decreased sweating | o Pounding heartbeat | o Muscle pain |
| o Heat intolerance | o Slow pulse rate | o Joint pain |
| o Non-restful sleep | o Pain at front of the chest | o Numbness or tingling |
| o Insomnia | o Poor vision | o Protrusion of one or both eyeballs |
| o Thick tongue | o Weight loss | o Sparse eyebrows |
| o Swelling of face | o Wasting of tongue |
How do you Test for Thyroid Related Problems?
The best way to approach thyroid evaluation is to look at multiple points.
To do this we can take advantage of our knowledge of thyroid physiology and how it works.
For instance:
We know that the thyroid helps to control metabolism and heart rate.
We can, therefore, use markers such as your basal metabolic rate (24) (the number of calories that you consume) and your resting heart rate (25) to help us evaluate if the thyroid is working optimally.
It makes sense that those people with low thyroid function would present with a lower resting heart rate and a slower metabolism than those with normal thyroid function.
Not only does it make sense but it is also shown to be true in several clinical studies (26)!
In addition to evaluating these factors, we also want to assess thyroid serum lab tests, assess a complete set of symptoms and look at other factors that may influence thyroid function.
Compare this approach to the one-dimensional and conventional thyroid testing which includes only one lab test – the TSH.
Again, all of these tests have been used in other studies and are derived from our basic understanding of thyroid physiology so we can count on them being accurate, especially when used together.
If you feel you have thyroid problems then consider using this 4-step approach:
Step #1 – Assess Serum Thyroid Lab Tests
- Check the TSH – If your TSH is > 2 then you are hypothyroid. A TSH < 2 does not rule out hypothyroidism.
- Check Free T3 – This value should be in the upper 1/3 of the reference range.
- Check free T4 – This value should also be in the upper 1/3 of the reference range. A high T4 with a lowish T3 and reverse T3 > 15 may indicate thyroid at the cellular level.
- Thyroid antibodies – Antibodies > 30 need to be addressed by cooling down the immune system and providing the correct nutrients.
- Reverse T3 – This value should be < 15.
- Free T3 to reverse T3 ratio – Values < 0.2 indicate a conversion problem of T4 to T3 and are usually associated with states like insulin resistance, leptin resistance, obesity, fatigue, depression, and medications that slow down your metabolism (narcotics, antidepressants, etc.)
- Sex hormone binding globulin – This value should be > 70 in women and > 30 in men. This allows me to see how well your tissues are responding to the current levels of thyroid hormone floating around in your body.
Step #2 – Assess Symptoms
Your clinical symptoms can also be a clue as to what is happening in your body.
If you are experiencing weight gain or fatigue from thyroid dysfunction then it makes sense that those symptoms should IMPROVE as you take thyroid medication or if you undergo treatment.
If your symptoms are NOT improving then this may be a sign that you are either not on the right track, not on the right medication or that there is some other issue causing these problems (such as problems unrelated to thyroid dysfunction).
Over 70 years ago it wasn’t uncommon for physicians to dose thyroid hormone based on symptoms alone, but now we have more sophisticated ways to determine thyroid status in the body.
The point here though is that you should listen to the cues from your body and use them to help guide treatment (just don’t use them without the other steps).
Step #3 – Assess Basal Body Temperature and Basal Metabolic Rate
Your basal body temperature can be used as a surrogate marker for your metabolism.
Consider this simplified process:
Your cells produce energy, and this energy is released as heat, and this release of heat helps to set your body temperature.
Certain conditions (such as hypothyroidism) can REDUCE the amount of energy that you produce which may then cause your body temperature to be lower than normal through the process above.
Because of this, you can use your body temperature (and resting heart rate) as a way to evaluate thyroid status.
Your body temperature should be around 97.8 degrees first thing in the morning.
If it is less than 97.8 and you have hypothyroid symptoms or a known diagnosis of hypothyroidism, then it’s possible that your low body temperature may be due to insufficient dosing of thyroid medication.
Above is a typical representation of basal body temperature before and after thyroid treatment over the course of 1 month – just to give you an idea of the importance of thyroid function on body temperature.
You can clearly see the variability at the beginning of the month which is classic for patients suffering from thyroid disease.
Over 3-4 weeks of consistent thyroid hormone replacement therapy (Armour thyroid in this case) the body temperature levels out and becomes much more consistent.
It should be pointed out that while your body temperature can be helpful it should never be used alone because many other conditions (such as ovulation) may alter body temperature.
Instead, it should be used as part of a complete plan, particularly for patients with difficult-to-diagnose and manage thyroid diseases.
Step #4 – Assess Other Factors that Influence Thyroid Function
We’ve previously discussed other factors which influence thyroid regulation but there are many others worth discussing.
These factors include cortisol levels, iron status, and other nutrients.
All of these factors, while separate from your thyroid, may influence thyroid hormone receptor activity, conversion status, and so on.
Because of this interaction, it’s important to focus on your overall health instead of laser-focusing on just thyroid function.
If you have deficiencies in these areas (which is common in MANY people) you may have thyroid hormone in the blood but it’s not working at 100% capacity – leaving you with thyroid symptoms.
In addition, lifestyle factors such as stress management, diet, sleep schedule, and exercise routines can be adjusted to help improve hormone regulation in your body.
You can learn more about natural approaches to thyroid management in this post.
How do you Treat Thyroid Related Problems?
Treatment of thyroid-related problems is highly variable and highly individualized.
Whenever possible the goal of treatment should be to address and reverse the underlying causes of thyroid dysfunction in the body.
This isn’t always possible in every patient, but it doesn’t mean that you should ignore factors outside of typical thyroid hormone replacement.
Consider the following therapies that may potentially improve your thyroid status:
- Bioidentical T3 therapy (Sustained Release or rapid-acting like Cytomel or liothyronine) – This medication is preferred in certain conditions such as thyroid resistance, obesity, leptin resistance, insulin resistance, diabetes, fibromyalgia, and weight loss resistance.
- Bioidentical T4 + T3 therapy – Each amount can vary and allows for a tailored medication for each patient.
- Natural Desiccated Thyroid hormone (Armour Thyroid, Nature-Throid, WP Thyroid, etc.) – Porcine-derived T4 and T3 combinations.
- Bioidentical T4 therapy alone (like Synthroid, levothyroxine or Tirosint)
- Dietary Intervention: Certain foods, such as those high in goitrogens, may impact thyroid function. Other diets such as the AIP diet may help reduce antibody levels.
- Targeted Supplementation: Nutrients such as Zinc, Selenium, Iodine, and Iron may help improve thyroid function.
- Stress Management: Stress may play a role in peripheral thyroid conversion through its effects on gastrointestinal function. Managing stress can also help improve energy levels and hormone balance (27).
Final Thoughts
There are many different types of thyroid problems that can occur as a result of thyroid dysfunction in your body.
The first step in diagnosing a thyroid problem is to start with your symptoms and then move to lab tests from there.
Once you have a diagnosis you can determine if your thyroid problem is something that is temporary or something that will require long-term treatment.
Remember:
You can almost always impact your disease state in some way by taking action to improve your diet, lifestyle, stress, and so on.
Now I want to hear from you:
Are you experiencing thyroid problems?
Have you been able to get a diagnosis and get treatment?
Why or why not?
Leave your comments below!
Scientific References
#1. https://www.ncbi.nlm.nih.gov/pubmed/21893493
#2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4044302/
#3. https://www.ncbi.nlm.nih.gov/pubmed/27038492
#4. http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2265.1977.tb02938.x/abstract
#5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3219552/
#6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3441105/
#7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3441105/
#8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1279933/
#9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4415174/
#10. https://www.ncbi.nlm.nih.gov/pubmed/3281846
#11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4415174/
#12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3271310/
#13. https://www.ncbi.nlm.nih.gov/pubmed/25758370
#14. https://www.ncbi.nlm.nih.gov/pubmed/2142391
#15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3063534/
#16. https://www.ncbi.nlm.nih.gov/pubmed/9571980
#17. https://www.ncbi.nlm.nih.gov/pubmed/3674063
#18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3169862/
#19. https://www.ncbi.nlm.nih.gov/pubmed/3132788
#20. https://www.ncbi.nlm.nih.gov/pubmed/20233310
#21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4980994/
#22. https://www.ncbi.nlm.nih.gov/pubmed/18844476
#23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3169863/
#24. https://www.ncbi.nlm.nih.gov/pubmed/18279014
#25. https://www.ncbi.nlm.nih.gov/pubmed/23777550
#26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4980994/
#27. https://www.ncbi.nlm.nih.gov/pubmed/23444388
#28. Cheron RG, Kaplan MM, Larsen PR. Physiological and pharmacological influences on thyroxine to 3,5,3’-triiodothyronine conversion and nuclear 3,5,3’-triiodothyronine binding in rat anterior pituitary. J Clin Invest 1979;64:1402-1414.
#29. Araujo RL, Andrade BM, da Silva ML, et al. Tissue-specific deiodinase regulation during food restriction and low replacement dose of leptin in rats. Am J Physiol Endocrinol Metab 2009;296:E1157-E1163.
#30. Leibel RL, Jirsch J. Diminished energy requirements in reduced-obese patients. Metabolism 1984;33(2):164-170.
#31. Croxson MS, Ibbertson HK. Low serum triiodothyronine (T3) and hypothyroidism. J clin Endocrinol Metab 1977;44:167-174.
#32.Dore C, Hesp R. Wilkins D, et al. Prediction of energy requirements of obese patients after massive weight loss. Human Nutr clin Nutr 1982;366:41-48.
#33. Drenick EJ, Dennin HF. Energy expenditure in fasting obese men. J Lab Clin Med 1973;81:421-430.
#34. Pittman CS, Suda AK, Chambers JB, McDaniel HG, Ray GY. Abnormalities of thyroid hormone turnover in patients with diabetes mellitus before and after insulin therapy. JCEM 1979;48(5):854-60.