Did you know that iron deficiency may be one of the reasons your thyroid symptoms remain out of control even while taking thyroid medication?
Iron deficiency is one of the most common nutrient deficiencies seen in hypothyroid patients.
It’s up there with B12 deficiency, magnesium deficiency, and vitamin D deficiency.
Not only is it common, but it is frequently misdiagnosed and/or missed by doctors.
Why? For one very important reason:
Most doctors are trained to look for iron deficiency anemia (1).
They rarely ever miss this diagnosis.
But what they do miss is suboptimal iron levels as measured by ferritin.
When it comes to thyroid function, the measure of your iron stores (and not your serum iron levels) is more important.
Patients who have hypothyroidism deserve special attention and treatment if their iron stores are low because of how important iron is for thyroid hormone function (2).
Today you will learn:
- Why iron is so important for thyroid function.
- How to test both your iron levels and iron storage levels.
- What level of iron is optimal for thyroid function.
- When to supplement with iron and which types of supplemental irons work best.
- How iron impacts thyroid medication absorption and other supplements.
- And much more…
Thyroid Function and Iron Status
Iron is required for proper thyroid function.
Studies are clear on the matter (3).
Not only is iron required for the creation of thyroid hormone (4), but low iron levels are also associated with low levels of free T3 (5).
As a thyroid patient, you are probably well aware that T3 is the single most important and powerful thyroid hormone in your body.
Iron deficiency reduces how much of that hormone your body can produce.
This may explain why some patients still experience the symptoms of hypothyroidism despite taking their thyroid hormone medication.
The association between iron and TSH level is clearly defined in the graph below:

You can see the inverse relationship between transferrin saturation and the TSH.
As your transferrin saturation falls (6), the TSH rises indicating a state of hypothyroidism.
Remember:
A high TSH means low thyroid and a low TSH means high thyroid.
Transferrin saturation is a lab test that tells you how much of the serum iron in your body is bound versus unbound.
A low transferrin saturation indicates low serum iron levels in the body.
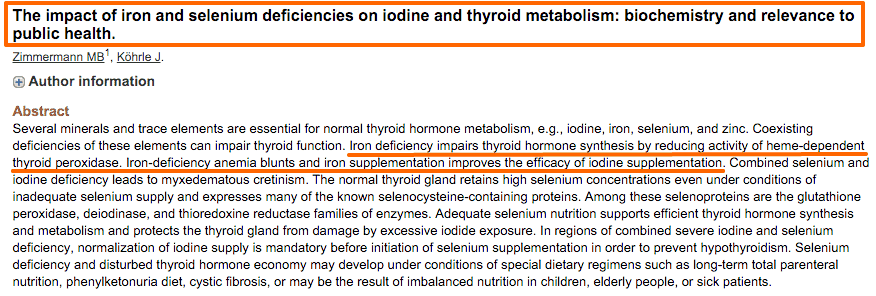
When it comes to thyroid hormone production, iron is required due to its effects on heme-dependent thyroid peroxidase.
Heme-dependent is another way to say iron-dependent. In other words, this important enzyme requires iron to function.
In addition, low iron has been shown to impact the effects of iodine supplementation (7).
Meaning the lower your iron levels are the less likely you are to utilize iodine if you are supplementing with it.
This can lead some patients to believe that iodine supplementation is not working for them when, in fact, it may be due to their iron status instead.
The worse part about iron deficiency is that it is so commonly missed.
Most providers will only check iron levels if they find that you have grossly abnormal hemoglobin or red blood cell levels which indicate iron deficiency anemia.
And because iron studies are not routinely checked, many hypothyroid patients are walking around with sub-optimal iron levels that are impairing their thyroid without even realizing it.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Symptoms of Low Iron & Hypothyroidism
So how do you know if you have iron deficiency?
One of the first places to look is at your symptoms.
If present, iron deficiency usually leads to a host of symptoms which we will go over in a second.
Unfortunately, because of the bidirectional relationship between iron deficiency and hypothyroidism, if you experience one you are likely to experience the other.
This complicates the picture because you may experience a combination of both hypothyroid symptoms and iron deficiency symptoms which do have some overlapping features.
As a result, you can’t always trust your symptoms but evaluating your symptoms can help you determine if you need further testing.

Symptoms of iron deficiency in hypothyroid patients include:
- Fatigue
- Weakness
- Pale Skin (especially in the creases of the palms)
- Shortness of Breath
- Dizziness, especially with exertion or exercise
- Cravings for ice (to eat or chew it)
- Cold hands and feet
- Brittle nails and thin/dry Hair
- Headaches
You will notice that many of these symptoms also closely match the symptoms of hypothyroidism.
For instance, both conditions can result in fatigue, weakness, and cold hands and feet.
How do you know if those symptoms are caused by your thyroid or by your iron status?
You won’t know for sure unless you get tested for both (more on that later).
Symptoms of Hypothyroidism
For comparison’s sake, let’s quickly discuss some of the symptoms of hypothyroidism.
You are probably well aware of these symptoms because you may be experiencing them right now but it’s still worth going over quickly.
Typical symptoms of hypothyroidism include:
- Fatigue especially after sleeping 8-10 hours a night or feeling like you need to nap daily
- Weight gain or the inability to lose weight
- Mood issues such as mood swings, anxiety, or depression
- Hormone imbalances such as PMS, irregular periods, infertility, and low sex drive
- Muscle pain and joint pain
- Cold hands and feet, feeling cold when others are not or have a persistently low body temperature
- Dry or cracked skin, brittle nails, and excessive hair loss
Patients with a combination of iron deficiency and hypothyroidism may notice that their hypothyroidism symptoms get worse the lower their iron gets.
The good news is that these symptoms do tend to decrease with proper iron supplementation and replacement.
Hashimoto’s Thyroiditis and Iron Deficiency
Do patients with Hashimoto’s also have issues with iron?
The answer to this question is a resounding yes.
While patients with Hashimoto’s thyroiditis are not your garden-variety hypothyroid patients, they still tend to have many of the same issues that hypothyroid patients experience.
The lack of thyroid hormone (or fluctuating thyroid hormone levels as the case may be) is still enough to cause changes to stomach acid (8) levels and alter iron absorption.

Proper iron levels are still required for optimal thyroid function in both hypothyroid and Hashimoto’s patients.
If you have Hashimoto’s make sure that you are also following the information outlined in this post so you can get properly evaluated.
Is your Iron Level Optimal?
When we talk about nutrient status we really need to differentiate between having ‘normal’ levels and having ‘optimal’ levels.
Most physicians are trained to look at reference ranges and base treatment on lab values that fall outside of the normal reference range.
But, unfortunately, the reference range for many nutrients (iron included) spans a wide range.
Take serum iron for instance:
The reference range is from 40-190 micrograms/dL.
Your doctor will most likely only care if you are less than 40 or higher than 190 mcg/dL.
But that leaves so much room in between where you may feel sub-optimal.
The difference between 50 and 150 is huge.
And your doctor may ignore your iron levels if your value is 45, but they may treat you if you are 38.
With this concept in mind, and when I give you my recommended reference ranges, I am always referring to the ‘optimal’ levels of iron in your body.
The optimal levels allow your thyroid to function optimally.
Because most physicians do NOT evaluate your labs with the optimal ranges in mind the chances are very high that you have suboptimal iron levels.
When it comes to evaluating for Iron deficiency I recommend these tests:
(Remember that you can ask your doctor to order these tests at your next visit, he/she shouldn’t have a problem doing this for you)
Iron Lab Tests: Ferritin, Serum Iron, % Saturation, and TIBC
To get your iron status evaluated you need ALL of the following lab tests:
Ferritin – This number represents the total storage of iron in your body.
Serum Iron – This represents circulating iron in your blood.
TIBC (Total Iron Binding Capacity) – This represents your body’s ability to carry iron (It will go up when the iron is low).
Percent Saturation – This is the ratio of serum iron and TIBC.
Your doctor will be used to ordering these labs, but the tricky part is in the interpretation.
I find that patients typically feel better when they fall within these ranges to both reduce symptoms and increase T4 to T3 conversion.
Instead of focusing on the standard reference ranges provided by the lab reporting your results focus on the following ranges.
Optimal iron levels for hypothyroid patients:
Ferritin – Optimal Levels = 40-50 ng/mL.
Serum Iron – Middle of the reference range.
TIBC (Total Iron Binding Capacity) – Middle of the Reference range.
Percent Saturation – 35-38%.
Falling outside of these optimal ranges may indicate that your iron is sub-optimal and may be impacting your thyroid function.
If this is the case then you will want to consider using treatments and/or supplements to bring your iron into the optimal range.
Hypothyroid Patients do Better on Liquid Iron
So what do you do if you find yourself with sub-optimal levels?
Based on my experience in testing hundreds of patients with low thyroid function, I’ve found that many thyroid patients frequently have ferritin levels in the 20-30 ng/mL range.
This usually puts them inside of the ‘normal’ reference range but outside of the ‘optimal’ reference range.
When the ferritin is this low it’s often a good idea to supplement with iron to bring the ferritin level back up.
When it comes to iron supplementation, you have a couple of options:
#1. iron tablets or capsules.
And #2. liquid iron.
Between these two options, liquid iron tends to work best for thyroid patients.
Liquid iron is more gentle on the stomach and often comes with additional nutrients that can assist in the absorption of iron.
Iron tablets and capsules can still work but may cause indigestion and worsen constipation.
As you know, thyroid patients already often suffer from constipation (9) so taking a supplement that may make that condition worse is not ideal.
If your iron level is low and you are looking for a liquid iron supplement then this one is a great option.
If you would prefer iron capsules then this would be a great option.
You don’t have to use my recommendations but if you choose to take iron of any kind just make sure to take it with Vitamin C to help increase absorption (10).
How to Take Iron Supplements
A word of caution for those thinking about taking an iron supplement:
You never want to take iron unless you know for sure that your level is low.
High levels of iron can be toxic to the body so make sure you check to see if you really need to supplement with iron before doing so.
If you’ve already checked your iron status and know that you need it then these guidelines should be considered:
Take your liquid iron away from food.
Avoid taking other supplements, coffee, or tea when you take your iron supplement (These may limit the absorption of iron).
Take your supplement with vitamin C or a glass of lemon water (both of these help your body absorb iron).
Take your iron with B vitamins – B Vitamins help with the absorption of iron.
Take your iron at least 4 hours away from your thyroid hormone medication (if you are taking any). Iron supplements can bind to thyroid hormone medication and prevent its absorption. If you are taking both then using one in the morning and the other at night works best.
Take your iron at least once per day.
The daily dosing of iron usually works best for those with sub-optimal ferritin but not very low ferritin levels (outside of the normal reference range).
If you find that your ferritin or iron are both below even the normal range then you may need to take your iron supplement several times per day.
Track your Progress by Following Ferritin Levels
When taking iron it is very important that you constantly monitor and track your progress every few weeks to months.
Not tracking may lead to really high levels of iron over time, or you may miss the fact that your body doesn’t tolerate the form of iron you are using.
Iron levels are easy to track.
After 4-6 weeks of taking an iron supplement, you can ask your doctor to recheck your iron panel (list above).
Once you have your results you can determine if the type of iron you are taking is working, if you need to cut back on your dose, or if you need to increase your dose.
Over time you should see your iron studies including serum iron and ferritin increase.
You should also experience a decline in your low iron symptoms and you may even see a decline in your hypothyroid symptoms.
Remember that iron is like Goldilock’s nutrient.
Too little is harmful to the body, but too much can be just as harmful.
You do not want elevated iron stores in your body as this can lead to inflammation and many other conditions (11).
What if your ferritin levels are elevated but you have low serum iron?
This lab pattern can and does happen, especially in patients with Hashimoto’s.
While ferritin is considered a marker of iron storage in the body it is also considered an acute phase reactant (12).
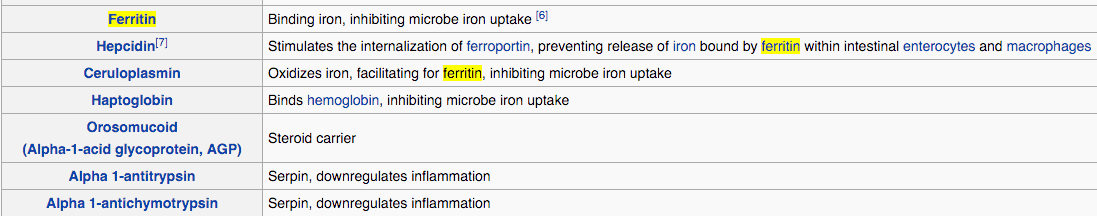
Acute phase reactants are measurements that can be tested in the body that elevate in states of inflammation.
And ferritin is one of these reactants.
This lab pattern of low serum iron with elevated ferritin is common in patients with Hashimoto’s thyroiditis and other inflammatory conditions.
Because Hashimoto’s is primarily a disease of the immune system, it makes sense that many patients with this condition also experience elevated inflammation.
The problem?
This pattern of high ferritin and low serum iron can fool you into thinking that your iron stores are high when in reality they are low.
The body is just in a state of inflammation which is masking the low iron storage.
For this reason, ferritin is a sensitive marker of iron storage when it is low but not when it is high.
If you have this lab pattern then you can often tease out what is really happening by ordering additional tests to check for inflammation.
This will help you determine if you actually need to supplement with iron.
Recap & Final Thoughts
Patients with hypothyroidism and Hashimoto’s frequently experience sub-optimal iron levels.
Iron is critical to thyroid function in the body and these sub-optimal levels can lead to symptoms that may mimic the symptoms of hypothyroidism.
Because of these changes, it is important that you have your iron levels evaluated with optimal ranges in mind.
If you are suffering from hypothyroidism and think you may also have sub-optimal iron levels then you should start by getting a full iron lab test panel.
Replacing low iron may help improve thyroid function by increasing T4 to T3 conversion and helping your thyroid medication do its job.
And while you are at getting your iron levels checked don’t forget to check for other nutrient deficiencies such as vitamin B12, vitamin D, and magnesium.
These are also very common nutrient deficiencies found in hypothyroid patients.
FAQ about Iron and Hypothyroidism
Can an iron deficiency cause hair loss?
Yes, iron is required for proper hair growth and may be one of the main causes of hair loss in patients with hypothyroidism and Hashimoto’s thyroiditis.
Unfortunately, low thyroid hormone itself can also cause hair loss or changes to your hair which can make identifying the true cause of hair loss difficult.
Many patients with hypothyroidism who also have hair issues (hair loss, damaged hair, etc.) have a combination of both iron deficiency and low thyroid hormone.
Replacing iron levels and replacing thyroid hormone in the body are both required for optimal hair growth.
You can read more about how to address hair loss and regrow your hair if you have hypothyroidism in this article.
Will iron deficiency make weight loss more difficult?
The answer is maybe.
Why?
This largely has to do with the interaction between iron and thyroid hormone.
When iron is low your thyroid function will also be blunted.
Low iron decreases thyroid function which may lead to a decreased metabolism which may lead to weight gain.
You can draw a line between iron deficiency and weight gain but it’s not as clean as you might think.
If weight loss is your goal you will want to take a multifaceted approach that addresses nutrient deficiencies, hormone imbalance, thyroid function, inflammation, diet, stress reduction, sleep, and so on.
So while iron is technically included in this list it’s not the most important part.
What is ferritin?
Ferritin is a marker of iron stored in the body.
It is also a marker of inflammation and is often elevated in inflammatory states.
At low levels, it is very sensitive to iron deficiency, but at higher levels, the value becomes less predictive of iron status and more predictive of inflammatory states.
Is ferritin required for hair growth?
Yes, a ferritin level of at least 30 ng/mL is required for optimal hair growth (13).
Studies have shown that levels less than 30 ng/mL may result in hair loss.
Low ferritin, along with low thyroid function, is probably the most important factor for hair growth in thyroid patients.
How long will it take for my iron/ferritin to increase?
As long as you are absorbing the iron supplements that you are taking then you should see an improvement in both measures within 2-3 months.
Ideally, you will want to retest your ferritin and iron studies after 8 weeks of daily iron use.
You may not see a large bump in either at that time, but you should see a slow and steady upward trend (even if minor).
If you do not see any positive change then you may need to evaluate the type of iron you are taking.
For instance:
Are you taking pills or are you taking liquid? What type of iron are you taking? How much are you taking? Is your intestinal tract allowing for absorption?
Answering these questions may help you make changes to your regimen.
What if iron supplements don’t work?
For various reasons, you may be someone that doesn’t respond to oral iron supplements.
If you fall into this category then you may need what is called an iron infusion.
This is a small procedure in which iron is directly infused into your bloodstream.
It is very effective at increasing iron stores in your body but it is typically only used for extreme cases.
This procedure is usually reserved for those suffering from acute iron deficiency, those who are having trouble with constant bleeding, or those who have repeatedly failed oral iron supplements.
This procedure does carry some risks (14) with it so it is typically performed in a hospital-like setting.
If you find that you are not responding to iron supplements, or if you fit any of the categories listed above, you may want to speak to your doctor about an iron infusion.
Can an iron deficiency cause anxiety?
Iron deficiency may exacerbate symptoms of anxiety and may indirectly lead to panic attacks.
Low iron leads to increased shortness of breath which may make certain patients feel like they are unable to catch their breath.
This can trigger a cascade of events leading to a panic attack or anxiety.
Now I want to hear from you:
Have you been suffering from iron deficiency as well as hypothyroidism?
What have you done to increase your ferritin levels?
What didn’t work for you?
Leave your comments below!
Scientific References
#1. https://www.ncbi.nlm.nih.gov/books/NBK448065/
#2. https://pubmed.ncbi.nlm.nih.gov/28202844/
#3. https://www.ncbi.nlm.nih.gov/pubmed/12487769
#4. https://www.ncbi.nlm.nih.gov/pubmed/12487769
#5. https://www.ncbi.nlm.nih.gov/pubmed/16500878
#6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4729155/
#7. https://www.ncbi.nlm.nih.gov/pubmed/12487769
#8. https://pubmed.ncbi.nlm.nih.gov/12754530/
#9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6185413/
#10. https://www.ncbi.nlm.nih.gov/pubmed/2507689
#11. http://www.irondisorders.org/iron-overload
#12. https://www.ncbi.nlm.nih.gov/books/NBK519570/
#13. https://www.ncbi.nlm.nih.gov/pubmed/23428658
#14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4518169/