Cancer is a scary word and most of the fear associated with this word has to do with not understanding cancer.
If you can learn the basics of thyroid cancer, including what to expect with treatment and prognosis, then you may not be as fearful about your cancer.
This guide will teach you what you need to know about thyroid cancer (if you or a loved one has been diagnosed) including the symptoms associated with this disease, how it is diagnosed and treated, what the survival rate is, and more:
Thyroid Cancer 101
Let’s start with some basics…
Thyroid cancer is a fairly common type of thyroid cancer and is the most common type of cancer of your endocrine or hormone system.
The good news about thyroid cancer is that it is a good cancer to have (if you have to have one) because the most common type of thyroid cancer is the least aggressive and most treatable.
In addition, the survival rate among thyroid cancer patients is as high as 97% (1).
Much of this has to do with the fact that thyroid nodules are so aggressively monitored (with ultrasound imaging) (2) and because people tend to find thyroid cancer early.
Once cancer gets to the late stage and it goes throughout the body, it can be very difficult to treat.
Luckily, this doesn’t happen in most cases of thyroid cancer (except for very rare forms).
To try and dispel the fear associated with thyroid cancer I’ve put together a checklist of events that tend to happen with most thyroid cancer patients.
This outline isn’t perfect, but it can really help you understand the big picture and help to ease your mind.
The typical course of how thyroid cancer is identified and treated (not all patients will necessarily fit this mold):
- Patients are told they have a thyroid nodule which requires further workup with imaging studies. Most nodules are not symptomatic and are often found during routine exams or accidentally with other imaging studies of the chest/heart/lungs. It’s important to realize that the vast majority of thyroid nodules are NOT cancerous, in fact up to 99% of all thyroid nodules are considered benign and do not contain cancer cells (4).
- This nodule is imaged using ultrasound technology where your radiologist can determine if the nodule has a certain key feature that increases the risk of thyroid cancer (features such as size, calcium deposits, and so on). The radiologist may also evaluate the lymph nodes in your neck to see if they look suspicious.
- If the nodule is suspicious then a fine needle aspiration is recommended (known as FNA for short). This biopsy procedure allows Pathologists (a certain type of Doctor) to examine a sample of the nodule under a microscope to learn more about the nodule. This information usually allows the pathologist to determine what type of thyroid cancer you have and how advanced the cancer is (5). This information is critical and helps outline which treatments are necessary. If you have an enlarged lymph node in the neck then this also may need a biopsy to determine if the cancer has spread.
- If thyroid cancer is identified then the next step is complete (or partial) removal of the thyroid gland from the neck. This procedure is known as “thyroidectomy”. Depending on how advanced the cancer is you may also need to have some, or all, of your lymph nodes removed as well.
- In some cases, the removal of your thyroid gland will be the only treatment that you need (6). But some patients will benefit from an additional therapy known as Radioactive Iodine ablation. This procedure kills off any remaining thyroid gland cells in your body (even thyroid cells with cancer). Your Doctor will help you determine if you need RAI in addition to thyroid removal.
- After your thyroid is removed you will be started on thyroid hormone replacement medication. This medication is REQUIRED and all patients who have their thyroid removed must use thyroid medication for the rest of their life. Thyroid hormone is required for optimal function of your body and so it must be replaced after your thyroid is removed or damaged with RAI.
- After your procedure, you will need to have your blood tested every few months to determine if your dose of thyroid hormone is adequate (7). Insufficient thyroid hormone replacement may result in fatigue, weight gain, depression, hair loss, and so on.
This sequence of events is fairly typical of patients who are diagnosed with thyroid cancer.
But remember:
Not all patients will have the same presentation and will require the exact same treatment!
There are many different types of thyroid cancer (some more aggressive than others) and all of these factors determine how your cancer needs to be treated.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
What are the Symptoms of Thyroid Cancer?
Most patients with thyroid cancer do NOT have any symptoms meaning they are asymptomatic.
One point that is confusing for many patients is that thyroid cancer usually doesn’t cause problems with the thyroid gland itself.
Conditions of the thyroid gland itself, known as hyperthyroidism and hypothyroidism, tend to occur from OTHER conditions such as autoimmune disease or nutrient deficiencies.
It’s important to understand this because some conditions, such as thyroiditis or goiter, can interfere with thyroid hormone production and increase the overall size of your thyroid gland.
This may cause a “thyroid cancer scare” even though it is from a completely different condition.
But does this mean that it can’t cause symptoms?
No, but it does mean that it is rare.
If thyroid cancer causes symptoms it tends to be because the cancer is sufficiently large enough that it is compressing important anatomical structures in the neck.
For instance:
If thyroid cancer is large enough it may cause problems with breathing, changes in your voice, or pain with swallowing.
This has to do with where your thyroid gland is placed (right in the middle of your neck) and the proximity of your thyroid gland to very important anatomical structures.
As you can imagine, if something is large enough to interfere with your voice box then it will usually be visible when swallowing or when closely examining the neck.
Most cases of thyroid cancer are NOT this big and they are only detected with careful palpation (touching) of the thyroid gland or with special high-resolution ultrasound imaging (9).

Some thyroid cancers, such as medullary thyroid cancer, tend to infiltrate lymph nodes which may cause enlargement of lymph nodes in your neck.
For medullary thyroid cancer, this is common, but for papillary and follicular thyroid cancer this is less common.
Symptoms of thyroid cancer include:
- Difficulty or pain with swallowing
- Changes to your voice
- Pain in the neck or in the thyroid gland
- Enlargement of lymph nodes in your neck
- A constant cough (which doesn’t produce any sputum)
Note: Thyroid cancer is usually painless, so if you have an enlarged and painful thyroid gland then it is more likely to be related to thyroiditis than thyroid cancer.
But how do we catch thyroid cancer early if patients don’t have any symptoms?
Most of the diagnosis of thyroid cancer comes from the proper evaluation of thyroid nodules (more on that below).
How is Thyroid Cancer Diagnosed?
Thyroid cancer is often suspected based on ultrasound imaging and confirmed with fine needle aspiration or biopsy.
If there is any suspicion whatsoever regarding the shape or size of your thyroid gland then your Doctor will order an ultrasound image.
If you have any inflammation in the gland, thyroid nodules, irregularities in thyroid texture, etc. all of these may be visible on the ultrasound.
In fact, certain characteristics are typical of thyroid cancer and these characteristics can help guide diagnosis and further management (11).
If, for instance, you have a thyroid nodule that has calcifications inside of it with ill-defined margins and locally enlarged lymph nodes, then the risk that your thyroid nodules are cancerous is increased.
Below you can find features seen on ultrasound that can tip off your doctor (and you) to early types of thyroid cancer based on these characteristics.
These characteristics can be thought of as specific patterns seen in certain thyroid cancers which radiologists give specific names.
You can find this information on the “impression” portion of your ultrasound report.
Features on ultrasound that may indicate you have papillary thyroid cancer include (you can find more information here (12)):
- Predominately solid (70%) and hypoechoic (77-90%)
- Presence of punctate microcalcification
- Ill-defined margins
- Intranodular vascularity on color flow imaging
- Cystic necrosis and microcalcifications in local lymph nodes
Features on ultrasound that may indicate you have anaplastic carcinoma include:
- Hypoechoic tumor involving the entire lobe or thyroid gland
- Ill-defined margin
- Areas of necrosis or cell death in the gland (78%)
- Necrosis or death of local lymph nodes
- Intranodular vessels on color flow imaging
- Expansion of cancer outside of thyroid capsule
Features on ultrasound that may indicate you have medullary carcinoma:
- Solid hypoechoic nodule (one specific spot)
- Echogenic foci in the tumor
- Chaotic intranodular vessels on color flow imaging
Features on ultrasound that may indicate you have follicular thyroid cancer include:
- Hyperechoic area/lesion
- Predominately solid
- Well-defined and “haloed” on imaging
After ultrasound imaging, if necessary, your Doctor will order an FNA biopsy which will give more results and tell you exactly the type of cancer that you are dealing with (13).
From there you will have a better idea as to what you are dealing with and how to treat it (depending on the type and stage of cancer).
Thyroid Cancer Prognosis and Survival Rates
When it comes to thyroid cancer it’s helpful to understand some basic rules:
#1. The earlier you catch and treat thyroid cancer the better.
#2. The earlier the stage (meaning stage 1 and stage 2) the better your prognosis will be.
#3. Certain types of cancers carry a better prognosis than others (due to how aggressive they can be).
#4. Your age at the time of diagnosis matters. Those who are less than 35 years old tend to have a better prognosis than those who are older than 62 at the time of diagnosis (14).
#5. Each individual case is different.
So with these in mind let’s talk about thyroid cancer and survival rates.
Fortunately, the most common type of thyroid cancer (known as papillary and follicular thyroid cancer) is the most treatable and curable type of thyroid cancer you can have.
Up to 85% of all cases of thyroid cancers fit into this criteria (15).
In many cases, complete removal of the thyroid gland (with or without RAI therapy) is sufficient to “cure” cancer.
The 5-year survival rate for patients who have this type of cancer is as high as 98% (and as low as 85% depending on the study).
This means that if 100 people have papillary/follicular thyroid cancer that 98 of them will be alive after 5 years (which is considered a very high survival rate for cancer).
The survival rate isn’t perfect, however, because some people continue to have cancer despite having their thyroid removed.
Unfortunately, it is impossible to completely remove the thyroid gland, even with surgery, so there is a small possibility that you may retain some thyroid cancer cells even after your surgery.
In some cases, cancer can come back locally (where your thyroid was removed) and this is known as “local recurrence”.
The most aggressive type of thyroid cancer is known as anaplastic thyroid cancer.
Anaplastic thyroid cancer rapidly grows and is often found outside of the thyroid gland upon diagnosis.
In general, the faster cancer grows and the more it spreads throughout the body the worse the prognosis.
Because of this anaplastic thyroid cancer has the worst prognosis out of all thyroid cancers.
Most patients with anaplastic thyroid cancer do not survive longer than 6-8 months after diagnosis (17).
Fortunately, this type of cancer is also the rarest.
Types of Thyroid Cancer
You can think of cancer as something that grows without the normal growth restrictions put upon your cells.
These restrictions help keep your cells in check and prevent overgrowth.
Cancer emerges from specific types of cells and your organs/tissues vary in which types of cells are in them.
Cancers are named based on what types of cells they emerge from and often the type of cell they emerge from can tell you something about how they behave.
The different types of cells in your thyroid gland include:
#1. Follicular cells that pump out your thyroid hormones.
#2. Parafollicular cells that pump out calcitonin (medullary thyroid cancer emerges from these cells).
Another important thing to know about your cancer is whether or not it is “differentiated”.
Differentiated refers to the appearance of your cells under the microscope when they are evaluated by a pathologist.
Cancers that are “differentiated” can easily be identified while cancers that are “undifferentiated” cannot.
From a prognosis standpoint, it’s better to be able to differentiate the cells which means that undifferentiated cancers (like anaplastic thyroid cancer) tend to be more aggressive than differentiated cancers.
Differentiated cancers tend to include papillary, follicular, and Hurthle cell cancers while undifferentiated cancers include the anaplastic thyroid cancer variant.
You can find a list of thyroid cancers below including some basic information:
- Papillary thyroid cancer (18) – Accounts for the majority of thyroid cancers (around 80+%). This type of cancer is the most common but also carries the best prognosis.
- Follicular thyroid cancer (19) – Accounts for 10-20% of thyroid cancers.
- Medullary thyroid cancer (20) – Accounts for 3-4% of all thyroid cancers. Up to 20% may be hereditary (meaning they run in the family). This type of cancer can either be aggressive or slow growing.
- Anaplastic thyroid cancer (21) – Accounts for about 2% of all thyroid cancers. Anaplastic thyroid cancer is very aggressive and grows very quickly which leads to a much poorer prognosis compared to other types of thyroid cancer. Because this cancer behaves differently from the other types of thyroid cancers listed here this type of thyroid cancer may require surgical removal, removal of lymph nodes, chemotherapy, and/or radiation therapy.
Treatment Options
The goal when treating thyroid cancer is to attempt to remove cancer from the body while minimizing damage to other necessary organs and tissues.
The cancerous cells of your thyroid gland can be removed through surgery, but they can also be damaged and killed through other methods such as radioactive iodine ablation.
Depending on the type of thyroid cancer that you have, how aggressive the cancer is, and if it has spread, your doctor may use a combination of the therapies listed below:
- Surgery – The most common surgical procedure used to treat thyroid cancer is a complete thyroidectomy (which is the complete removal of your thyroid gland). Sometimes surgical removal of lymph nodes may also be necessary.
- Radioactive Iodine Ablation – Radioactive iodine is a special procedure that uses iodine molecules that have been targeted with radiation. This therapy takes advantage of the fact that your thyroid concentrates iodine inside of it while other cells do not. This means that if you give someone radioactive iodine, their thyroid cells (including cancerous cells) will take up this molecule and damage/kill the cells inside. Radioactive iodine is a useful procedure to help kill off thyroid cells even after your thyroid has been removed (because it’s impossible to surgically remove ALL thyroid cells even with complete thyroid removal).
- Chemotherapy and Radiation (22) – Rarely used but may be necessary for very aggressive cancers such as anaplastic thyroid cancer.
- Suppressive thyroid hormone replacement therapy – After your procedure, your Doctor may intentionally give you a high dose of thyroid hormone medication with the goal to suppress a hormone known as TSH. TSH is secreted by the pituitary gland and is short for Thyroid Stimulating Hormone. As the name implies, TSH stimulates your thyroid gland and thyroid tissues which may cause the growth of existing thyroid cancer. By eliminating or “suppressing” your TSH it is felt that this therapy may reduce the risk of thyroid cancer recurrence and slow down thyroid cancer growth.
Conclusion
Thyroid cancer is the most common type of endocrine cancer in the body.
Despite it being the most common endocrine tumor, it is still not very common.
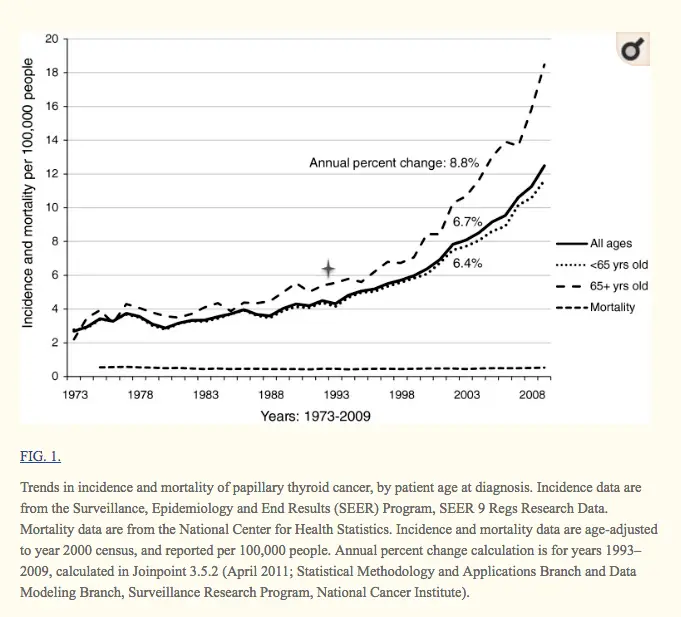
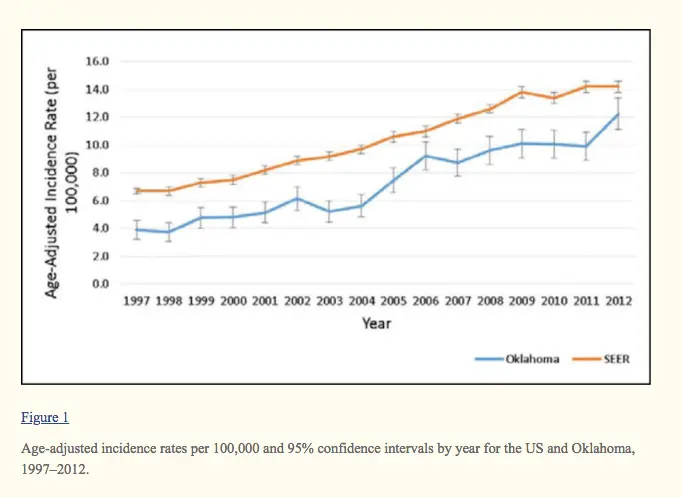
The rate and incidence of thyroid cancer are increasing which is felt to be secondary to increased and early detection.
While the rate and incidence of thyroid cancer are increasing, the mortality and prognosis associated with the disease are staying stable (which is a good thing!).
The most common type of thyroid cancer, differentiated thyroid cancer, is very treatable and carries an excellent prognosis (one of the highest among all types of cancers).
Rarely, thyroid cancer can be undifferentiated which means it may be aggressive and grow very rapidly.
Now I want to hear from you:
Do you have thyroid cancer?
Which type of thyroid cancer do you have? Is it differentiated or undifferentiated?
What treatment have you undergone?
How are you doing now?
Leave your comments below!