Would it surprise you to know that, contrary to what your doctor might tell you, you can do something about your elevated antibodies?
And we aren’t talking about fly-by-night radical treatments that are insanely expensive or may cause you to grow a third arm.
I’m talking about research-backed treatments that have been used successfully by tens of thousands of Hashimoto’s patients in the past.
That’s all well and good, but why does it matter? Doesn’t good old levothyroxine do everything that you need?
No way!
While levothyroxine can *sometimes help you feel better, it does nothing to stop the ultimate progression of Hashimoto’s which is the destruction of your thyroid gland.
And the sooner you do something about your immune system the better because you can *sometimes put your disease into remission.
The earlier you start these treatments the better, but even if you’ve had a rip-roaring case of Hashimoto’s for decades, something is still better than nothing which is probably what your doctor is recommending.
So with this in mind, let’s talk about some treatments that can help you reduce your thyroid antibodies starting right now:
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
#1. Diet (The Foods you Put In Your Mouth)

The first, and perhaps most important step, is to take a long look at the foods that you are putting into your body.
And by that, I am referring to your diet.
Not the type of diet that you get on for a few weeks or days, but a lifestyle shift that helps you continuously and consistently put healthy food inside of your body.
Maybe you are already eating ‘healthy’ foods and you think this section doesn’t apply to you.
This type of logic may not necessarily be true, especially considering that there are many types of ‘healthy’ diets, and not all of them are healthy or ideal for those with Hashimoto’s.
In fact, there is a wide dispute over what constitutes a healthy diet (4)!
To further complicate the picture, each person is unique in terms of what type of foods they tolerate and what type of foods cause inflammation or harm.
And these foods can shift throughout a person’s life as well!
The good news is that we don’t have to look far to figure out what works for Hashimoto’s.
We have a bunch of information from patients with Hashimoto’s to be our guide.
In fact, we have hundreds of case studies, and even medical research, to suggest which diets are best.
Based on this information, here are the top 3 best diets for those with Hashimoto’s looking to reduce their TPO antibodies:
Going Gluten-Free, Dairy-Free, and Soy-Free Diet
Perhaps one of the best shotgun approaches to changing your diet is by going gluten-free, dairy-free, and soy-free.
If you aren’t sure where to start then you may want to start here.
While not everyone with Hashimoto’s will need to stay off of these food groups long-term, it’s still one of the easiest and most effective diets for treating Hashimoto’s.
I don’t believe that everyone with Hashimoto’s HAS to be gluten-free forever, but I do find that foods containing gluten can exacerbate and perpetuate inflammation in the gut, and temporarily removing them for a short period, usually helps most people.
Soy, due to its processing, may lead to inflammation and dairy has been shown to be inflammatory for various reasons as well.
Using the Autoimmune Paleo Diet or AIP Diet
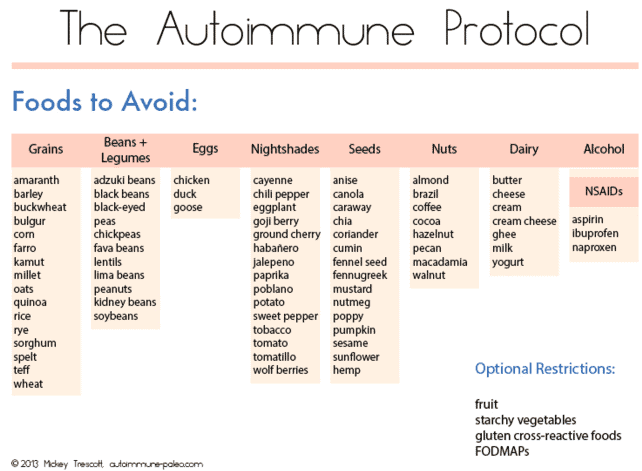
The AIP diet stands for autoimmune protocol or the autoimmune paleo diet.
You can think of this type of diet as a pared-down version of the paleo diet.
It takes the standard paleo diet, which is already fairly restrictive, and restricts your food choices even further.
And it turns out that the AIP diet is actually quite effective at lowering TPO antibodies for most people who use it.
You can see a case study of a patient with Hashimoto’s who used the AIP diet, in conjunction with other therapies, to lose 50 pounds and improve her thyroid status significantly.
This is just one example but there are many others.
There are also emerging studies (5) that show promise in using the AIP diet to treat all sorts of autoimmune conditions.
One of the downsides to using this diet is that some people end up restricting their diet so much that they develop an intolerance to healthy foods and have trouble re-introducing them back into their diet.

Because of this, I tend to reserve the AIP diet for those who have failed less restrictive diets or for those who have a history of multiple autoimmune diseases on top of their diagnosis of Hashimoto’s.
One of the benefits of going on the AIP diet is the amazing online community, free recipes, and help that you can receive through online groups.
Using the Elimination Diet
The elimination diet can be very powerful at reducing TPO antibodies as well.
In a nutshell, the elimination diet works by removing certain food groups that may be perpetuating inflammation in your body.
As you remove these foods, and if they are causing you issues, you should notice an improvement in your digestion and your symptoms fairly quickly.
You can do this diet one of two ways:
#1. Test yourself using delayed IgG food sensitivity testing and remove only food groups that you react to based on this test.
Food intolerance testing, while potentially helpful, is certainly not 100% reliable or accurate (6).
Often, people will find that they are ‘reactive’ to MANY different types of foods and food groups even those that are considered quite healthy.
Because of this, testing for food intolerance may lead you astray and cause you to remove food groups that would otherwise be beneficial.
There are some people, including those that I’ve treated in the past, who have done very well by following the information provided by these tests, however.
#2. Remove the most common food allergies and monitor your symptoms upon reintroduction of those food groups.
If you don’t want to test for food sensitives you can always take the shotgun approach by simply removing specific food groups that are widely known to cause issues (7).
Foods in this group include:
- Eggs
- Wheat
- Dairy
- Soy
- Peanuts
- Shellfish
- Tree nuts
- Beef products
- Corn
Statistically speaking, these food groups are usually the cause of digestive problems for most people.
Removing all of these food groups for a period of time (usually 6 to 12 weeks) and then reintroducing them slowly one at a time will help you determine which ones are causing you issues.
From there, it’s just a matter of trial and error until you figure out what works best for your thyroid and antibody levels.
#2. Increasing your Testosterone Levels
Androgens such as DHEA and testosterone are another powerful tool that can be used to help lower TPO antibodies and most people don’t even know they exist as a potential treatment!
In case you haven’t noticed, the majority of patients who have Hashimoto’s are women (8).
This is actually true of almost ALL autoimmune diseases (with few exceptions).
Part of the reason this is felt to occur has to do with how testosterone, DHEA, and other androgens interact with your immune system (9).
It is currently felt that higher (or should I say ‘normal’) levels of testosterone act as a sort of protection against autoimmune diseases.
Because men have higher baseline levels of testosterone they are more protected than women (assuming this theory is correct).
If this theory is correct then it follows that people with low testosterone may be at increased risk for developing Hashimoto’s thyroiditis.
And this certainly holds true in my experience, as I often test each and every patient with Hashimoto’s for both testosterone and DHEA.
My experience suggests that most women with Hashimoto’s also tend to have lower-than-normal testosterone levels for their age.
If you are someone who has both Hashimoto’s and low testosterone, then you may benefit from the use of testosterone cream or gel.
Testosterone is a bio-identical hormone that can be used as a medication to help bring up total testosterone levels in the body.
Women tend to benefit tremendously from testosterone, just like men, even at low doses.
The goal when using testosterone cream or gel in women is to bring your testosterone back up to a normal level, not to give you more than you need.
Using testosterone in this way makes it a very safe and effective treatment for both men and women.
Testosterone replacement therapy (TRT for short) may help your immune system in the following ways:
- Balance TH1 and TH2 (10) immune responses
- Lower the autoimmune process and autoimmune attack on the thyroid gland (and, in some cases, suppress it) (11)
- Enhance weight loss (a great benefit for many patients with Hashimoto’s thyroiditis)
- Increase libido and sex drive (12)
How do you know if you are a potential candidate for using testosterone therapy to treat Hashimoto’s?
It’s simple, you just need to order a few tests including serum free testosterone, total testosterone, and DHEA-S.
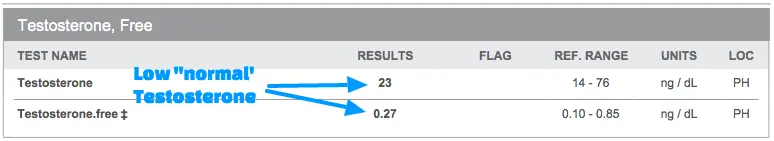
Once you have your tests in hand, all you need to do is look at your result and compare it to the reference range.
I find that women with testosterone (free or total) in the bottom 1/3 of the reference range often benefit from taking testosterone.
As you take testosterone, make sure you monitor both your symptoms and your total and free testosterone levels.
You can get testosterone through gels, creams, pellets, or injections.
If you are unable to get your doctor to prescribe testosterone then you may want to look into using DHEA.
DHEA is a weaker androgen when compared to testosterone but it is available over the counter as a supplement.
Your body uses DHEA as a template for creating testosterone and estrogens.
Use caution when taking DHEA, though, as you can’t control what your body decides to do with it once you take it.
Your body may take that DHEA and produce estrogen in place of testosterone which may cause more harm than good!
#3. Optimizing your Vitamin D Level

Vitamins and certain supplements can also be used to help balance immune function and may, therefore, reduce your thyroid antibody levels.
It’s always a good idea to keep an eye on all nutrients in your body for overall health but there are several that play a more focused role in regulating your thyroid and immune system.
The only downside to using supplements to try and lower thyroid antibodies is that we don’t have a lot of evidence to suggest that they work for every person.
Having said that, anecdotally, I’ve seen a lot of success in patients who use supplements when managing Hashimoto’s.
When you use a supplement, just be aware that what worked for someone else may not work for you.
Keeping that in mind will help manage your expectations.
When it comes to vitamins and Hashimoto’s, few are more important than Vitamin D.
Vitamin D is involved in regulating immune function (13) and is commonly deficient in patients who have Hashimoto’s thyroiditis.
Replacing Vitamin D may be one easy way to ensure that your immune system is functioning well.
Vitamin D, as long as you use the right form, is also very cheap!
Before you use Vitamin D, though, make sure you test your levels.
You can do that by ordering a 25-hydroxy Vitamin D level (14).
If your 25-hydroxy Vitamin D is less than 40 ng/mL or higher than 60 ng/mL then you want to try and adjust it back into that range.
While Vitamin D deficiency is quite common among the general population, there is a growing number of people who are actually taking too much (especially within the thyroid population).
So be sure you are within that range.
When taking a Vitamin D supplement make sure your Vitamin D is in the D3 form.
Vitamin D2, commonly prescribed by doctors, requires processing by the body and is not the ideal form to use.
For better absorption, look for a micellized D3 supplement in a liquid.
#4. Improving Gut Health
I mentioned earlier that many patients with Hashimoto’s also suffer from gut-related issues.
I want to take a second to expand on that here.
Your gut is the center of thyroid hormone conversion, neurotransmitter production, and immune system education.
Any problem in your gut may, therefore, affect and alter any of these systems.
Dysfunctional gut health may lead to more inflammation in the body and may actually be the site where Hashimoto’s originates.
For this reason, if you want to lower your TPO antibodies then you must pay attention to your gut!
That means treating all gut-related issues, balancing gut bacteria, and killing off potentially harmful gut bacteria.
Patients with Hashimoto’s can experience a range of gut-related issues including any or all of the following:
- Acid reflux
- Low stomach acid (15)
- Autoimmune gastritis (16)
- Intestinal atrophy from Celiac Disease (17)
- H. Pylori infections (18)
- Small intestinal bacterial overgrowth (19)
- Gastroparesis (20)
- Small fungal bacterial overgrowth
- Intestinal dysbiosis
The presence of any of these gut conditions can negatively impact your immune system and may make your Hashimoto’s worse.
The solution?
You have to identify any gut problems you may suffer from and treat those problems!
This is easier said than done, I know, but it’s often one of the most important things you can do if you have Hashimoto’s.
For many, making simple changes such as taking a probiotic and a prebiotic and eating healthy foods can be enough to see serious changes in your gut (for the better).
If you don’t see success with this approach then you may need further testing by your doctor to evaluate for infections or other problems such as Celiac disease.
#5. Consider using LDN (Low Dose Naltrexone)
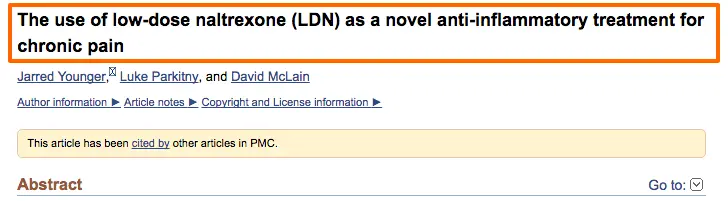
In this case, I saved the best for last.
I’ve personally found low-dose naltrexone (or LDN for short) to be particularly helpful in lowering TPO antibodies, reducing inflammation in Hashimoto’s, and treating other problems thyroid patients face such as weight gain and chronic pain.
But what is LDN?
LDN is an opiate blocker (meaning it sits on the receptor and blocks opiates from binding to your cells) and is available as a prescription medication.
It is conventionally used to treat alcohol addiction, but it can be used off-label to help modulate the immune system to treat autoimmune diseases.
The mechanism of action is not well understood but it probably works by temporarily increasing endorphin production.
Taking low doses of LDN causes a blockade of opiate receptors which then fades rapidly and results in a corresponding increase in endorphins which then impact the immune system.
LDN has gained traction in the integrative and functional medicine community as a potential treatment for autoimmune diseases including Hashimoto’s thyroiditis.
While it doesn’t have as many studies as other standard medications, it has been shown to be beneficial in the following ways:
- Modulate the immune system
- Help the body differentiate between self and foreign tissue
- Lower inflammation (21)
- Reduce chronic pain (22)
How do you use LDN to lower TPO antibodies?
Because LDN is used off-label, the standard dosing recommendations don’t really apply.
Instead of using the standard dose of 50mg, LDN takes advantage of a much lower dose usually in the range of 1.5mg to 4.5mg per day.
Dosing usually starts on the low end and slowly titrates up over a period of time.
After a set period of time of daily use, you can check your thyroid antibodies to see if you experience any benefit.
Unfortunately, LDN will not work for everyone.
My experience, as well as that of many others who use it frequently, suggests that around 50% of people who use it experience some benefit.
The other 50% notice no real perceptible change or improvement.
How do you know if it’s working?
The best way to know is to simply keep track of your symptoms and keep track of your TPO antibodies.
If it’s working then you will notice a reduction in your low thyroid symptoms and a reduction in your TPO antibodies.
If you’ve taken LDN for 3 months or longer and you haven’t noticed a change in either then you are probably in the 50% group that won’t benefit from using it.
#6. Black Seed Oil (Nigella Sativa)

Another great option to get your antibodies under control is the use of a plant called nigella sativa.
This topic can get kind of confusing but let me break it down for you:
Nigella sativa is the plant that produces black seeds which are commonly pressed to create black seed oil.
And, we have at least one double-blind placebo-controlled trial showing that nigella Sativa powder (23) (from the plant) can help reduce thyroid antibodies, boost thyroid function more generally, and shrink the size of the thyroid gland.
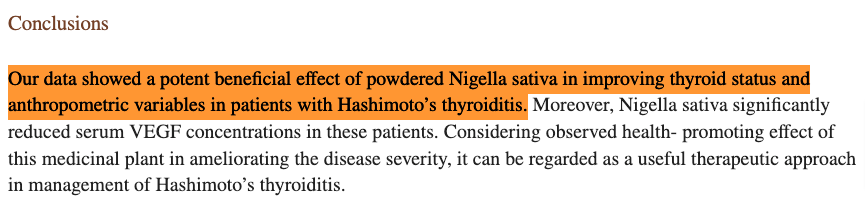
Even though this study was relatively small by most standards, the results are very impressive and are hard to ignore.
It’s very unusual to see these kinds of results and this kind of study for any natural therapy which is why I do frequently recommend the use of this plant for patients with Hashimoto’s.
While the study mentioned above used nigella sativa powder, I still believe you can replicate the results by using black seed oil.
Black seed oil is often better because it concentrates the active ingredients into an oil that can more easily be taken by patients.
You can even take it a step further by standardizing the concentrations of active ingredients like thymoquinone, P-cymene, carvacrol, and the free fatty acids found in black seeds for even better results.
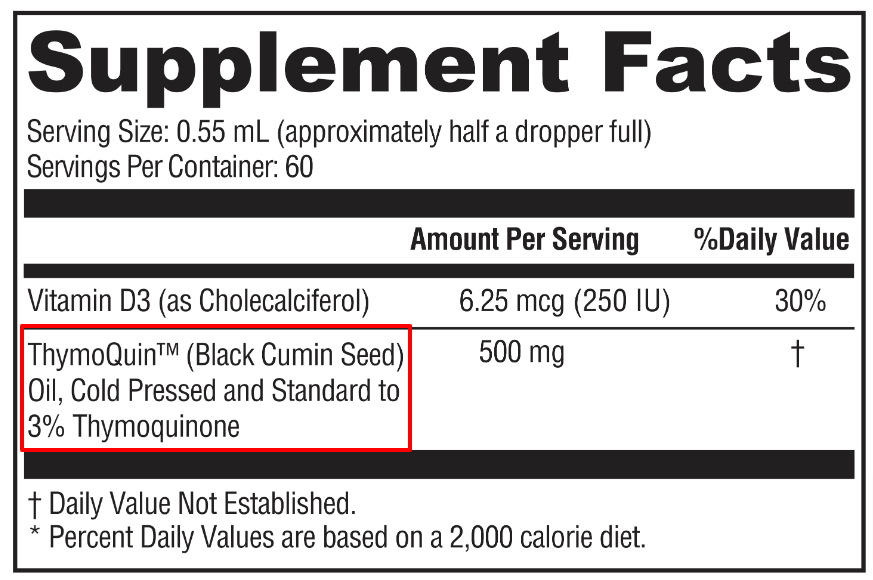
To get these benefits, I recommend using 1,000 mg of black seed oil each day for at least 90 days.
If you feel inclined, you can check your thyroid lab tests and antibody levels prior to using it and then recheck them after 3 months.
This isn’t required, by any means, but it’s a good idea to keep track of your lab tests so you can follow your progress.
Use a black seed oil like this one for the best results possible.
What is the Normal Range for TPO Antibodies?
In general, you will want your TPO antibodies to be as low as possible.
That means nonexistent or < 30 U/mL.
The reason for this is simple:
We know that the presence of antibodies indicates potential damage to the thyroid gland.
Getting your antibodies to as close to zero as possible ensures that these antibodies aren’t floating around in your bloodstream capable of inducing damage.
The standard reference range (2) for thyroid peroxidase antibodies (abbreviated as TPO antibodies) is given as a value less than some number.
This may sound ambiguous, but it’s just how it is.
In most cases, the “normal” range is given as less than 60 U/mL or even less than 30 U/mL.
If you pull out your own lab tests and compare, you may find that your reference range is a little bit different and that’s okay.
As long as you focus on getting your antibody levels to as close to zero as possible then you are on the right track.
More important than the absolute level of antibodies in your blood is the trend of those antibodies over time.
If you see those antibodies trending down as you integrate new treatments and therapies into your life then you’ll know you’re on the right track.
And by combining as many of the treatments we’ve discussed here as possible, you’ll give your body and thyroid the best shot they have at getting back to normal.
If you’re feeling a little overwhelmed by all of this information then I’d recommend reading this article next.
It outlines four meals that you can eat every single day to optimize your thyroid.
Scientific References
#1. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/autoimmune-disorders
#2. https://testdirectory.questdiagnostics.com/test/test-detail/7260/thyroid-peroxidase-and-thyroglobulin-antibodies?cc=MASTER
#3. https://www.ncbi.nlm.nih.gov/books/NBK459262/
#4. https://www.who.int/news-room/fact-sheets/detail/healthy-diet
#5. https://pubmed.ncbi.nlm.nih.gov/31275780/
#6. https://pubmed.ncbi.nlm.nih.gov/20413700/
#7. https://www.fammed.wisc.edu/files/webfm-uploads/documents/outreach/im/handout_elimination_diet_patient.pdf
#8. https://www.sciencedirect.com/science/article/pii/S0091302214000466
#9. https://pubmed.ncbi.nlm.nih.gov/25708485/
#10. https://www.ncbi.nlm.nih.gov/pubmed/8035512
#11. https://www.ncbi.nlm.nih.gov/pubmed/1917404
#12. https://www.ncbi.nlm.nih.gov/pubmed/22552705
#13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6047889/
#14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3719391/
#15. https://pubmed.ncbi.nlm.nih.gov/20351569/
#16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5405068/
#17. https://pubmed.ncbi.nlm.nih.gov/27256300/
#18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7167994/
#19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4056127/
#20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2833301/
#21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3962576/
#22. https://www.ncbi.nlm.nih.gov/pubmed/24526250
#23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5112739/