Have you been told that you have a low TSH?
Are you experiencing symptoms such as
It may surprise you to know that a low TSH can be associated with multiple conditions all of which present in different ways.
This article will go into detail on how to interpret your TSH, how to determine the cause, the symptoms associated with each cause, and further instructions on how you should proceed.
This article should be helpful if you have hyperthyroidism, hypothyroidism or pituitary issues (because all of these conditions can result in changes to your TSH level!).
Let’s jump in:
TSH as a Marker of Thyroid Function
Let’s briefly discuss what the TSH actually stands for and what it is a marker of.
TSH stands for thyroid stimulating hormone and it is a hormone that is produced by the pituitary gland in your brain.
TSH is one of the main methods that your body uses to control and tightly regulate thyroid function and control of your body.
The primary job of TSH, unsurprisingly, is to ‘stimulate’ your thyroid gland.
This stimulation results in the production of thyroid hormones, primarily T3 and T4.
Once these thyroid hormones are released into the bloodstream, they go through your body and interact with all of your cells to regulate your metabolism (1), help your body produce heat (2), help your heart beat, and your hair grow (3), and so on.

If you have a low amount of TSH in your body then your thyroid may not be getting the proper amount of ‘stimulation’ that it needs.
As you might guess, this can lead to some serious downstream side effects and consequences that are felt by you as certain symptoms.
There’s only one problem:
There are many different causes of TSH dysregulation (4) and each condition is associated with a different set of symptoms!
Luckily, you can differentiate between these conditions with a little bit of knowledge and some thyroid lab tests.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
5 Main Causes of Low TSH
As I mentioned previously, it’s actually very important that you understand the primary cause of your issue.
It’s possible to have a low TSH and have either the symptoms of hypothyroidism or hyperthyroidism, all depending on the underlying cause.
With that in mind, below you will find a list of the most common conditions that may result in a suppressed or low TSH.
You should be able to identify where you fit in, but in case you can’t, I’ve also included some follow-up tips at the end to help you further stratify yourself.
#1. Hyperthyroidism (Endogenous)
Perhaps the most common cause of low TSH is caused by what is known as endogenous hyperthyroidism (5).
The term hyperthyroidism refers to a state in which there is too much thyroid hormone floating around in the bloodstream.
The most common cause of hyperthyroidism is the autoimmune disease Graves’ disease in which your body autonomously (by itself) produces thyroid hormone without regard to the normal feedback loop.
As thyroid hormone is produced your body will attempt to normalize the amount by lowering the TSH.
But, if the thyroid gland is producing thyroid hormone through another stimulus (in this case through antibody stimulation) then it doesn’t slow down in response to the low TSH.
This cycle continues until the TSH is close to zero or very suppressed.
Endogenous hyperthyroidism should be differentiated from exogenous hyperthyroidism (6) which is caused by taking too much thyroid hormone medication and something we will discuss below.
Endogenous hyperthyroidism is hard to miss because you will often experience very significant symptoms which will lead you to your Doctor’s office.
In addition, you will also see other findings on your lab tests such as an elevation of thyroid-stimulating immunoglobulin (the autoimmune marker for Graves’ disease) and elevated free T3.
Symptoms associated with endogenous hyperthyroidism include:
- Hot flashes
- Weight loss
- Diarrhea
- Fatigue
- Nervousness
- Irritability
- Bone loss
- Heart palpitations
- Rapid resting heart rate
- Hair loss
These symptoms are hard to miss and they are often enough to identify the cause of your low TSH without further testing (but testing should still be used!).
#2. Thyroid Medication
Here’s where things can get a little bit tricky.
Some people, perhaps you, suffer from changes to their TSH as a result of taking thyroid medication.
Any thyroid medication that you take by mouth will influence your TSH level, provided that it is absorbed into your body.
This includes medications like Synthroid, levothyroxine, Armour Thyroid, Nature-throid, liothyronine, and Cytomel.
All thyroid medications have this effect.
It stems from a feedback loop that exists in your brain designed to help control how much thyroid hormone is produced at any given time.
Doctors take advantage of this feedback loop to help them determine how much thyroid hormone they should give to patients.
The topic of the value of TSH in determining your medication dose is something we can discuss in another place, but let me say here that TSH isn’t always the best marker to use (7).
But back to the TSH and thyroid medication for a moment.
As you take thyroid medication by mouth it will act to reduce your TSH.
The more medication you take the lower your TSH will go.
So, it’s certainly possible to take enough thyroid medication that it will suppress or lower your TSH.
But, does this mean you are hyperthyroid?
Does this mean that you have the same biologic condition as those patients who have endogenous hyperthyroidism?
The answer is both yes and no, and it depends on the patient and this is where it can get confusing.
It’s both possible to take an excessive amount of thyroid hormone, sufficient to reduce the dose and become hyperthyroid.

It’s also certainly possible to take thyroid hormone, enough to lower your TSH, but still remain clinically hypothyroid.
These two conditions present clinically on opposite ends of the spectrum.
If you have a low TSH due to taking thyroid medication and you are feeling hot, anxious, experiencing heart palpitations, feeling jittery, or losing your hair, then you may be on the hyperthyroid spectrum.
On the other hand, if you have a low TSH while taking thyroid medication and you are gaining weight, feeling fatigued, experiencing hair loss, suffering from constipation, and experiencing depression, then you are most likely biochemically hypothyroid, despite what your TSH says.
You can definitively differentiate between these two states by ordering free thyroid hormones which we will discuss later.
Symptoms associated with a low TSH due to thyroid medication include:
- Some patients experience hyperthyroid symptoms while others experience hypothyroid symptoms. Which set of symptoms you experience depends on what medication you are taking, the dose of that medication, and how well you are converting T4 to T3.
#3. Pituitary Dysfunction
We know that you can have a low TSH from either taking too much thyroid hormone by mouth or because your body is producing too much thyroid hormone on its own.
These two causes of low TSH occur due to the regulatory feedback loop that exists in your body.
But what if the organ which produces TSH is damaged and cannot produce this hormone?
That’s exactly what happens with pituitary dysfunction.
Remember:
Your pituitary gland (an organ in your brain) is the sole provider of TSH for the body.
If it becomes damaged, or injured in any way, then you will not be able to produce TSH (8).
If you don’t produce TSH then obviously your levels will fall because your body can’t get it from any other source.
And, as you might suspect, this results in symptoms that are often much different than those previously listed.
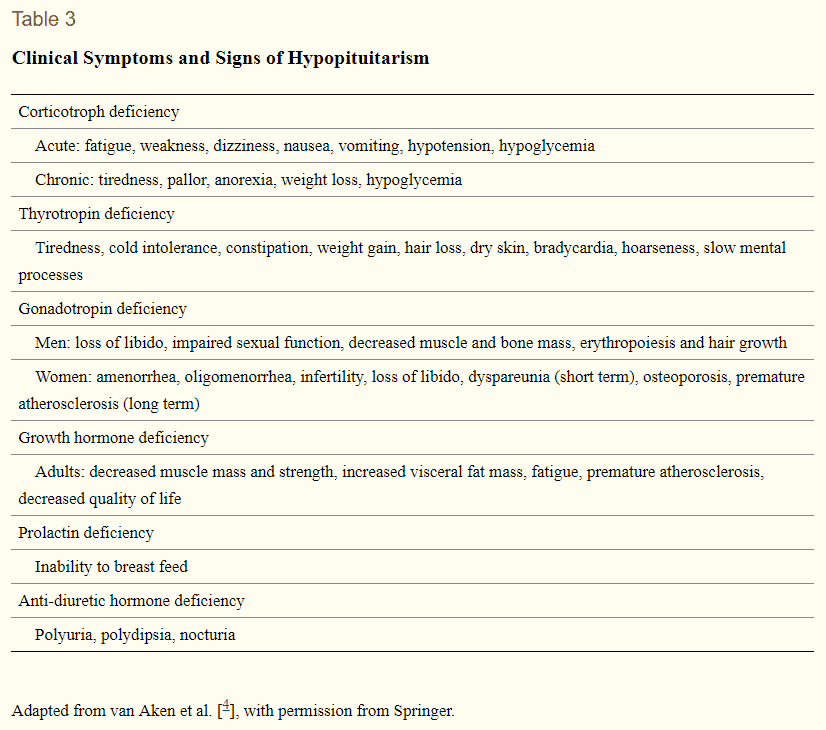
The reason for this has to do with the fact that your pituitary produces much more than just TSH.
It also produces other stimulating hormones including FSH, LH, ACTH, Prolactin, and Growth hormone.
If you have pituitary damage it’s very likely that your pituitary will not be able to these other important hormones as well.
If these stimulating hormones are not produced then they will not go around the body ‘stimulating’ the release of hormones and many of your normal hormone levels will drop.
This happens with your thyroid as well.
As TSH levels fall, your thyroid will no longer be stimulated and it will no longer produce sufficient levels of T4 and T3.
As your free thyroid hormone levels fall, you will start to experience the symptoms of hypothyroidism.
But, in addition, you may also experience symptoms associated with low testosterone, low estrogen, low progesterone, low growth hormone, and so on.
Pituitary damage can stem from trauma to the head, it can occur from tumors, and it can be caused by pregnancy due to lack of blood flow.
Symptoms associated with a low TSH due to pituitary dysfunction include:
- Symptoms of hypothyroidism: weight gain, hair loss, constipation, fatigue, depression, cold body temperature, cold intolerance, and so on.
- Other symptoms associated with low sex hormones include decreased libido, changes to your menstrual cycle, appetite changes, painful intercourse, vaginal dryness, changes to breast size/volume, and hot flashes.
#4. Lab Anomaly
Another important cause of low TSH is a lab anomaly.
What do I mean?
Believe it or not, your lab tests are not always accurate.
In fact, it’s been estimated that up to 3-5% of lab results are inaccurate at any given time (9).
What does this mean for you?
It means that, in some cases, your TSH may just be the result of a lab anomaly and there may not be any problems with it.
You can identify this problem quite easily because, if you fall into this category, you will most likely not experience any symptoms.
Furthermore, it’s very likely that your low TSH was identified through routine testing and not because you went to the Doctor for any specific problem.
If you fit into this problem then it’s very important that you not jump into treatment right away.
Instead, a better approach is to simply re-test your lab results after 6-8 week period and also look at other thyroid lab tests at that time.
This approach will prevent you from starting treatment unnecessarily which can be associated with problems by itself.
While this is not necessarily a common occurrence, it’s still worth considering because some small fraction of people will fit into this category.
Symptoms associated with a low TSH due to lab anomaly:
- There should not be any symptoms with this condition.
#5. Euthyroid Sick Syndrome
Another, relatively common, cause of low TSH is due to a condition known as euthyroid sick syndrome.
Euthyroid sick syndrome, referred to as ESS, is more of a constellation of changes that occur due to a specific stimulus on the body.
You can think of ESS as protective changes which occur when the body is under extreme stress.
The stress can be from any cause including severe illness, chronic illness (10), extreme dieting (11), extreme social stress (12), environmental exposure (13), and so on.
The theme that links all of these exposures is how the body reacts.
When you put your body under these specific influences it responds with a few changes in your thyroid gland including:
- A drop in TSH and TRH
- A drop in free T3 and total T3
- A rise in reverse T3
- A drop in T4 to T3 conversion
All of these changes result in one major change:
A reduction in thyroid hormone production and function in the body.
Sometimes this can be a good thing but sometimes it can work against your body and result in serious problems.
ESS is becoming more and more common as people are exposed to repeated stressors and as the condition is coming into light due to more advanced testing.
This condition is often missed unless tests beyond the TSH are ordered.
Simply ordering the TSH by itself may lead to a false conclusion that you have excess thyroid hormone in the body, but can be differentiated from this state by checking for free thyroid hormones.
The suppression or reduction in TSH that occurs in ESS stems from changes in the bloodstream picked up by your hypothalamus which directly influences TRH.
As TRH drops the TSH will follow and then free thyroid hormones will soon after.
Symptoms associated with a low TSH caused by euthyroid sick syndrome:
- This condition may or may not be associated with symptoms. Often, if it is associated with symptoms these symptoms will closely mimic those of hypothyroidism.
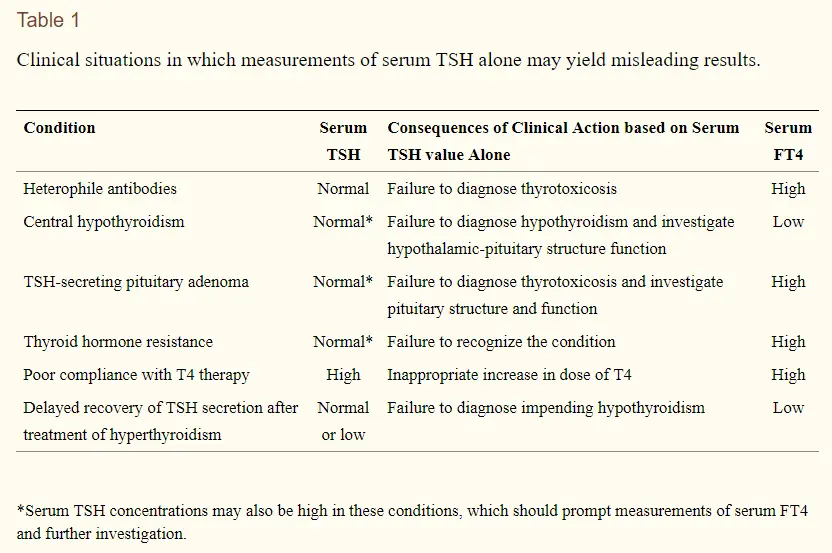
Further Testing is Often Necessary
In almost every case of low TSH, you will need to get more advanced testing done.
The TSH is the standard way physicians use to generally evaluate your thyroid, but there are many further tests that can and should be ordered.
The TSH only gives you a specific set of information about your pituitary gland but it doesn’t give you information about the amount of circulating free thyroid hormone in your body or about how well you are converting or utilizing thyroid hormone.
These factors can easily be evaluated by adding a few extra tests.
Tests that you will want to get beyond the TSH include:
- Free T3
- Total T3
- Free T4
- Reverse T3
- Thyroid antibodies (TSI antibodies, TPO antibodies, and TgAB)
These lab tests will help differentiate the various causes of low TSH and will help you have a better idea as to what is happening in your body.
Below you will find a list of lab patterns and how they match up with the conditions listed above:
- Low TSH, low free T3, low free T4, high reverse T3 – This pattern is seen in euthyroid sick syndrome.
- Low TSH, very high free T3, low free T4 – This pattern is seen in cases of endogenous hyperthyroidism such as Graves’ disease.
- Low TSH, high free T4, low free T3 – This pattern is usually seen with thyroid medication but doesn’t necessarily mean that you are hyperthyroid.
- Low TSH, normal free T3, normal free T4 – This pattern is seen with a lab anomaly.
- Low TSH, low free T4, low free T3, low reverse T3 – This pattern is seen in pituitary dysfunction.
Conclusion
This article highlights the importance of understanding thyroid physiology before jumping to conclusions, treatments, and diagnoses.
While TSH is a potentially great marker for assessing thyroid function, it falls short in a number of ways and can be misleading unless it is also evaluated in the context of other thyroid lab tests.
A low TSH can be caused by 5 main conditions, all of which are associated with various symptoms and can be differentiated from one another with further testing.
You can identify these conditions by looking at various thyroid lab patterns and determining where you fit in.
Now I want to hear from you:
Do you have a low TSH?
Do you know what is causing your TSH to drop or lower?
What other symptoms are you experiencing?
Are you undergoing treatment?
Leave your comments or questions below!