Low progesterone is more common than you might think.
If you’ve been dealing with changes to your mood, weight gain, or irregularities in your menstrual cycle then you might have low progesterone without realizing it.
Finding out if you have low progesterone is important because progesterone (along with estradiol/estrogen) helps maintain and keep in balance other hormone systems in your body.
Use this guide and low progesterone symptoms checklist to help determine if you have low progesterone, but more importantly what causes it and how to treat it:
The Complete List of Low Progesterone Symptoms
In the female body, progesterone fluctuates over time (throughout the month) to help keep estradiol in balance and maintain hormonal harmony.
Small imbalances in progesterone may result in very big symptoms due to the balancing effect that this hormone has cellularly and on other hormones.
When you couple this with the fact that even a few pounds of weight gain is enough to set progesterone in a tailspin you may begin to understand the importance of checking and treating your levels.
Why do we care so much about progesterone?
In the most basic sense progesterone is the perfect balance to estrogen in the body.
Most women don’t realize it but you actually have more progesterone than you have estrogen.
Progesterone directly counteracts and balances the growth hormone-like effects of estradiol and estrogens in the body.
While estrogen helps build tissue up (breast tissue, uterine tissue, fat cells) progesterone helps to slim down the exact same tissue.
This effect extends beyond tissues and even impacts your mood, sex drive, and emotions.
I’ve outlined the most common symptoms of low progesterone below. This checklist should be used in combination with your serum progesterone levels (more on that later).
If you do determine that you fit the symptoms of having low progesterone you will also want to try to find the underlying cause.
Low Progesterone Symptom Checklist:
- Sleep Disturbance (Insomnia)
- Water Retention or Bloating
- Emotional lability (irritability, depression, or other unexplained mood changes)
- Menstrual irregularities (if still menstruating)
- Uterine fibroids
- Breast Tenderness or breast pain
- Breast lumps or cysts
- Anxiety or difficulty relaxing
- Decreased libido or low sex drive
- Hot flashes (rare, but does occur)
- Breast tenderness and pain
- Premenstrual syndrome or symptoms consistent with PMDD
- History of Endometriosis or issues with fertility (1)
Note that some of these symptoms may be directly related to progesterone, but some may be related to the hormone imbalance that occurs when progesterone is low.
Remember that the balance of estrogen to progesterone is incredibly important in women.
For instance:
Low progesterone or high estrogen may result in similar symptoms as the ratio tips in favor of estrogen to progesterone.
In some cases, it may be difficult to distinguish low progesterone from high estrogen.
The vast majority of the time (at least in the United States) women suffer from low progesterone related to stress and age, and high estrogen related to weight gain and exposure to endocrine disruptors.
This means that a combination of therapy targeted at both lowering estrogen and increasing progesterone may be required for most women.
With that in mind, it’s important to understand what is considered “normal” as it relates to progesterone in your body.
Symptoms of Adequate Progesterone levels:
- Improved sleeping patterns (ease in falling asleep and staying asleep)
- Feeling more relaxed
- Reduced breast tenderness around cycle (if menstruating)
- Improved mood (reduced depression and irritability)
- Increased libido and sex drive
- Regular menstrual cycle
- Feeling more like “yourself” the last 2 weeks of your cycle
Remember:
The exact level and amount of progesterone that you need in your body will be different from other women.
The combination of the 3 major sex hormones (Testosterone, Progesterone, and Estradiol) come together to create your unique physiology.
If we lined up 100 healthy women and tested these 3 major hormones we would find high variability between each and every one.
We would also find differences in their menstrual cycles, bust size, body fat percentage, basal metabolic rate, and basal body temperature.
Why?
Because each woman is unique in the level of sex hormones that they possess, and it is these hormones that come together to help (in a major way) many of the attributes listed above.
The bottom line:
In most cases, you will need to use a combination of symptoms and serum progesterone levels to figure out what your “optimal” progesterone level truly is.
In most cases, you will find that there is some “trigger” or some “cause” of low progesterone that must be treated as well.
This brings us to our next topic:
What causes Low Progesterone?
The importance of this section is to outline that some (in fact many) causes of progesterone may actually be reversible.
This provides a unique opportunity for many of you.
Why?
Because we don’t necessarily want to increase your progesterone by brute force using bio-identical progesterone cream.
This may lead to unwanted symptoms such as weight gain, water retention, or bloating (you can read more about using progesterone for weight loss here).
It’s also important to remember that changes in 1 hormone system will almost always result in changes across multiple hormone systems.
This is why adding progesterone cream may be insufficient to seriously reduce your symptoms long term.
With that in mind let’s discuss the most common causes of low progesterone:
#1. Undiagnosed or Untreated Hypothyroidism
Remember when I said that your hormone systems are linked?
Thyroid hormone is a perfect example.
Adequate thyroid hormone and function are required for both regular ovulation (2) and progesterone production in the body.
Specifically, studies have linked T3 thyroid hormone (3) (the active thyroid hormone) to the release and cycle of healthy progesterone levels.

So what does this mean for you?
The incidence of hypothyroidism is estimated to be around 10% of the population (in the US) with subclinical hypothyroidism estimated to be about another 10%.
That means there is about a 20% chance that if you are reading this you have some issue with thyroid function.
What’s worse is that simply being overweight has also been shown to reduce thyroid function and T3 levels as well (this doesn’t take into account the effect that weight directly has on progesterone either).
When you couple the high rate of hypothyroidism and the current treatment paradigm that may leave many patients with suboptimal thyroid treatment (4) it becomes clear why testing your thyroid is high up on this list.
So what are you supposed to do?
If you have low progesterone make sure you get a complete thyroid panel and evaluate both your total T3 and free T3 levels.
Example of the complete thyroid panel:
- TSH
- Free T3
- Free T4
- Reverse T3
- Total T3
- Thyroid antibodies
You can find relevant information on how to address thyroid hormone imbalances on my blog and in the links above.
#2. History of Birth Control Use
Another big reason for low progesterone among young women is the judicious use of birth control pills as a catch-all therapy for any PMS-like symptoms.
The idea behind birth control pills (when not used as a contraceptive) is to completely suppress the normal homeostasis and cycle of your hormones throughout the month.
Doses of synthetic and pharmaceutically derived hormones are given to women to suppress the normal ovulatory pattern.
In some women using oral contraceptives may help temporarily reduce symptoms, but it does nothing to treat the underlying cause.
In addition, some women suffer from complications related to taking birth control medications such as infertility (5), weight gain, acne, and worsening symptoms.
The bottom line?
Taking suppressive doses of synthetic hormones may result in suppressed progesterone levels after you discontinue taking OCP.
This effect seems to be worse in some women and they develop a condition known as post-birth control syndrome.
This constellation of symptoms likely relates to the dysregulation of normal hormonal systems (remember the menstrual cycle is quite complex with alternating levels of multiple hormones and hormone precursors throughout the month) that occur from long-term birth control use.
Just remember that taking any hormone (synthetic or bio-identical) may have consequences on the regulatory systems in your body.
In most cases using bio-identical hormones (if necessary) is preferred over synthetic and pharmaceutically derived variations of progesterone.
Most physicians have no problem prescribing synthetic hormones to control symptoms but balk when you discuss bio-identical hormones.
Why your Doctor would prefer a pharmaceutical derivative of a natural hormone over the exact replica of the hormone that your body has evolved to use over thousands of years is beyond me, but this is the world we live in.
#3. Weight Gain
Excess weight (even 10+ pounds) is enough to increase the risk that you will develop endometrial cancer.
Studies have suggested that this increase in risk is related to how obesity alters estrogen and progesterone levels (6):

Excess weight (those with a BMI of > 30) leads to a combination of the following:
- Excess estrogen or estrogen dominance
- Hyperinsulinemia or insulin resistance (think PCOS-like symptoms)
- Increase in inflammatory markers
- Increase in IGF-1 (growth hormone to all cells including cancer)
These negative consequences seem to hit some women harder than others, but we can all agree that having excess weight is NOT healthy for the metabolic systems in your body.
The good news is that this cascade of negative changes can be opposed by balancing and increasing progesterone.
Increasing progesterone (by taking bio-identical progesterone in this study) resulted in balancing estrogen dominance (reducing the cellular effect of estrogen), normalizing IGF-1 levels, and normalizing the expression of progesterone receptors on cells.
Taking progesterone may reduce some of these negative effects and reduce your risk of developing endometrial cancer but it may not be sufficient to help with weight loss.
You can find more information on how to achieve long-lasting weight loss through hormone balancing in my 60-day weight loss guide.
#4. Age
Age is another inevitable cause of low progesterone in every woman.
Starting at around age 35 your progesterone levels will start to drop until menopause at which point they will become very low and stay there (unless you supplement).
This is important to note because even without hormone imbalances, weight gain, thyroid disorders, etc. your progesterone will STILL lower slowly over time.
Let’s illustrate this concept with a graph:

In the graph above you can see progesterone in the red line and estrogen (estradiol) in the dark line.
As you can see, both hormones estrogen and progesterone eventually drop off to very low levels starting from age 35.
The important thing to note here is the rather dramatic decline of progesterone RELATIVE to estrogen that occurs after age 35.
Remember that it is the ratio of progesterone to estrogen that we are most worried about, not necessarily the absolute values of progesterone or estrogen.
This dramatic decline in progesterone results in relative estrogen dominance in most women from around age 40 to menopause which may result in the symptoms listed in the first section of this blog post.
This decline can largely be delayed with a healthy lifestyle, maintaining a normal weight, and ensuring proper hormone balance as you age.
#5. Menopause
Along the same lines as the age-related decline of progesterone is the decline of progesterone that occurs in EVERY woman after menopause.
Menopause is the absence of ovulation that all women will eventually go through.
Because ovulation is responsible for the majority of progesterone produced in the female body it’s easy to understand that when ovulation fails progesterone will subsequently fall to near-zero levels.
There are many supplements and therapies that you can undergo to reduce the symptoms associated with menopause and fight the decline in both estrogen and progesterone.
I’ve outlined these therapies and supplements in this post.
#6. Excessive Stress And/or Adrenal Burn Out
Stress might be the most common reason for low progesterone in women in the US.
People tend to undervalue the potency and effect that chronic and sustained stress has on the physiologic processes in the body.
Acute levels of stress have been shown to spike both cortisol and progesterone (7), as outlined below in the graph:
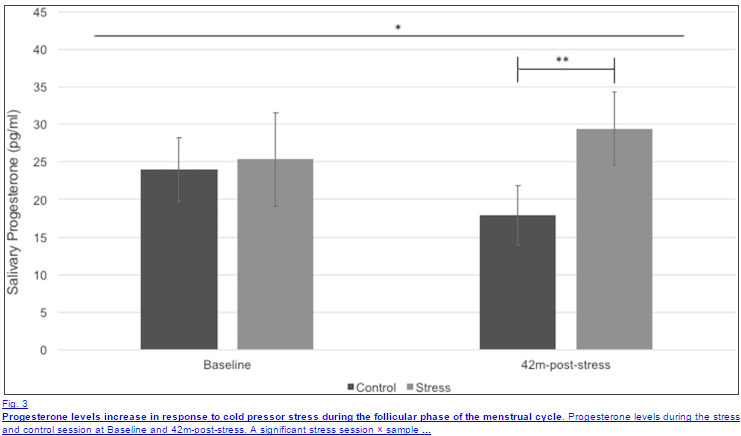
Long-term stress, on the other hand, has quite a different effect on progesterone.
Sustained stress leads to changes in adrenal hormones which may result in higher-than-normal cortisol and lower-than-normal progesterone.
This phenomenon has been termed “pregnenolone steal” to highlight the adrenal preference to create pregnenolone (and therefore cortisol) over progesterone.
Chronic stress also leads to changes in thyroid physiology by increasing the conversion of T4 to reverse T3.
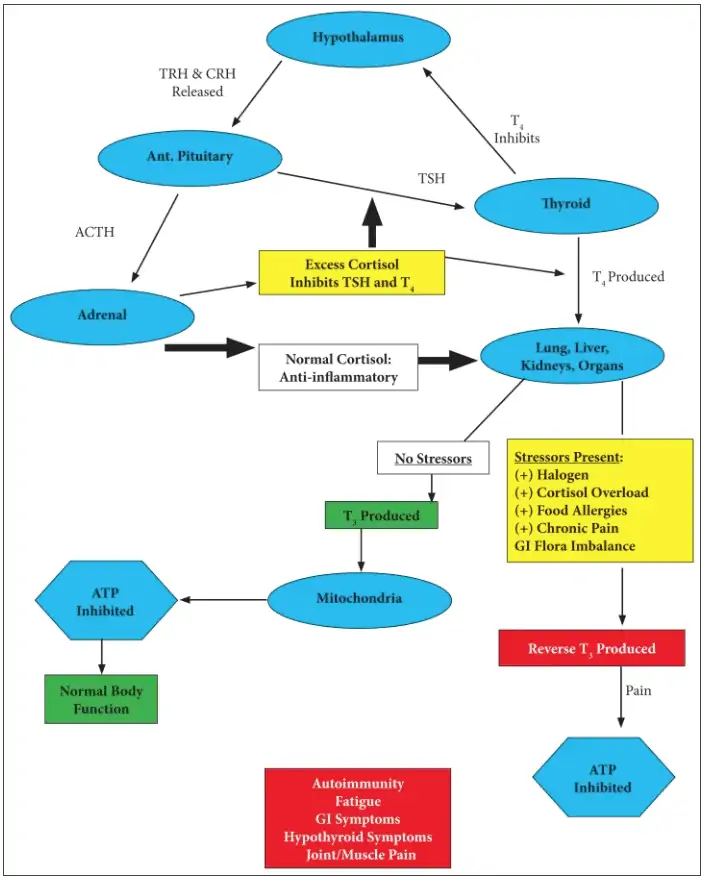
The net effect of decreased thyroid hormone is a reduction in ATP and energy production along with cellular hypothyroidism.
You already know that hypothyroidism will lead to progesterone, so now we have a stress-thyroid-low progesterone connection.
What kind of stress are we referring to?
Pretty much any type of stressor may impact the adrenal system: physiologic, lack of sleep, emotional stress, physical/traumatic, etc.
It seems that emotional stress, such as rejection from peers or social stress (8), impacts progesterone more than other types of stress.
Regardless of the source of your stress, the bottom line is that it must be treated.
That means it needs to be eliminated (if possible).
In addition, many patients find benefits in using certain supplements to augment the effects of reducing stressors to regulate cortisol levels in the body.
You can find a full list of supplements that can help adrenal-related problems in this post.
#7. Sensitivity to Xenoestrogens or Endocrine Disruptors
This is a topic that certainly doesn’t get enough attention, so it’s worth elaborating on what exactly I am talking about when I say endocrine disruptors and xenoestrogens.
Endocrine disruptors (otherwise known as EDCs) are chemicals that interfere with normal hormone balance in the body (9).
Whether you realize it or not you are being exposed to these chemicals on a daily basis.
I’ve included all of the areas in which we come into contact with these chemicals in the figure below:
- Commercial and processed foods (soy milk)
- Lipophilic chemicals in industrial factors that process foods
- Lipophilic chemicals in industrial agriculture/livestock facilities
- Pesticides/fungicides directly on the food
- Phyto-estrogens within certain foods
- Synthetic hormones (think oral contraceptives) which are metabolized and recycled in the body
- Transdermal exposure through cosmetics (makeup, hair spray, lotions, etc.)
- Inhalation (hair spray, paint, etc.)
- Oral exposure through foods
- Storage of endocrine disruptors in adipose (fat) and breast milk
- Embryonic exposure -> transfer from the mother to the child
- Transfer to offspring through lactation and breastfeeding
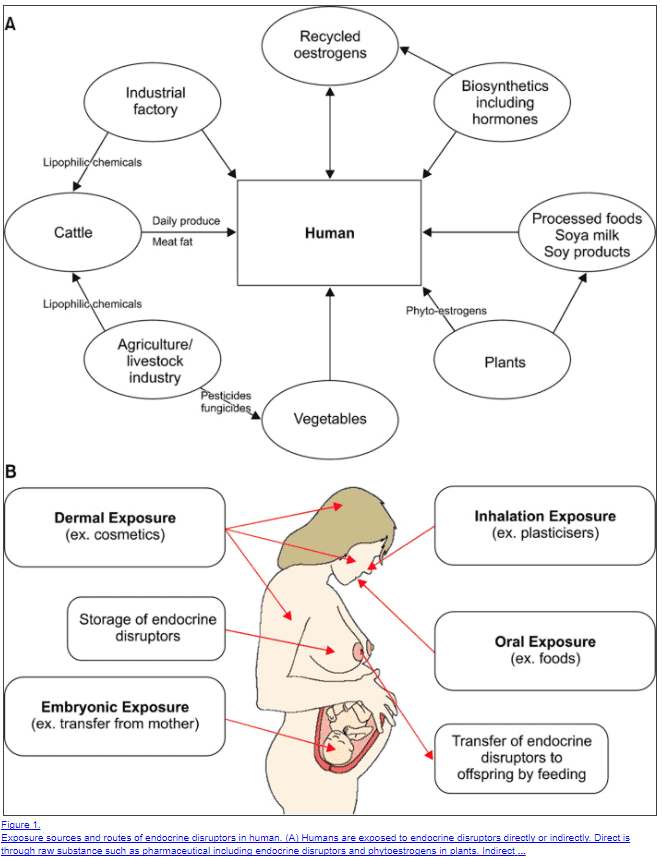
It’s easy to see that you are coming into contact with these chemicals and endocrine-disrupting chemicals on a daily basis.
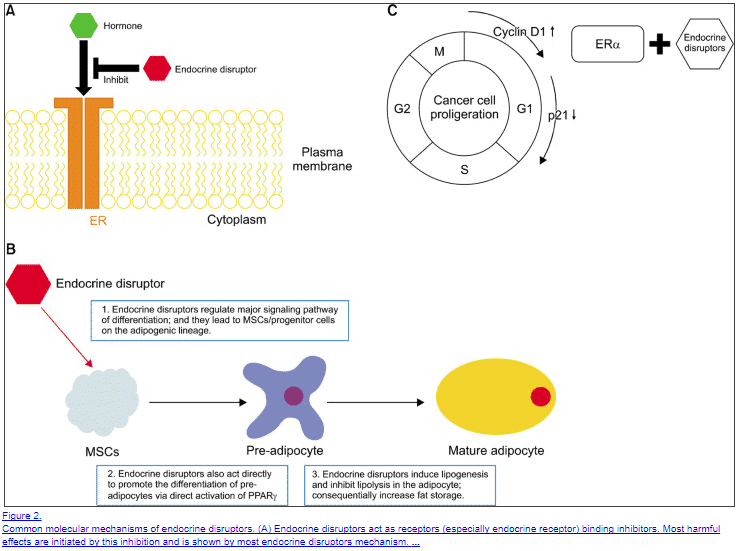
But here’s the deal:
Some people seem to tolerate EDCs better than others.
And, it seems that EDCs take time to build up in your system before they start to cause trouble with your hormones.
This means that some people will naturally have higher levels than others when we consider that some people avoid fewer chemicals in their life or simply have higher activity of phase II liver detoxification enzymes.
The result is that EDCs may be playing a big role in some people and a smaller role in others.
EDCs work by “mimicking” the effects of traditional and regular hormones and by blocking the cellular binding of these native hormones.
The net result is an increase in estrogen a reduction in progesterone (10) and an increase in fat mass.
One big problem with EDCs is that they limit lipogenesis (the burning of fat) which promotes more EDC storage and build-up over time.
So how do you get rid of them?
First and foremost you want to avoid them at all costs.
Secondly, you can improve the elimination of these chemicals by increasing certain enzymes in your liver (those involved in phase II Detoxification pathways (11)).
You can do this by taking certain supplements:
- Milk thistle + MCM + NAC – Take 2 capsules of this supplement daily for 2-3 months.
- Calcium D-glucarate – Take up to 2 grams per day for 10-14 days in a row then take a 1-2 week break.
- Vitamin C (buffered) – At least 2-5 grams daily. If you experience diarrhea simply back down on your dose.
Third(ly?) you need to drink enough water, ensure that you have proper bowel movements, and make sure that have frequent deep sweats.
#8. Cellular Progesterone Resistance (As seen in PCOS & Endometriosis)
This is an emerging concept that has been shown to at least play a role in patients with endometriosis and PCOS.
The idea is that your cells become resistant to the effects of progesterone (12) in the presence of high estrogen levels (estrogen dominance).
This same scenario occurs in leptin resistance, insulin resistance, and thyroid resistance.
As hormone levels in the body increase, your body has a protective mechanism that downregulates receptor activity to certain hormones.
The effect is a temporary reduction in cellular activity but it usually results in abnormal serum labs that don’t match the symptoms of the patient.
Likewise, progesterone resistance creates a scenario in which serum progesterone levels may be “normal” but cellular resistance is occurring which creates the symptoms of low progesterone (which can make diagnosis difficult).
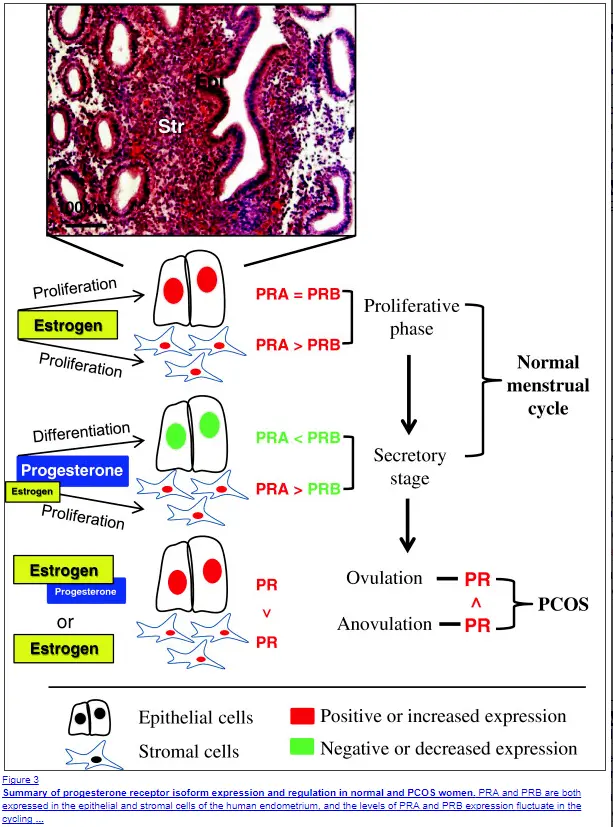
Progesterone resistance tends to occur in patients who ALSO have insulin resistance, higher than normal IGF-1 levels, and high serum estrogen.
It is felt that certain cells may coexpress receptors for insulin, IGF-1, estradiol, and progesterone.
This means that an increase in ANY of these hormones may result in the downregulation of progesterone receptors which leads to progesterone resistance.
Another big problem for women who have progesterone resistance is that taking progesterone will NOT improve the situation and may make your symptoms worse.
This phenomenon may explain why some women who take progesterone, even with low levels, experience negative side effects.
The good news?
This condition can be treated.
Studies have shown that metformin actually helps reverse progesterone resistance (13).
This is good news because it indicates that reversing insulin resistance (which is what metformin does) actually sensitizes your cells to progesterone.
Treatment of progesterone resistance should, therefore, focus on the treatment of existing hormone resistance syndromes and THEN the replacement of progesterone.
Testing your Progesterone
Next up on the list is how to determine if you actually have low progesterone.
Luckily, it’s actually quite easy to diagnose with simple lab tests.
But first, let me show you an example:
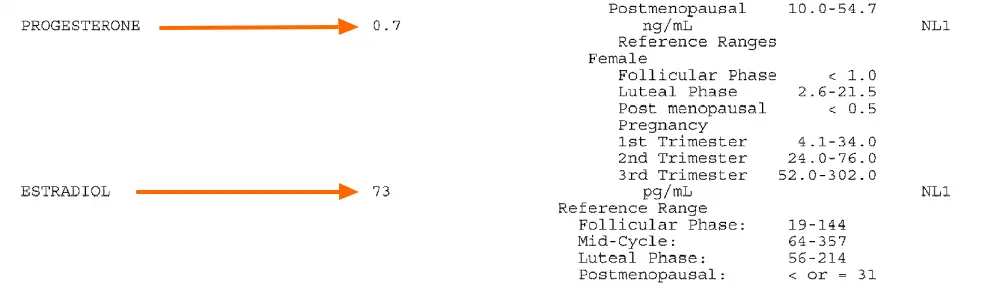
This is a serum lab test of both progesterone and estradiol.
You can see in this example that the serum progesterone level is 0.7 ng/mL while the estradiol level is 73 pg/mL.
This set of labs was drawn on day 20 of this patient’s menstrual cycle, which is when progesterone should be at its peak.
This data suggests that this patient has low progesterone (the reason is unclear with just lab data).
In this set of data, we can see that this patient is indeed experiencing low progesterone and estrogen dominance during this cycle.
You can test yourself by assessing BOTH progesterone and estradiol on days 19-21 of your cycle.
Just remember that serum lab testing won’t necessarily work for each person. Some people may need more extensive testing such as DUTCH urine testing or estrogen metabolite testing.
But it’s relatively easy to start out with a simple serum progesterone/estradiol ratio.
Bio-Identical Progesterone Cream
We’ve discussed several treatment options up until this point but we haven’t really discussed how to correctly use progesterone (and if you should).
If you determine that you have low progesterone (through a combination of serum testing and symptoms) then you may want to consider supplementation of bio-identical progesterone.
You should proceed cautiously when using progesterone, however, especially if you suspect that you may have progesterone resistance.
Why?
Because taking progesterone without addressing the underlying causes of progesterone resistance may worsen your symptoms.
If you decide to proceed with progesterone then I recommend a trial of progesterone cream.
This should be used based on your age and if you are cycling (or not).
You can find relevant information on how to use progesterone safely below:
How to Supplement with Bioidentical progesterone
- If menstruating: Use 20-40mg per day on days 14-28 of your cycle (the latter half of the month)
- If in menopause: you can use 20-40mg per day either 6 days per week (with rest on the 7th) or 26-28 days per month (with 1-3 days off per month)
- Make sure to monitor your symptoms while using and discontinue use if you experience any negative side effects
- Discuss the use of bioidentical hormones with your physician
Back to you
Progesterone is very common among women in the united states – both menstruating and postmenopausal women.
Treating low progesterone starts with the proper evaluation of both your symptoms and serum lab testing.
If your progesterone is low you may find a significant reduction in symptoms such as bloating, weight gain and depression.
Some women may experience worsening of symptoms when supplementing with progesterone which should trigger an evaluation for progesterone resistance.
But now I want to hear from you:
Do you have the symptoms of low progesterone?
Have you used progesterone cream in the past?
Did it work for you? Why or why not?
Leave your comments below!