If you were to ask your doctor how long you need to take thyroid medication the answer you would probably get is forever.
That’s a pretty scary thought for many thyroid patients and it causes them a lot of hesitancy in even starting the medication in the first place.
After all, wouldn’t you think twice before starting something that you would then have to take forever?
I don’t blame patients for having second thoughts but there are several problems with this proposition:
The first? If you really need something, you shouldn’t have an option of using it or not.
If your body actually needs thyroid medication then it just needs it, it doesn’t necessarily matter whether you want to take it or not.
Thyroid hormone is not something you can live without, so if your doctor is suggesting that you “might” need it then perhaps they are unsure of your diagnosis or they are trying to put you on treatment too early.
And second, the idea that you have to take thyroid medication forever isn’t really grounded in reality.
The standard thought process among doctors is that once you start taking thyroid medication, you will simply have to take it for life.
They say this because hypothyroidism is considered a chronic disease (1), one for which there is no known cure.
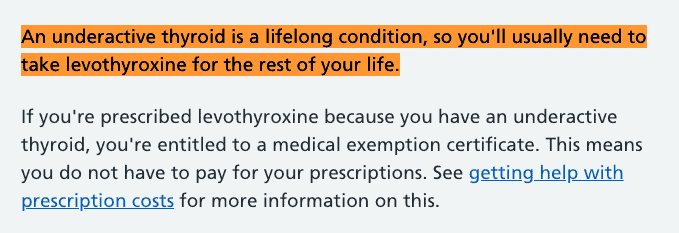
*Image text screenshot is from nhs.uk website showing how conventional medicine looks at thyroid hormone medication.
So if you start treatment for an incurable disease, then the logic is that you will need to take that treatment forever.
But, again, this isn’t actually true.
There are many conditions that result in temporary hypothyroidism for which thyroid medication may be temporarily useful but not necessarily required long-term.
There are also situations in which patients have been incorrectly placed on thyroid medication due to unknown reasons.
Whatever the reason, we know that somewhere between 10-33% of patients taking thyroid medication likely do not need to be on it.
You don’t have to take my word for it either, you can just take a look at studies like this one (2).
The evidence for this is still emerging and is considered fairly weak right now, but the direction it is heading is very promising.
It suggests that there are absolutely situations in which thyroid patients may be able to get off of their thyroid medication without taking it for life.
But we have a big problem:
This data is new and emerging so doctors aren’t aware of it (3) and, for now, they tend to lump thyroid patients into the massive category of hypothyroidism without considering whether or not their specific issue is life-long or temporary.
Based on what we know right now, the key to understanding how long you need to take thyroid medication depends on whether or not your hypothyroidism is considered reversible or irreversible.
Let’s talk about how to figure out which camp you fall in.
Understanding Why Thyroid Patients Need Thyroid Medication
This is a pretty basic idea but it is something that is often missed by thyroid patients so let’s talk about it right now.
Why do thyroid patients even need thyroid medication?
It’s actually simple and I alluded to it above:
Thyroid hormone is something that human beings can’t live without.
Not only is it required for life, but it’s also necessary to enjoy the life that you live!
You can survive with a low level of thyroid hormone in your body (hypothyroidism), but you probably wouldn’t enjoy your existence.
It would be riddled with all sorts of problems such as fatigue, weight gain, cold intolerance, hair loss, depression, anxiety, menstrual problems, muscle pain, acid reflux, rashes, and so on.
If your body stopped producing thyroid hormone completely then, yes, eventually you could die but that doesn’t really happen in developed countries.
Before that occurs, most people end up in their doctor’s office complaining of the symptoms I mentioned above and looking for a solution.
The solution they are offered? Thyroid medication.
Unfortunately, thyroid medication doesn’t always solve all of these issues, at least not 100%, which leaves thyroid patients feeling stuck.
They feel like they can’t control their symptoms, they feel like their medication may even make some of them worse, and they often feel unheard by their doctor.
This can sometimes lead these patients to believe that the thyroid medication they were given is part of the problem.
The reality couldn’t be farther from the truth.
Thyroid hormone is most likely the solution, they were just given the wrong type or dose.
You can read a whole lot more about this idea and how to solve it here.
If you’ll notice, pretty much everything we’ve discussed so far is more about managing your symptoms and not about finding what caused them.
This is very important because it’s the reason that many thyroid patients end up on thyroid medication longer than they need to.
Here’s what I mean:
The symptoms you present with tell your doctor that you have low thyroid function but they don’t tell you why.
And we know that there are many potential reversible causes of hypothyroidism.
So it very well may be the case that your low thyroid function is real, but is something that is treatable or can be managed with time.
This isn’t always the case, though, as there are many permanent causes of hypothyroidism, but there are enough reversible causes for this to impact up to 1/3 of patients taking thyroid medication.
And, after hearing this, you might think it would be easy to identify when your thyroid function returns to normal but you’d be wrong.
Once you start taking thyroid medication, for any reason, it will have a suppressive effect on your body’s ability to produce its own thyroid hormone.
This happens with all hormones.
Once you start taking thyroid hormone, the normal feedback loops in your brain slow down because your body recognizes that it’s getting thyroid hormone from some other source.
And unless you try to take yourself off of thyroid medication, there’s no way to know if your own body is capable of producing thyroid hormone on its own.
In other words, you could be sitting here reading this with a thyroid gland that is capable of working but you’d never know because the thyroid medication you are taking is blocking it from doing so.
This is the situation that up to 1/3 of thyroid patients may be in, and is the topic of a lot of ongoing research.
It’s unclear why this happens but one theory this occurs has to do with the difference between reversible and irreversible causes of hypothyroidism.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Reversible Causes of Hypothyroidism
Reversible causes of hypothyroidism are those causes that result in the temporary slowing of your thyroid gland.
Initially, these states would be indistinguishable from irreversible causes of hypothyroidism because they would both result in the same set of symptoms and the same set of labs.
This means both sets of conditions would likely result in treatment with thyroid medication and a recommendation for life-long use.
The primary difference, though, is that, eventually, your own thyroid gland may return to normal function either because of things that you do to help it get there or because of time.
Here’s a list I put together that includes some potentially reversible causes of hypothyroidism.
*Image screenshot is taken from medscape.com.
By the way, as you look at this list and the one below, you will find that some conditions make an appearance on both.
This is not a mistake!
Many medical conditions exist on a spectrum and may be more severe or less severe depending on many factors.
More severe conditions may result in permanent thyroid gland damage and less severe versions may not.
Hypothyroidism caused by Hashimoto’s (in some but not all cases)
Hashimoto’s thyroiditis is the #1 cause of hypothyroidism in developed countries and it’s the result of an autoimmune disease.
In some cases, Hashimoto’s can be managed or put into remission with aggressive early treatment.
This isn’t always possible but when it is, you may be able to restore or improve thyroid gland function to pre-disease levels.
Treatment with natural therapies like diet, supplements, lifestyle changes, and even off-label prescription medications may help you get there.
In general, the earlier you diagnose and treat Hashimoto’s, the higher your likelihood of remission.
Unfortunately, if you’ve had Hashimoto’s for several decades, you likely have some degree of permanent thyroid gland damage which means this is not possible (see more information below).
If you have hypothyroidism and you’ve never been checked for Hashimoto’s, you should do that as soon as possible because the likelihood that your thyroid disease is caused by this autoimmune disease is very high.
Hypothyroidism caused by iodine deficiency
Iodine deficiency is a known reversible cause of hypothyroidism and a primary cause of goiter (4).
Iodine intake is required for thyroid hormone creation in the thyroid gland and a deficiency means you are unable to create enough for the demands of your body.
In cases of hypothyroidism caused by iodine deficiency, taking iodine supplements is enough to completely fix the issue and return thyroid function to normal.
In previous decades, iodine intake wasn’t a huge problem due to the fortification of iodine in foods but iodine intake has consistently declined in recent years and may be an emerging problem for many people and thyroid patients.
For these reasons, it’s always a good idea to ensure that you are taking a daily dose of iodine within the RDA of 150 to 300mcg.
This ensures that you don’t need to worry about iodine deficiency and these low levels are not enough to cause thyroid problems which can occur with very high doses.
Hypothyroidism caused by other nutrient deficiencies
Aside from iodine, deficiencies in other nutrients have been shown to depress thyroid function to levels that may cause hypothyroidism.
Some of the most important include selenium deficiency (5) (especially if combined with iodine deficiency), vitamin A deficiency (usually seen in developing countries (6)), zinc deficiency (7) (particularly common among the elderly), and iron deficiency (8) (very common among women due to the menstrual cycle).
These nutrients are necessary for regulating thyroid function, iodine metabolism, thyroid conversion, and thyroid cellular function.
Some have a more profound impact on thyroid function and thyroid lab tests than others, but all have the potential to impact thyroid symptoms.
Nutrient deficiencies are often a solvable problem as well meaning you may have low levels but due to supplements or dietary changes, that can change relatively quickly.
It may be the case that there are many thyroid patients out there with suboptimal levels of key nutrients that impact thyroid function to a degree that results in hypothyroidism but these problems may be addressed with lifestyle changes.
We don’t know how common these nutrient deficiencies are in thyroid patients (at least not exactly) but it’s my experience that they certainly do play a role. It’s a good idea to take stock of these basic nutrients and use supplements to replace them as needed.
Hypothyroidism caused by stress
Stress can have a profound impact on all hormones in the body including thyroid hormone (9).
One single bout of stress is probably not enough to result in significant depression to thyroid function but consistent daily stress, or repeated bouts of extreme stress, might be.
The stress I am talking about here would be something you might experience with the passing of a loved one (spouse, child, or parent) or the result of a particularly nasty or hostile divorce or something similar.
This is the type of stress that impacts your sleep, your eating habits, your mood, and so on.

Depending on the degree of the stressful event, it may take your body years to recover.
But the key here is that it will eventually recover. In helping thousands of thyroid patients over the years, I’ve found that many cases can be traced back to a single stressful event.
If you can remember, think back to when you first were diagnosed with hypothyroidism and what was happening in your life at that time.
If it was anywhere near a major stressful event then this may have contributed to your thyroid status.
Hypothyroidism caused by illness
It is well known that illness has a negative impact on many different thyroid lab tests including TSH, free t3, free t4, and reverse T3.
To the untrained eye, these changes can look like hypothyroidism when, in reality, these changes are the result of something called euthyroid sick syndrome.
The changes to thyroid lab tests that occur during illness are felt to have some evolutionary advantage in that they divert resources from things that don’t matter (such as hair growth, skin health, and nail health) to things that do matter (such as immune system function and heart health).
These changes are felt to be completely reversible and will, eventually, return to normal once your illness has passed or resolved.
This issue doesn’t usually manifest for minor illnesses such as sinus infections, but it can become an issue for severe issues like pneumonia, heart attacks, stroke, or any other condition that would lead you to the hospital.
Your body can recover pretty quickly from a sinus infection but a more severe issue like a heart attack will have lingering effects on the body and thyroid for a long time.
If you happen to be tested or diagnosed during your recovery period, then you may be incorrectly diagnosed with hypothyroidism and placed on thyroid medication.
It’s also worth pointing out here that there is likely a situation in which chronic low-grade illness may contribute to true hypothyroidism but may be misdiagnosed as euthyroid sick syndrome. Cases of chronic Lyme disease (10) and long covid (11), would fit into this category.
Hypothyroidism caused by dieting
Many people don’t realize this but dieting has a profound negative impact on thyroid function!
We know this from starvation studies (12) but I’ve also had the advantage of testing thyroid function in patients who have just recently undergone extreme dietary restrictions from things like the hCG diet.
And when I tested these patients, their thyroid lab patterns look just like hypothyroidism.
They show very high levels of reverse t3, low t3, and changes to their TSH. These changes to thyroid function result as your metabolism declines in response to your calorie restriction.
The good news is that these changes are temporary, the bad news is that recovery can take years and that during your recovery period, you will look and feel hypothyroid.
If you go to your doctor during this period then you may be diagnosed with hypothyroidism and placed on thyroid medication.
Hypothyroidism caused by prescription medications
Thyroid patients are often concerned to learn that many prescription medications can negatively impact thyroid function (13).
The degree to which these medications interfere with your thyroid varies, but it is well known that they have the potential to.
Some prescription medications can cause permanent problems while others may cause alterations to thyroid lab tests or thyroid function that can vary from problematic to unproblematic depending on the person.
In some cases, you may be able to solve this issue by trying a new medication in a different class.
In other situations, it may be required for you to take that medication because the side effects of not taking it are too severe.
If you find that you are taking any of the medications on this list then touch base with your doctor to see if there are alternatives for your personal situation.
Here is a list of some of the more common medications that can do this:
- amiodarone
- Thalidomide
- Tyrosine kinase inhibitors
- interferon
- rifampin
- phenobarbitol
- carbamazepine
- lithium
- interleukin-2
- predinose
- dopamine
- opioids
- metformin
- anti-depressants
- acid blockers
- sucralfate
- bile acid sequestrants
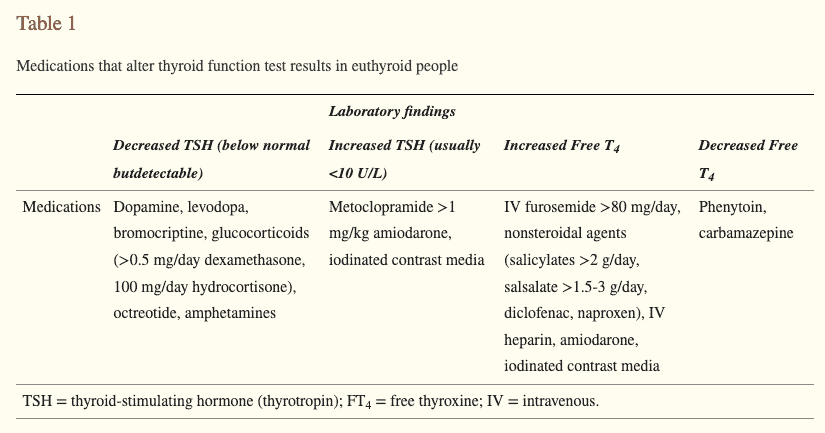
Hypothyroidism caused by sub-acute thyroiditis
A relatively uncommon cause of temporary hypothyroidism is a direct thyroid gland infection.
Yes, your thyroid gland can become infected, just like any other part of your body, it just doesn’t happen very often because it’s relatively contained and protected compared to other tissues like your lungs or sinuses.
Infections of the thyroid gland are referred to as subacute thyroiditis.
The name given to this condition explains everything you need to know.
Subacute means it usually lasts a few months and thyroiditis refers to inflammation.
Most people with an infection of the thyroid gland start out with hyperthyroidism which then transitions to hypothyroidism (14) which eventually transitions to normal thyroid function.
It’s usually hard to miss this condition because it’s one of the few diseases of the thyroid gland that causes thyroid gland pain, but it’s possible that it could be.
If the initial diagnosis was missed then you could be placed on thyroid medication during the hypothyroid phase and kept on it indefinitely.
There are also some people who benefit from temporarily taking thyroid medication just for symptom control, and if that’s you, then you should know it is very likely that you will only need it for a short period of time.
Hypothyroidism caused by postpartum thyroiditis
Postpartum thyroiditis is another inflammatory condition of the thyroid gland that can temporarily cause hypothyroidism which is often reversible.
It occurs in about 5% of women in the first year after they give birth.
In most cases, it is temporary, though it can sometimes also progress to permanent hypothyroidism.
Thyroid function can vary during the course of this disease but there is often a hypothyroid period.
Because it is a very similar condition to Hashimoto’s thyroiditis (it’s another form of autoimmune thyroiditis), it’s possible to confuse the two conditions. If that’s the case, you could be prematurely diagnosed with permanent autoimmune thyroiditis when the reality is that your condition may only be temporary.
You can get an idea if you are at risk for developing this condition by testing your thyroid antibodies in the third trimester of pregnancy.
Women who have elevated thyroid peroxidase antibodies in the third trimester of pregnancy have about an 80% chance of developing postpartum thyroiditis (15).
If you are currently pregnant or trying to get pregnant then you should be aware of this condition.
Misdiagnosed hypothyroidism from lab error or biotin
Finally, you should be aware that lab tests are not as accurate as you might think!
This is important because lab testing is almost always part of the diagnosis of hypothyroidism.
But there are many factors that can influence the accuracy of your thyroid lab tests.
Some of the more common include ingredients that interfere with the thyroid testing assay like biotin but there are times when lab tests are just inaccurate due to problems in the laboratory (16).
I’ve seen many situations where patients are told they have a huge thyroid problem and yet their symptoms don’t align with that diagnosis at all.
It isn’t until they get their thyroid retested that they realize something is wrong with the first set of lab tests.
Always make sure that your thyroid lab tests align with your symptoms. If there is an inconsistency between the two then it never hurts to retest your thyroid gland.
After all, what’s one more needle poke compared to a life-long use of thyroid medication?
Irreversible Causes of Hypothyroidism
We’ve spent a lot of time discussing those issues that result in temporary or reversible hypothyroidism so it now only makes sense to discuss those conditions which are irreversible.
Below you will find a list of conditions that, if present, mean you will need to take thyroid medication for the rest of your life.
This harkens back to my original statements discussing the need for thyroid hormone by the body and for not only surviving but for thriving as well.
Hypothyroidism caused by thyroid removal (thyroidectomy)
Unfortunately, if your thyroid gland has been completely removed then you will need to take thyroid medication for life.
The only workaround here is if only half of your thyroid gland has been removed.
As long as you still contain some thyroid tissue then that remaining thyroid gland tissue can enlarge and sometimes make up for the missing portion.
Very rarely, thyroid patients can have their thyroid gland completely removed and still not need thyroid medication.
This happens in rare cases when there is extra-thyroidal tissue in another place of the body (17) such as the chest or near the tongue. This is very rare but I’ve seen it happen before.
Hypothyroidism caused by radioactive iodine ablation (RAI)
The purpose of radioactive iodine ablation therapy is to destroy the thyroid gland and, if the thyroid gland is destroyed, you will need to take thyroid medication for life.
The only exception to this rule is if your ablation was unsuccessful because you were given an insufficient dose of radiation.
Nowadays this isn’t very common, but it used to be more common dating back to 30 or 40 years ago.
For most people who undergo radioactive ablation therapy, they can expect that 100% of their thyroid gland has been removed.
Hypothyroidism caused by end-stage Hashimoto’s thyroiditis
Hashimoto’s is one of those conditions that can either be reversible or irreversible, depending on the circumstance.
If left unattended for decades, Hashimoto’s will eventually result in the complete destruction of your thyroid gland and create a situation that is similar to that of thyroidectomy or RAI.
You can identify if you are in this stage by evaluating your thyroid gland with an ultrasound.
In end-stage Hashimoto’s, an ultrasound will show an atrophied (shrunken) thyroid gland that is non-functional.
Unfortunately, once you get to this state you will be required to take thyroid medication for life.
Hypothyroidism caused by empty sella syndrome (ESS)
Empty sella syndrome can be both an acquired condition or a genetic condition (18) (depending on the circumstance) which can negatively impact pituitary function.
In some cases, ESS is found incidentally and has no impact on thyroid or hormone function.
We won’t discuss these cases because they aren’t important for our discussion.
If you do have a version of ESS that results in hypothyroidism, then that condition will be permanent and irreversible.
This is because the thyroid is regulated at several steps including two which are found in the brain.
Whether your problem is with the thyroid gland itself or with the portions of the brain that regulate thyroid hormone, the result is the same: you will most likely need to take thyroid medication for life.
Hypothyroidism caused by pituitary or hypothalamic problems
As I just mentioned, thyroid function is regulated at three important levels:
- At the level of the hypothalamus
- At the level of the pituitary gland
- And at the level of the thyroid gland
If you have a genetic or permanent problem with any of these three systems then you may end up with irreversible hypothyroidism.
In cases of pituitary and hypothalamus dysfunction, it may very well be the case that your thyroid gland is perfectly capable of producing thyroid hormone if it had the right stimulation.
Unfortunately, though, problems in the pituitary gland and the hypothalamus block this stimulation.
Here are a few examples of irreversible problems of the hypothalamus and the pituitary gland (19):
- Pituitary tumors
- Tumors that compress the hypothalamus
- Sheehan syndrome
- TRH deficiency
- Radiation to the brain
- Infiltrative disorders like sarcoidosis or amyloidosis
These conditions are pretty uncommon and rare compared to those we have discussed thus far but it’s still important to include them here.
Hypothyroidism caused by some prescription medications
Most of the time, prescription medications only cause a temporary hypothyroidism which is lifted once the offending medication is removed.
This isn’t always the case, though, at least for some medications.
Two notable exceptions include amiodarone and lithium.
Amiodarone is used for certain heart conditions (20), so those who are using it, often really need to use it.
Lithium is considered a mood stabilizer (21) and is often used for conditions such as bipolar disorder.
Again, those who are taking lithium are taking it because they have usually exhausted other options and must take it for mood regulation.
Both of these medications may result in permanent hypothyroidism if they are taken for a long period of time.
There is no guarantee that this will happen, but there have been studies that show that it can occur.
If you are taking either of these medications then be sure to check with your doctor to see if they are absolutely required or if you may be able to try another option.
If they aren’t an option, just realize that long-term use of either of these may result in the need for thyroid medication for life.
Thyroid cancer
Finally, we have thyroid cancer.
Even though thyroid cancer itself has the potential to cause thyroid dysfunction, it’s usually caught long before this occurs.
That’s doctors will often say that if you are going to have a cancer, thyroid cancer is the one to have.
Try telling that to thyroid cancer patient survivors, though!
Thyroid cancer almost always results in irreversible hypothyroidism because treatments almost always include 100% removal of the thyroid gland (22).
As a result, thyroid cancer survivors are classified in the group of thyroidectomy patients that require thyroid hormone for life.
Some surgeons are opting to take a less aggressive approach to thyroid removal (23) in certain thyroid cancers so you may be able to get away with removing only a portion of your thyroid gland in some cases.
This is always preferable to a complete thyroidectomy whenever possible!
Be sure to discuss this option with your surgeon prior to your surgery but realize that leaving in a portion of your thyroid gland does place you at a slightly higher risk for cancer recurrence.
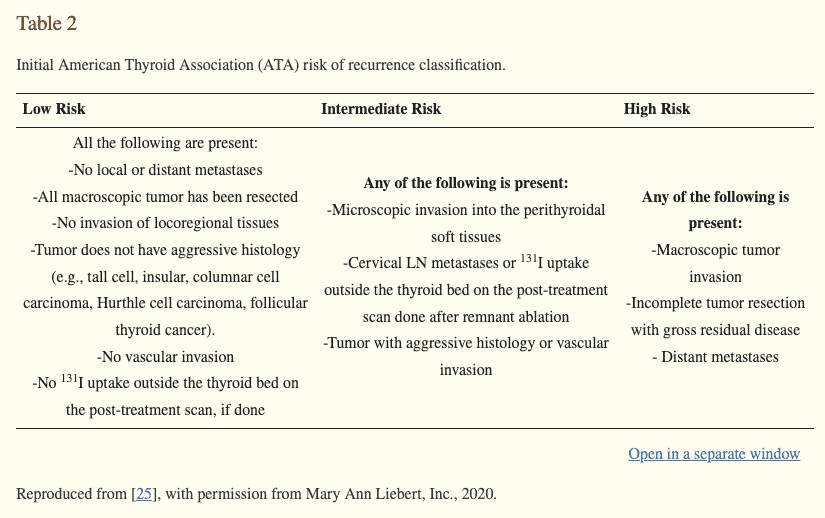
This risk may be worth it, though, if it means a much better quality of life for the rest of your life.
How Do You Know If You Can Stop Taking Thyroid Medication?
If you’ve been placed on thyroid medication at some point in your life, and you just got done reading this, then you are probably asking yourself if you are someone who must continue to take it.
Unfortunately, right now we don’t have a great way to assess whether someone is likely to be able to stop taking their thyroid medication short of trial and error.
There’s a lot of research going into this topic, though, and there may be better guidelines in the future.
Based on what we know right now, here are some guidelines that, if present, indicate that you have a solid chance of being able to get off of your thyroid medication:
- A history of thyroid medication use for less than 4 years in total
- The presence of normal free T4 levels with your original diagnosis
- If your current TSH is less than 1.8
- If your dose of thyroid medication is 50mcg or less
- If you are a woman (women are twice as likely to get off of their thyroid medication compared to men)
Be aware that this information only applies if you have a potentially reversible cause of hypothyroidism!
Even if you fit the criteria above but have an irreversible cause of hypothyroidism, it won’t help you as your body will require thyroid medication for life.
If you are interested in learning more about getting off of thyroid medication (referred to as deprescribing) then I would recommend reading this detailed article.
Wrapping it Up
Thyroid medication is not something you should be scared of taking but it’s also not something you should take if you don’t have to.
Many thyroid patients have been told that they need to take their medication for the rest of their lives but that isn’t always the case.
The main point in determining whether or not you must take your thyroid medication forever is whether or not the underlying cause of your hypothyroidism is reversible or irreversible.
Use the list above to try and categorize your hypothyroidism and, if possible, you can then determine whether a trial of deprescribing makes sense for your unique situation
Now I want to hear from you:
Have you been told that you must take thyroid medication for life?
How many years have you been taking your thyroid medication?
Do you know if your hypothyroidism is considered reversible or irreversible?
Have you tried getting off of your thyroid medication? If so, how did it work for you?
Leave your questions or comments below!
Scientific References
#1. nhs.uk/conditions/underactive-thyroid-hypothyroidism/treatment/
#2. ncbi.nlm.nih.gov/pmc/articles/PMC8110016/
#3. ncbi.nlm.nih.gov/pmc/articles/PMC3241518/
#4. ncbi.nlm.nih.gov/pmc/articles/PMC4049553/
#5. ncbi.nlm.nih.gov/pmc/articles/PMC7783124/
#6. pubmed.ncbi.nlm.nih.gov/15531495/
#7. ncbi.nlm.nih.gov/pmc/articles/PMC3746228/
#8. ncbi.nlm.nih.gov/pmc/articles/PMC6166193/
#9. pubmed.ncbi.nlm.nih.gov/21032895/
#10. ncbi.nlm.nih.gov/pmc/articles/PMC6963229/
#11. ncbi.nlm.nih.gov/pmc/articles/PMC9305273/
#12. pubmed.ncbi.nlm.nih.gov/1436373/
#13. pubmed.ncbi.nlm.nih.gov/20578900/
#14. ncbi.nlm.nih.gov/books/NBK279084/
#15. ncbi.nlm.nih.gov/books/NBK557646/
#16. ncbi.nlm.nih.gov/pmc/articles/PMC2851209/
#17. eje.bioscientifica.com/view/journals/eje/165/3/375.xml#
#18. ninds.nih.gov/health-information/disorders/empty-sella-syndrome
#19. ncbi.nlm.nih.gov/pmc/articles/PMC3169862/
#20. ncbi.nlm.nih.gov/pmc/articles/PMC3474631/
#21. pubmed.ncbi.nlm.nih.gov/19942149/
#22. cancer.org/cancer/thyroid-cancer/treating/surgery.html
#23. ncbi.nlm.nih.gov/pmc/articles/PMC7692138/