Low progesterone is more common than you might think.
If you’ve been dealing with changes to your mood, weight gain, or irregularities in your menstrual cycle then you might have low progesterone without realizing it.
Finding out if you have low progesterone is important because progesterone (along with estradiol/estrogen) helps maintain and keep in balance other hormone systems in your body.
Use this guide and low progesterone symptoms checklist to help determine if you have low progesterone, but more importantly what causes it and how to treat it:
The Complete List of Low Progesterone Symptoms
In the female body, progesterone fluctuates over time (throughout the month) to help keep estradiol in balance and maintain hormonal harmony.
Small imbalances in progesterone may result in very big symptoms due to the balancing effect that this hormone has cellularly and on other hormones.
When you couple this with the fact that even a few pounds of weight gain is enough to set progesterone in a tailspin you may begin to understand the importance of checking and treating your levels.
Why do we care so much about progesterone?
In the most basic sense progesterone is the perfect balance to estrogen in the body.
Most women don’t realize it but you actually have more progesterone than you have estrogen.
Progesterone directly counteracts and balances the growth hormone-like effects of estradiol and estrogens in the body.
While estrogen helps build tissue up (breast tissue, uterine tissue, fat cells) progesterone helps to slim down the exact same tissue.
This effect extends beyond tissues and even impacts your mood, sex drive, and emotions.
I’ve outlined the most common symptoms of low progesterone below. This checklist should be used in combination with your serum progesterone levels (more on that later).
If you do determine that you fit the symptoms of having low progesterone you will also want to try to find the underlying cause.
Low Progesterone Symptom Checklist:
- Sleep Disturbance (Insomnia)
- Water Retention or Bloating
- Emotional lability (irritability, depression, or other unexplained mood changes)
- Menstrual irregularities (if still menstruating)
- Uterine fibroids
- Breast Tenderness or breast pain
- Breast lumps or cysts
- Anxiety or difficulty relaxing
- Decreased libido or low sex drive
- Hot flashes (rare, but does occur)
- Breast tenderness and pain
- Premenstrual syndrome or symptoms consistent with PMDD
- History of Endometriosis or issues with fertility (1)
Note that some of these symptoms may be directly related to progesterone, but some may be related to the hormone imbalance that occurs when progesterone is low.
Remember that the balance of estrogen to progesterone is incredibly important in women.
For instance:
Low progesterone or high estrogen may result in similar symptoms as the ratio tips in favor of estrogen to progesterone.
In some cases, it may be difficult to distinguish low progesterone from high estrogen.
The vast majority of the time (at least in the United States) women suffer from low progesterone related to stress and age, and high estrogen related to weight gain and exposure to endocrine disruptors.
This means that a combination of therapy targeted at both lowering estrogen and increasing progesterone may be required for most women.
With that in mind, it’s important to understand what is considered “normal” as it relates to progesterone in your body.
Symptoms of Adequate Progesterone levels:
- Improved sleeping patterns (ease in falling asleep and staying asleep)
- Feeling more relaxed
- Reduced breast tenderness around cycle (if menstruating)
- Improved mood (reduced depression and irritability)
- Increased libido and sex drive
- Regular menstrual cycle
- Feeling more like “yourself” the last 2 weeks of your cycle
Remember:
The exact level and amount of progesterone that you need in your body will be different from other women.
The combination of the 3 major sex hormones (Testosterone, Progesterone, and Estradiol) come together to create your unique physiology.
If we lined up 100 healthy women and tested these 3 major hormones we would find high variability between each and every one.
We would also find differences in their menstrual cycles, bust size, body fat percentage, basal metabolic rate, and basal body temperature.
Why?
Because each woman is unique in the level of sex hormones that they possess, and it is these hormones that come together to help (in a major way) many of the attributes listed above.
The bottom line:
In most cases, you will need to use a combination of symptoms and serum progesterone levels to figure out what your “optimal” progesterone level truly is.
In most cases, you will find that there is some “trigger” or some “cause” of low progesterone that must be treated as well.
This brings us to our next topic:
What causes Low Progesterone?
The importance of this section is to outline that some (in fact many) causes of progesterone may actually be reversible.
This provides a unique opportunity for many of you.
Why?
Because we don’t necessarily want to increase your progesterone by brute force using bio-identical progesterone cream.
This may lead to unwanted symptoms such as weight gain, water retention, or bloating (you can read more about using progesterone for weight loss here).
It’s also important to remember that changes in 1 hormone system will almost always result in changes across multiple hormone systems.
This is why adding progesterone cream may be insufficient to seriously reduce your symptoms long term.
With that in mind let’s discuss the most common causes of low progesterone:
#1. Undiagnosed or Untreated Hypothyroidism
Remember when I said that your hormone systems are linked?
Thyroid hormone is a perfect example.
Adequate thyroid hormone and function are required for both regular ovulation (2) and progesterone production in the body.
Specifically, studies have linked T3 thyroid hormone (3) (the active thyroid hormone) to the release and cycle of healthy progesterone levels.

So what does this mean for you?
The incidence of hypothyroidism is estimated to be around 10% of the population (in the US) with subclinical hypothyroidism estimated to be about another 10%.
That means there is about a 20% chance that if you are reading this you have some issue with thyroid function.
What’s worse is that simply being overweight has also been shown to reduce thyroid function and T3 levels as well (this doesn’t take into account the effect that weight directly has on progesterone either).
When you couple the high rate of hypothyroidism and the current treatment paradigm that may leave many patients with suboptimal thyroid treatment (4) it becomes clear why testing your thyroid is high up on this list.
So what are you supposed to do?
If you have low progesterone make sure you get a complete thyroid panel and evaluate both your total T3 and free T3 levels.
Example of the complete thyroid panel:
- TSH
- Free T3
- Free T4
- Reverse T3
- Total T3
- Thyroid antibodies
You can find relevant information on how to address thyroid hormone imbalances on my blog and in the links above.
#2. History of Birth Control Use
Another big reason for low progesterone among young women is the judicious use of birth control pills as a catch-all therapy for any PMS-like symptoms.
The idea behind birth control pills (when not used as a contraceptive) is to completely suppress the normal homeostasis and cycle of your hormones throughout the month.
Doses of synthetic and pharmaceutically derived hormones are given to women to suppress the normal ovulatory pattern.
In some women using oral contraceptives may help temporarily reduce symptoms, but it does nothing to treat the underlying cause.
In addition, some women suffer from complications related to taking birth control medications such as infertility (5), weight gain, acne, and worsening symptoms.
The bottom line?
Taking suppressive doses of synthetic hormones may result in suppressed progesterone levels after you discontinue taking OCP.
This effect seems to be worse in some women and they develop a condition known as post-birth control syndrome.
This constellation of symptoms likely relates to the dysregulation of normal hormonal systems (remember the menstrual cycle is quite complex with alternating levels of multiple hormones and hormone precursors throughout the month) that occur from long-term birth control use.
Just remember that taking any hormone (synthetic or bio-identical) may have consequences on the regulatory systems in your body.
In most cases using bio-identical hormones (if necessary) is preferred over synthetic and pharmaceutically derived variations of progesterone.
Most physicians have no problem prescribing synthetic hormones to control symptoms but balk when you discuss bio-identical hormones.
Why your Doctor would prefer a pharmaceutical derivative of a natural hormone over the exact replica of the hormone that your body has evolved to use over thousands of years is beyond me, but this is the world we live in.
#3. Weight Gain
Excess weight (even 10+ pounds) is enough to increase the risk that you will develop endometrial cancer.
Studies have suggested that this increase in risk is related to how obesity alters estrogen and progesterone levels (6):

Excess weight (those with a BMI of > 30) leads to a combination of the following:
- Excess estrogen or estrogen dominance
- Hyperinsulinemia or insulin resistance (think PCOS-like symptoms)
- Increase in inflammatory markers
- Increase in IGF-1 (growth hormone to all cells including cancer)
These negative consequences seem to hit some women harder than others, but we can all agree that having excess weight is NOT healthy for the metabolic systems in your body.
The good news is that this cascade of negative changes can be opposed by balancing and increasing progesterone.
Increasing progesterone (by taking bio-identical progesterone in this study) resulted in balancing estrogen dominance (reducing the cellular effect of estrogen), normalizing IGF-1 levels, and normalizing the expression of progesterone receptors on cells.
Taking progesterone may reduce some of these negative effects and reduce your risk of developing endometrial cancer but it may not be sufficient to help with weight loss.
You can find more information on how to achieve long-lasting weight loss through hormone balancing in my 60-day weight loss guide.
#4. Age
Age is another inevitable cause of low progesterone in every woman.
Starting at around age 35 your progesterone levels will start to drop until menopause at which point they will become very low and stay there (unless you supplement).
This is important to note because even without hormone imbalances, weight gain, thyroid disorders, etc. your progesterone will STILL lower slowly over time.
Let’s illustrate this concept with a graph:

In the graph above you can see progesterone in the red line and estrogen (estradiol) in the dark line.
As you can see, both hormones estrogen and progesterone eventually drop off to very low levels starting from age 35.
The important thing to note here is the rather dramatic decline of progesterone RELATIVE to estrogen that occurs after age 35.
Remember that it is the ratio of progesterone to estrogen that we are most worried about, not necessarily the absolute values of progesterone or estrogen.
This dramatic decline in progesterone results in relative estrogen dominance in most women from around age 40 to menopause which may result in the symptoms listed in the first section of this blog post.
This decline can largely be delayed with a healthy lifestyle, maintaining a normal weight, and ensuring proper hormone balance as you age.
#5. Menopause
Along the same lines as the age-related decline of progesterone is the decline of progesterone that occurs in EVERY woman after menopause.
Menopause is the absence of ovulation that all women will eventually go through.
Because ovulation is responsible for the majority of progesterone produced in the female body it’s easy to understand that when ovulation fails progesterone will subsequently fall to near-zero levels.
There are many supplements and therapies that you can undergo to reduce the symptoms associated with menopause and fight the decline in both estrogen and progesterone.
I’ve outlined these therapies and supplements in this post.
#6. Excessive Stress And/or Adrenal Burn Out
Stress might be the most common reason for low progesterone in women in the US.
People tend to undervalue the potency and effect that chronic and sustained stress has on the physiologic processes in the body.
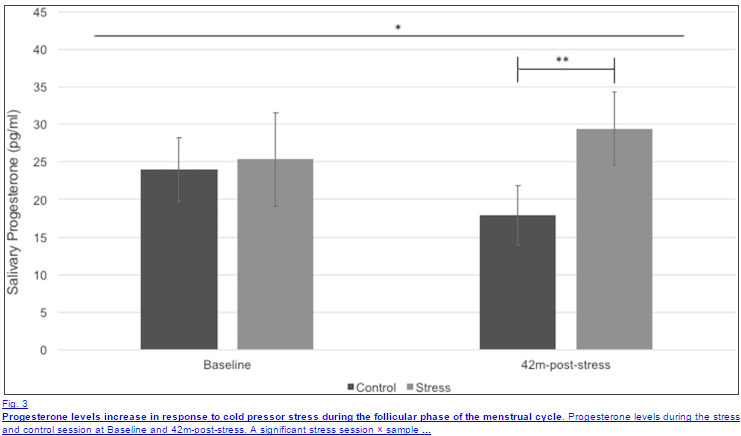
Acute levels of stress have been shown to spike both cortisol and progesterone (7), as outlined below in the graph:
Long-term stress, on the other hand, has quite a different effect on progesterone.
Sustained stress leads to changes in adrenal hormones which may result in higher-than-normal cortisol and lower-than-normal progesterone.
This phenomenon has been termed “pregnenolone steal” to highlight the adrenal preference to create pregnenolone (and therefore cortisol) over progesterone.
Chronic stress also leads to changes in thyroid physiology by increasing the conversion of T4 to reverse T3.
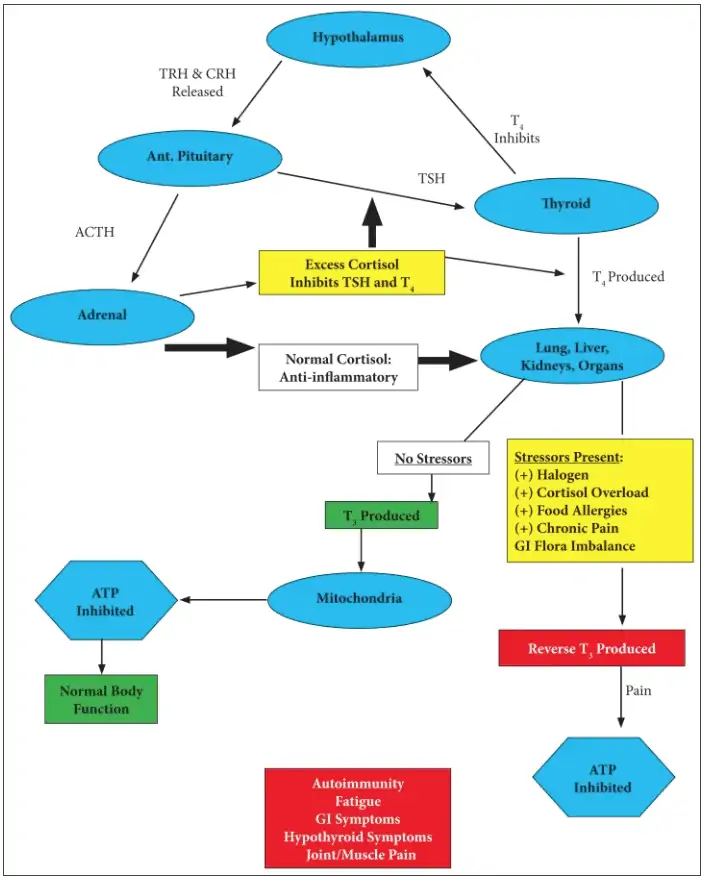
The net effect of decreased thyroid hormone is a reduction in ATP and energy production along with cellular hypothyroidism.
You already know that hypothyroidism will lead to progesterone, so now we have a stress-thyroid-low progesterone connection.
What kind of stress are we referring to?
Pretty much any type of stressor may impact the adrenal system: physiologic, lack of sleep, emotional stress, physical/traumatic, etc.
It seems that emotional stress, such as rejection from peers or social stress (8), impacts progesterone more than other types of stress.
Regardless of the source of your stress, the bottom line is that it must be treated.
That means it needs to be eliminated (if possible).
In addition, many patients find benefits in using certain supplements to augment the effects of reducing stressors to regulate cortisol levels in the body.
You can find a full list of supplements that can help adrenal-related problems in this post.
#7. Sensitivity to Xenoestrogens or Endocrine Disruptors
This is a topic that certainly doesn’t get enough attention, so it’s worth elaborating on what exactly I am talking about when I say endocrine disruptors and xenoestrogens.
Endocrine disruptors (otherwise known as EDCs) are chemicals that interfere with normal hormone balance in the body (9).
Whether you realize it or not you are being exposed to these chemicals on a daily basis.
I’ve included all of the areas in which we come into contact with these chemicals in the figure below:
- Commercial and processed foods (soy milk)
- Lipophilic chemicals in industrial factors that process foods
- Lipophilic chemicals in industrial agriculture/livestock facilities
- Pesticides/fungicides directly on the food
- Phyto-estrogens within certain foods
- Synthetic hormones (think oral contraceptives) which are metabolized and recycled in the body
- Transdermal exposure through cosmetics (makeup, hair spray, lotions, etc.)
- Inhalation (hair spray, paint, etc.)
- Oral exposure through foods
- Storage of endocrine disruptors in adipose (fat) and breast milk
- Embryonic exposure -> transfer from the mother to the child
- Transfer to offspring through lactation and breastfeeding
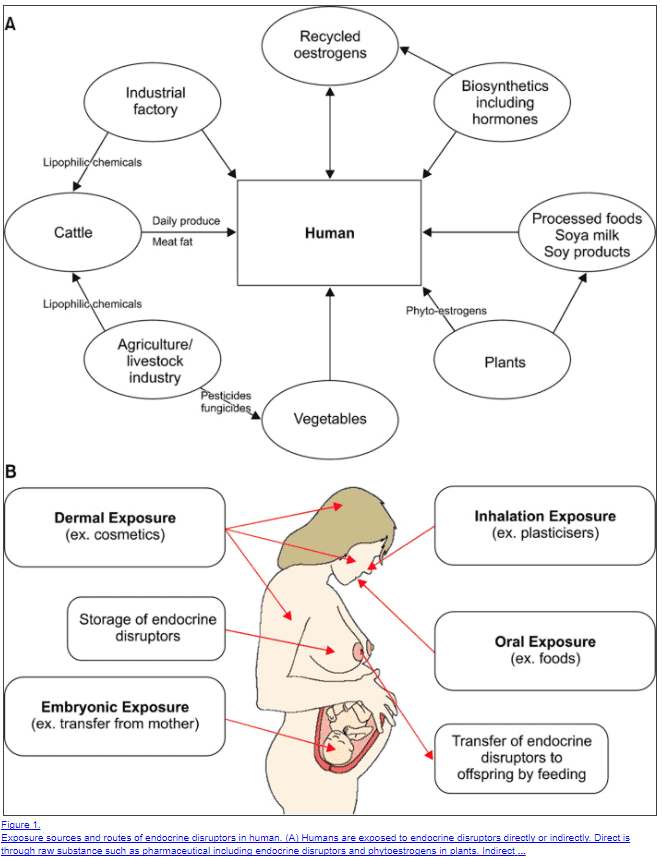
It’s easy to see that you are coming into contact with these chemicals and endocrine-disrupting chemicals on a daily basis.
But here’s the deal:
Some people seem to tolerate EDCs better than others.
And, it seems that EDCs take time to build up in your system before they start to cause trouble with your hormones.
This means that some people will naturally have higher levels than others when we consider that some people avoid fewer chemicals in their life or simply have higher activity of phase II liver detoxification enzymes.
The result is that EDCs may be playing a big role in some people and a smaller role in others.
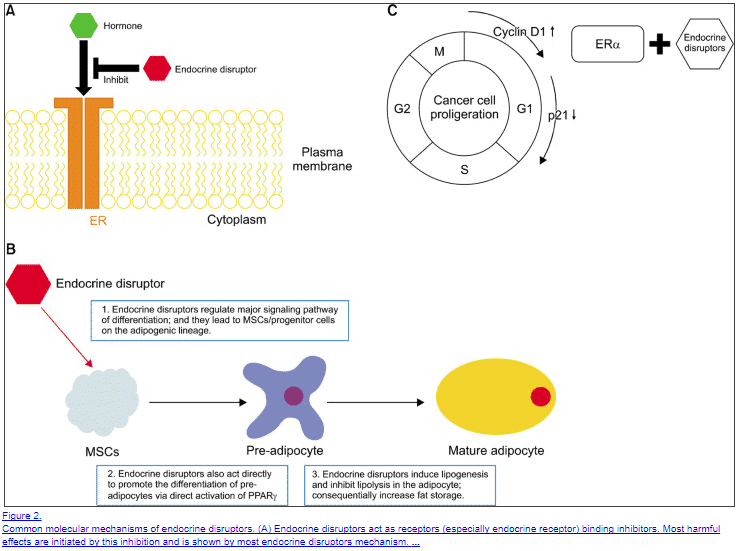
EDCs work by “mimicking” the effects of traditional and regular hormones and by blocking the cellular binding of these native hormones.
The net result is an increase in estrogen a reduction in progesterone (10) and an increase in fat mass.
One big problem with EDCs is that they limit lipogenesis (the burning of fat) which promotes more EDC storage and build-up over time.
So how do you get rid of them?
First and foremost you want to avoid them at all costs.
Secondly, you can improve the elimination of these chemicals by increasing certain enzymes in your liver (those involved in phase II Detoxification pathways (11)).
You can do this by taking certain supplements:
- Milk thistle + MCM + NAC – Take 2 capsules of this supplement daily for 2-3 months.
- Calcium D-glucarate – Take up to 2 grams per day for 10-14 days in a row then take a 1-2 week break.
- Vitamin C (buffered) – At least 2-5 grams daily. If you experience diarrhea simply back down on your dose.
Third(ly?) you need to drink enough water, ensure that you have proper bowel movements, and make sure that have frequent deep sweats.
#8. Cellular Progesterone Resistance (As seen in PCOS & Endometriosis)
This is an emerging concept that has been shown to at least play a role in patients with endometriosis and PCOS.
The idea is that your cells become resistant to the effects of progesterone (12) in the presence of high estrogen levels (estrogen dominance).
This same scenario occurs in leptin resistance, insulin resistance, and thyroid resistance.
As hormone levels in the body increase, your body has a protective mechanism that downregulates receptor activity to certain hormones.
The effect is a temporary reduction in cellular activity but it usually results in abnormal serum labs that don’t match the symptoms of the patient.
Likewise, progesterone resistance creates a scenario in which serum progesterone levels may be “normal” but cellular resistance is occurring which creates the symptoms of low progesterone (which can make diagnosis difficult).
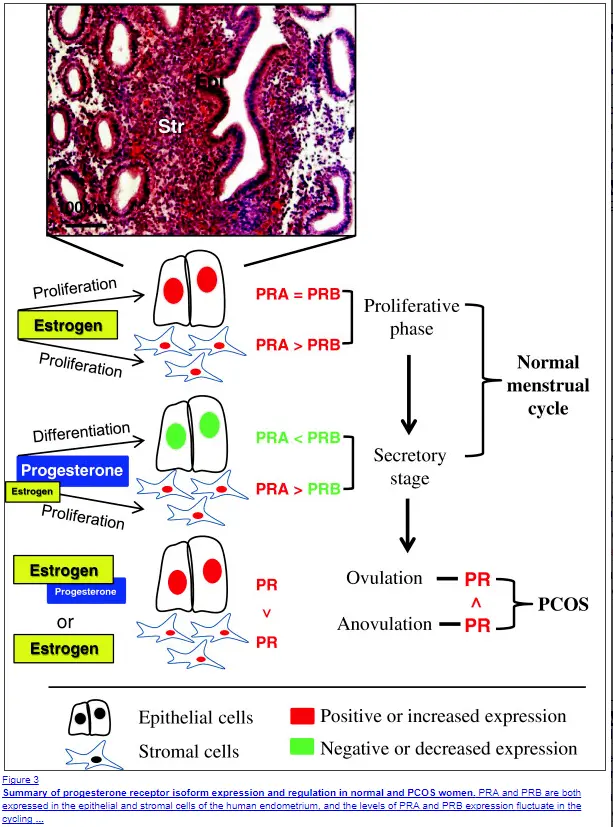
Progesterone resistance tends to occur in patients who ALSO have insulin resistance, higher than normal IGF-1 levels, and high serum estrogen.
It is felt that certain cells may coexpress receptors for insulin, IGF-1, estradiol, and progesterone.
This means that an increase in ANY of these hormones may result in the downregulation of progesterone receptors which leads to progesterone resistance.
Another big problem for women who have progesterone resistance is that taking progesterone will NOT improve the situation and may make your symptoms worse.
This phenomenon may explain why some women who take progesterone, even with low levels, experience negative side effects.
The good news?
This condition can be treated.
Studies have shown that metformin actually helps reverse progesterone resistance (13).
This is good news because it indicates that reversing insulin resistance (which is what metformin does) actually sensitizes your cells to progesterone.
Treatment of progesterone resistance should, therefore, focus on the treatment of existing hormone resistance syndromes and THEN the replacement of progesterone.
Testing your Progesterone
Next up on the list is how to determine if you actually have low progesterone.
Luckily, it’s actually quite easy to diagnose with simple lab tests.
But first, let me show you an example:
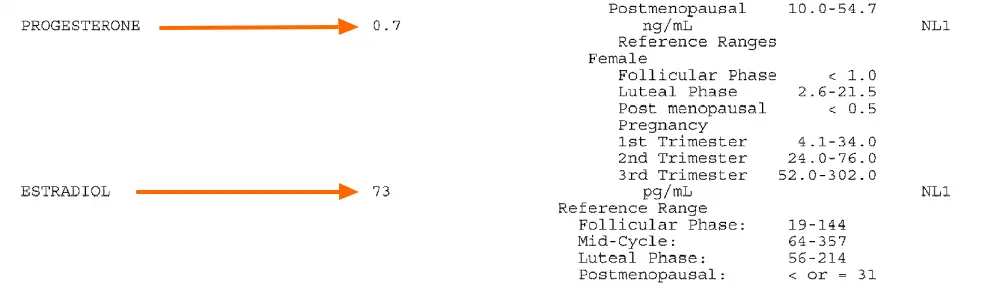
This is a serum lab test of both progesterone and estradiol.
You can see in this example that the serum progesterone level is 0.7 ng/mL while the estradiol level is 73 pg/mL.
This set of labs was drawn on day 20 of this patient’s menstrual cycle, which is when progesterone should be at its peak.
This data suggests that this patient has low progesterone (the reason is unclear with just lab data).
In this set of data, we can see that this patient is indeed experiencing low progesterone and estrogen dominance during this cycle.
You can test yourself by assessing BOTH progesterone and estradiol on days 19-21 of your cycle.
Just remember that serum lab testing won’t necessarily work for each person. Some people may need more extensive testing such as DUTCH urine testing or estrogen metabolite testing.
But it’s relatively easy to start out with a simple serum progesterone/estradiol ratio.
Bio-Identical Progesterone Cream
We’ve discussed several treatment options up until this point but we haven’t really discussed how to correctly use progesterone (and if you should).
If you determine that you have low progesterone (through a combination of serum testing and symptoms) then you may want to consider supplementation of bio-identical progesterone.
You should proceed cautiously when using progesterone, however, especially if you suspect that you may have progesterone resistance.
Why?
Because taking progesterone without addressing the underlying causes of progesterone resistance may worsen your symptoms.
If you decide to proceed with progesterone then I recommend a trial of progesterone cream.
This should be used based on your age and if you are cycling (or not).
You can find relevant information on how to use progesterone safely below:
How to Supplement with Bioidentical progesterone
- If menstruating: Use 20-40mg per day on days 14-28 of your cycle (the latter half of the month)
- If in menopause: you can use 20-40mg per day either 6 days per week (with rest on the 7th) or 26-28 days per month (with 1-3 days off per month)
- Make sure to monitor your symptoms while using and discontinue use if you experience any negative side effects
- Discuss the use of bioidentical hormones with your physician
Back to you
Progesterone is very common among women in the united states – both menstruating and postmenopausal women.
Treating low progesterone starts with the proper evaluation of both your symptoms and serum lab testing.
If your progesterone is low you may find a significant reduction in symptoms such as bloating, weight gain and depression.
Some women may experience worsening of symptoms when supplementing with progesterone which should trigger an evaluation for progesterone resistance.
But now I want to hear from you:
Do you have the symptoms of low progesterone?
Have you used progesterone cream in the past?
Did it work for you? Why or why not?
Leave your comments below!







Ah, yes! I am 46, have every sign of estrogen dominance, and hashimoto’s. Thyroid has been treated with success for 15 years with synthroid/cytomel, but since April I have tried to adjust to NDT with mixed results….feel great but levels have fallen and seem reluctant to bump up. Going to try to bump up one more time or consider adding in a tad of synthetic T4 to the Naturthroid.
Twice over the past 5 years I’ve tried to use bio identical progesterone cream (with some estrogen in there too since I’m still menstruating) and both times I experience severe aggravation, even hostility…exactly the opposite effects I wanted or expected. So I’m definitely one of those for whom progesterone was a bummer instead of a boone.
Your article gives me hope that perhaps I’m not sunk as I do think that progesterone supplementation could really help me *IF* I can get my system to allow it and not resist it.
The insulin resistance piece sounds interesting and I suppose there’s a blood test for that?
Other ideas?
Thanks,
Hope
Hi Hope,
Yes, you can test insulin through a 12 hour fasting insulin blood test. Normal levels should be less than 5.
Hi Westin,
I’m at a bit of a crisis. Here goes..
I’m 26, 27 in Feb.
My partner has just done a sperm test because he just wanted to know, and because the first 2 years we were together we did not get pregnant (we didn’t try to but we also didn’t try not to – i have not been on contraception for at least 4.5 years)
Anyway, we are getting married in 2 months and will be trying for a baby then.
Results of the sperm test were NO sperm, so as part of our referral to the fertility clinic I had to do blood tests etc to check my fertility also.
I had a blood test 5 days before my which came back saying i had a hyper thyroid (i have no symptoms of this), was low TSH and high T4. I also showed a low FSH level.
My second blood test, on day 3 of cycle has come back with low progesterone so it is unlikely that i ovulated.
Honestly, i’m worried sick now.
I am so worried that i’m not going to be able to have a baby. If it is stress that has caused it, i don’t know what to do. My grandma died just before Christmas which devastated me and then my grandad died in May. So yes its been a hard year.
My thyroid was checked in January and it was normal then.
Please give me your thoughts. Kristel.
I have been struggling with weight and hormonal imbalances my whole life. Over the last several years I have switched to a wholesome, paleo diet and I focus on weight lifting and HIIT (though I don’t overdo it like I used to). My hormones are pretty bad: low cortisol thoughout the day, low testosterone, dhea, progesterone, and even estradiol. I’m confused because I’m young (25) and very overweight, and yet both my estradiol and progesterone are low. I see little research addressing estrogen dominance in the context of having low estrogen, especially for young (and overweight) women. I also have some hypothyroidism. I’m currently taking sublingual BHRT of dhea, pregnenalone, and 100mg progesterone (second half of cycle) as well as NDT. While my thyroid numbers have improved, I’m still gaining weight and have no improvement in energy. I wonder if increasing my progesterone and/or switching to a cream would be helpful in my situation.
Hi Brenna,
Based on your brief history it seems that you likely have a bigger problem that isn’t being addressed. I would suspect that altering the way you take progesterone will likely not lead to significant changes in your weight.
Make sure you are not taking your progesterone at the same time as your thyroid meds. That will negate absorption of your thyroid meds. If your “numbers” mean TSH, I would aim for the lower end of the “normal” range.
Alot more Estrogen is stored in our tissues than in our blood. Have your prolactin tested and that will give you a much clearer idea of your estrogen levels. There are some studies on pubmed (search of estrogen concentrations in tissues). When you start to take progesterone it actually pushes some of that estrogen that is stored in tissue into the bloodstream and that’s why symptoms can be bad at first. Just some info to look into.
Thank you for that, Dr. Childs. I forgot to mention that I have some digestive issues, including low pancreatic enzyme production that began when I started menstruating at age 12. Hypothyroidism is also EXTREMELY genetic on my mom’s side. I’ve been addressing my gut health with antimicrobials and probiotics under the guidance of a FM practitioner, but determining what ultimately caused the weight and other hormonal imbalances has been a never ending struggle.
Hi Dr. Childs, I have POI and I have hypothyroidism. Started Estrogen and Medroxyprogesterone cyclically 3 years ago and then Synthyroid in Dec 2016 at 50mg. My hair fell out continuously on my head with very very bad scalp pain. I’ve tried many doctors, no one seems to understand the scalp pain. Fast forward, end of Aug 2017, new doctor says get off Syn and take Naturethroid 1/2 grain which basically took away all energy and then she put me on Prometrium 100mg continuously. A week later, too tired so she said to go 1 grain and I also started bleeding. She told me to up the Prometrium to 200mg and I told her I couldn’t take the insomnia and heart palps but noticed that the 10lbs I put on slid off fast! I’m 5’6 and 120 now so that’s my regular weight before Syn. Anyways, she didn’t listen to my insomnia and heart issue so I left to another practice early last month and put myself on 3/4 grain. Meanwhile, my eyebrows and eyelashes start to fall off alot. The new doc says to use 3/4 Naturethroid and 25 mg of Levoxyl. No help, did it for 10 days and gut said that wasn’t right as nothing was improving. I read one of your pieces that said titration is very very impt! My gut decided to stop that and take 3/4 (which makes me foggy) and add 1/4 grain 4 hours later each day and it seems to work, almost no heart palps. This was Oct 16, 2017 that I did this. I’ve had significant reduction in scalp pain (btw – I’m doing hair prp, just had 3rd tx) but my eyebrows and eyelashes continue to fall (not sure why this wasn’t present while on Synthyroid). I’ve told the doc but she doesn’t know if it will stop or what to say. I feel like I’m paying her but treating myself using your articles, I print them all off and highlight them and read and re-read. I’m terrified to wash my eyes and they hurt and are really sore! I’m devastated so I’m hoping you can help me. I still have to wait for the new thyroid labs, another 2.5 weeks before I can even have it since I changed the dose 10.16.17. The bleeding hasn’t stopped, it’s old and new blood. I do have bad entrometriosis but I’m also POI so I should only bleed if I’m on cyclical therapy. Since I’ve been on Prometrium, it has been a continuous therapy. Yes, I have tested high for inflammation, does having a high EOS absolute result of .5 mean anything? I am also pre-diabetic despite eating pretty well. Sorry this is so long.
Dr. Childs, you mention treating progesterone resistance by addressing insulin resistance. Do the other factors — leptin and thyroid resistances — need to be treated as well?
Also, is there a such thing as low progesterone as a woman’s particular homeostasis. Maybe she simply does not need it or needs levels lower than norm to feel OK.
Dr. Child, I am taking metformin and was able to reduce my A1C to 5.2 thanks to your articles, not sure what my fasting insulin is currently though.
With these changes I still suffer progesterone intolerance. Any other indicators to consider?
I am 45 years Old and am 2 years out from having a total hysterectomy. I take Estradiol 2mg daily. I have Many if not all the symptoms you describe regarding estrogen dominance/low progesterone. Every year (even before my hysterectomy) I have a physical, and my labs always come back within normal limits, with the exception of my fasting blood glucose is on the higher end of normal (~110 most of the time). My CBC recently came back showing I have high RBC (5.7), high hemoglobin (14,7), high hematocrit (46.5), and high ferritin (262). I have 3 nodules on my thyroid that my dr say are benign. My TSH was low (2.77), T4 was normal (1.5), and T3 was low (2.6). I think I’m most concerned about why my RBCs, hemoglobin, hCT, and ferritin are elevated. Can this be caused from my hysterectomy?? And why were they not elevated last year (one year post hysterectomy)?
Hi Dr. Childs,
I recently turned 25 years old and my naturopathic doctor has recommended Progest Avail by Designs for Health as a way to boost my progesterone. My cycles are long and often irregular, so I had labs drawn the day before I got my period. Those results showed progesterone of 1.1 and estradiol of 64. I also have PCOS and hypothyroidism (not Hashimoto’s disease though, as my antibodies are 0) – just low free T3 and free T4). I am incredibly nervous to try this bio-identical progesterone cream, but am desperate for symptom relief (weight gain, water retention, and severe acne). Is this type of cream something you would recommend for someone my age?? I feel like I’ve only ever heard of it use for menopausal women. I am so young, I don’t want to do more harm. Would love your input. Thanks!
Hi Jen,
Usually, there is something in the body that causes low progesterone (it often doesn’t occur on its own), it would be best to try and identify that problem and then address it. Taking supplements (just like medications) may sometimes mask problems without actually treating the underlying cause.
Dear Dr. Childs,
I have been feeling rather desperate (like many of your commenters here). I am 37, and have had a baby recently and am still nursing (baby is 10 months). Several years ago I took an estrogen only birth control pill that made me very sick: palpitations, tachycardia, difficulty breathing at rest, telangiectasias, skin sores/lip sores, feelings of dread and finally figured out it was the pill, and symptoms resolved with stopping pill. About 5 months ago, I began to have similar symptoms but this time with a very high blood pressure as well. I’ve been reading about estrogen dominance and seems to fit. Symptom include palpitations/tachycardia, skin/lip sores, trouble with sleep, fatigue, trouble getting deep breath at rest, feelings of dread. I’ve been evaluated by a cardiologist and internist and gone through intensive testing and been told it is anxiety. I do feel anxious, but feel it is a symptom and not the cause of all this. I am a physician myself and spend a lot of time figuring out what has caused my patients’ illnesses, and feel I haven’t been able to stop looking for mine despite what my doctors have said. Any advice? (I have not had hormone levels tested).
Many thanks.
Hi Leann,
The first place to look would be at basic hormones (thyroid, estrogen/progesterone, and some basic vitamin/nutrient levels like B12/folic acid) as this will give you a starting point. I would also make sure to check iron/ferritin, antibodies for thyroid autoimmunity and antibodies to gluten. I’m not convinced just based on your clinical presentation that this would be caused by estrogen imbalance alone, but I do think that it could be caused by one or more of the following issues listed above.
I’ve seen patients present with similar issues only to find sub-optimal B12 or gluten antibodies which can completely fix the issue. Your symptoms certainly present on the anxiety spectrum but you need to figure out what is exacerbating the anxiety or triggering it from the list above. Hope this helps!
As a side note, this might be the most pleasant interaction I’ve ever had with an intensivist on the subject of hormone imbalance! Haha 🙂
I have tried progesterone cream (25mg dose 2x/day) and have seen a decrease in symptoms of insomnia, fatigue, irritability, and anxiety. My dr. prescribed vaginal estradiol cream, but I have not had + results; abdominal pain, labial skin irritation, and breast tenderness. I am going to stop the vaginal cream and re-start the Progesterone cream. Your thoughts?
Hi,Dr. Childs, I love your website! I am two years post-menopausal (age 58) and have just started using progesterone cream. I am also reading Dr. John Lee’s menopause book. He suggests that even post-menopausal women take a week off all at once, but I have seen others including you say that it’s okay to take just one day off per week. Could you explain why we don’t need to take a string of days off in a row after a certain age? I would rather not because I love the way I feel on progesterone, but want to understand what I’m doing as far as the schedule. Thank you!
Hi Sheree,
If the dosage is small, and you are no longer cycling, then not taking a few days off here and there probably isn’t an issue. I still recommend it to my patients, though, because variability is a normal part of your hormone balance.
I’m 52, have a low thyroid ( which I take NDT for ), endometriosis and high cortisol*, ( which I treat with holy basil* ). I’ve had two periods so far this year, now in Aug, I’ve been taking biogenetical progesterone for 4 months 150mg. With one day off each week. Started off ok ( 1st 2 months ), but now appear to have more oestrogen dominance systems, ie; tender enlarged breasts, weight gain ( fluid retention ). I have read many articles that Dr lee wrote. Should I reduce my dose to see if that helps?
Hi Paula,
You can’t really say for certain that those symptoms are related to the progesterone because you are still having anovulatory cycles (due to perimenopause).
Hi Dr. Child’s,
I tested positive for sibo a couple months ago. I finally decided to take the two week antibiotic treatment with Rifaximin. I have 3 days left of the treatment, and I feel like I’m feeling worse today. I’ve been having excessive gas, bloating, etc. I have noticed an improvement of some symptoms, but after feeling worse today, I’m not sure what to think. I know everyone is different, but I have three days left of the treatment, and I feel frustrated that I’m feeling worse all of a sudden. How long does it take for symptoms to really improve? Am I just experiencing die off? I don’t know, I feel lost about this and I don’t know what to think. I am open to anyone else’s suggestions on here as well.
What are your thoughts about progesterone replacement if you have had a complete hysterectomy? I am replacing estrogen and testosterone. I was told if you didn’t have a uterus you did not need progesterone.
Hi Theresa,
Other cells in your body, including your breast tissues, have progesterone receptors. I’m not sure who is telling women that they don’t need progesterone if they don’t have a uterus but it makes very little sense. The only reason I could see someone suggesting that is because the risk of uterine cancer is diminished but that doesn’t diminish the risk of breast cancer or of the other positive benefits that progesterone provides to other cells and tissues.
I started taking Liothyronine and it reduced my luteal phase from 2 weeks to 1 week. So, I’m taking progesterone troches twice per day during my luteal phase to offset the effects. Why does Liothyronine reduce my progesterone levels? The same thing happened when I took Ashwagandha. It also happened when I took primrose oil and milk thistle. Why?
Hi doctor, 7 years ago that I noticed my period length was becoming shorter and shorter until it went down to 17 days… I went to the gynecologist which diagnosed me with hashimotos thyroiditis, and it’s been 18 months that I am on levothyroxine and also dydrogesterone the second half of the month but still see no improvement regarding the length of my cycle. My TSH was .67 last month… Can you give me some advice on how to improve my progesterone levels? Is Hashimoto the cause even with thyroid hormones in optimal range? I just turned 34. I have a very healthy weight and workout several times a week. Thank you!
Hey Doctor C!
Big fan. Video got me here.
I, myself have had issues & so far still struggling w/hormones.
(already lost 90 lbs/reversed 15 conditions w/diet/supps)
Blood test w/ND = 0 progesterone, really low testosterone, normal Estro, on Nature-throid (doing good there)
Tried the prog cream – no serum change
Tried prescription progesterone – heart rate up (peanut oil?)
Compounded + supps (maca, EOs)- pro & testosterone now 24.
Tried going off prog = testosterone stayed up but prog crashed again.
I am on pellets and taking progestrone pills and last week I forgot to take 1 pill on Wednesday three days later I was staining very light for 2 days is that normal I am 60 years old and perimenopausal.
Hi Donna,
If you are menopausal then that is certainly not normal but if you are perimenopausal then that could happen. Just make sure you understand the difference between those two things because it matters quite a bit in this case!
I thought this was Dr. Gonino’s site. I’m not sure what you would be sending me. There was no cost shown so I have to assume it is free. If not, don’t send me anything. I’ll talk to Dr G when I see him next.
Hi Mary,
I have no idea what you are talking about but you are welcome to read the information I have here 🙂
Hi Dr.Westin ,
Just came from listening to your Birth Control Side effects podcast and I’m not sure where to start ! I am 23 , will be getting married in a couple of months and will try for a baby then. I had regular menstrual cycles up to about 1 year ago to now. Actually I have not been having any periods for the last six months so I finally braved the courage to go see my GYN since I obviously saw my period was not coming I became concerned. I am not pregnant. Never have been on birth control , but had my blood work drawn and going to follow up on the results of that in a few weeks. The doctor put me on a Yasmin birth control alternative to “try and regulate my periods” the plan is to take me off in a few months to see if my period will come back by itself. So far I’m on week 2 of taking this medication and have had several of the symptoms you mention In your podcast. Not sure at this point what else to possibly ask my doctor to take instead of this birth control or what could be causing this irregular period cycle.
Menopaused
I have 2.0 nmol progesteron and
444 pmol estradiol
Am i still estrogen dominant?
i use progesteron 2x 75 mg cream and 1x bi est 0.25 cream
30 lbs gained from 2x 20 mg progesteron
Anny help please
Is it ok to take bio-identical progesterone if you have had breast cancer? My doctor will not prescribe the pills. I have Hashimoto’s disease. I understand progesterone is good for hormone positive BC?
Hi Marilyn,
It’s a very complicated and complex topic. Some people say yes and others say no, it depends on who you talk to and the type of breast cancer that you have.
Hello Dr Childs,
I’m Gaby, I was diagnosed with PCOS 12 years ago and have not been able to get it under control with the countless physicians I’ve seen. I am now 30, and finally found a Dr smart enough to even do proper labs but he didn’t test my progesterone.
I have been having nonovulatory cycles for the past 2 years by evidence of Basal Body temperature and negative LH tests done daily over a 60 day period. My last menses was induced by Provera after a 6 month absence. At exactly the 19th day of my cycle I used bioidentical progesterone to no avail.
My question is how would I even go about testing my progesterone or taking progesterone if I dont have a normal cycle?
** background info**
I am overweight and have managed to lose 30 lbs with new Dr recommendations.
I have high androsterone,
High free, total, and bioavailable testosterone,
normal DHEA and Estradiol levels.
Hi
I have Hashimoto’s , very high antibodies+ T3 and T4 low but borderline ok, which for the last 8 years or so I have managed solely through diet. I am now in menopause and experiencing much worse symptoms and adrenal fatigue, despite a very good diet/lifestyle . I was looking at testing hormones(progesterone DHEA etc) but are you saying that there is no point in supplementing with these if the thyroid is underactive as mine is?
Hi,
I have been having short cycles the last few months (22/23 days). I got off the pill 5 months ago. I gained lots of weight and acne from the pill. I’m getting back to my previous weight now and acne is clearing up. I’m doing low carb and Intermittent fasting. I started taking DIM and wanted to know if it’s good idea to start using the progesterone cream as well to lengthen my cycle.
Thank you!
Mielcah
At about age 15 – 16, my daughter began having what appeared to be migraine/anxiety symptoms that appeared to revolve around her cycle. Because of the cycle association, I took her to my OBGYN who tentatively diagnosed her with PMDD and prescribed her a low dose progestogen and had us do a follow-up with a neurologist. No labs were completed to confirm any hormone or other system levels.
Fast forward 3-4 years, her symptoms of anxiety have progressively gotten worse – we increased meds to cover actual pain from migraine and anxiety meds along with the low-dose progestogen. We have been to the ER and had MRIs and other tests run due to ramp up in symptoms that appear anxiety related, but in reading the Rx Info Sheets on the anxiety med – I find that she needs to be weaned from that med as it precisely describes the physical manifestations of a life threatening condition that my child has demonstrated since beginning the regimen.
All this to say that these symptoms, coupled with the fact that I just had a hysterectomy (total) with symptoms that were blown off for years by my medical professionals (severe and unexpected endometriosis was found when I was “under the knife”). These are the same doctors who are currently treating my daughter – I will be seeking medical advice elsewhere at this point.
I am at a loss as to next steps for my daughter’s initial symptoms. Thankfully I do have connections to the medical field and have privately consulted a medical professional about weaning her safely from the anxiety med – but I am concerned about communicating her true medical issues, how to get the tests she needs without extracurricular labs being completed, or if maybe we should just try holistic remedies first.
FYI
The link to your recommended bio identical progesterone cream is broken. Perhaps you can just indicate which one it is in the text?
Thank you.
Hi Leslie,
Thanks for letting me know! It should be fixed now. You can also find it here: https://amzn.to/3n8LxT4
I’ve read great things about Emerita ProGest. I’d like to try it, but my doctor prescribes 120 mg. BHRT cream for me. Do I really need that much when I read how well others are doing on 20mg ProGest? I’m also on BHRT BiEst 4mg. I’d rather order the OTC Progesterone cream and save money. I’m Post Menopause in great health.
Hi Karen,
When it comes to progesterone, less is more. Your goal should be to use the lowest dose possible while still managing your symptoms. When taking this approach, you’ll find the dose you need is quite small.
I’ve been experiencing hair loss and changes to my hair for almost 7 years now. I have weight gain to abdomen and hips without changes to diet. I’m 43 now. I have low Free T3, and very low Ferritin. From research I believe I have low progesterone symptoms- painful cramping during periods, heavy, clotting and short periods. I have been on Armour thyroid medicine that didn’t have have any effect on me, so I stopped taking it. I take vitamins every day. I am at a loss…. I don’t know which hormone is out of balance and why. I am still a normal weight for my height, but I’m not used to weighing as much as I do. I’m relatively healthy. I’m at a loss
Hello Dr. Childs,
I get menstral migraines and neck pain every month and they are usually debilitating. I am on a gluten, dairy, caffeine free diet due to my hashimoto’s disease and migraine problems. I take ND thyroid 60 mg every morning. I suffer from anxiety and inability to settle down and relax and sleeping is hard. I am 41 and have suffered from this since my kids were born (2013, 2015). I bought some progesterone cream (my doctor has recommended it in the past) and am excited to use it. Any advice?