Did you know that iron deficiency may be one of the reasons your thyroid symptoms remain out of control even while taking thyroid medication?
Iron deficiency is one of the most common nutrient deficiencies seen in hypothyroid patients.
It’s up there with B12 deficiency, magnesium deficiency, and vitamin D deficiency.
Not only is it common, but it is frequently misdiagnosed and/or missed by doctors.
Why? For one very important reason:
Most doctors are trained to look for iron deficiency anemia (1).
They rarely ever miss this diagnosis.
But what they do miss is suboptimal iron levels as measured by ferritin.
When it comes to thyroid function, the measure of your iron stores (and not your serum iron levels) is more important.
Patients who have hypothyroidism deserve special attention and treatment if their iron stores are low because of how important iron is for thyroid hormone function (2).
Today you will learn:
- Why iron is so important for thyroid function.
- How to test both your iron levels and iron storage levels.
- What level of iron is optimal for thyroid function.
- When to supplement with iron and which types of supplemental irons work best.
- How iron impacts thyroid medication absorption and other supplements.
- And much more…
Thyroid Function and Iron Status
Iron is required for proper thyroid function.
Studies are clear on the matter (3).
Not only is iron required for the creation of thyroid hormone (4), but low iron levels are also associated with low levels of free T3 (5).
As a thyroid patient, you are probably well aware that T3 is the single most important and powerful thyroid hormone in your body.
Iron deficiency reduces how much of that hormone your body can produce.
This may explain why some patients still experience the symptoms of hypothyroidism despite taking their thyroid hormone medication.
The association between iron and TSH level is clearly defined in the graph below:

You can see the inverse relationship between transferrin saturation and the TSH.
As your transferrin saturation falls (6), the TSH rises indicating a state of hypothyroidism.
Remember:
A high TSH means low thyroid and a low TSH means high thyroid.
Transferrin saturation is a lab test that tells you how much of the serum iron in your body is bound versus unbound.
A low transferrin saturation indicates low serum iron levels in the body.
When it comes to thyroid hormone production, iron is required due to its effects on heme-dependent thyroid peroxidase.
Heme-dependent is another way to say iron-dependent. In other words, this important enzyme requires iron to function.
In addition, low iron has been shown to impact the effects of iodine supplementation (7).
Meaning the lower your iron levels are the less likely you are to utilize iodine if you are supplementing with it.
This can lead some patients to believe that iodine supplementation is not working for them when, in fact, it may be due to their iron status instead.
The worse part about iron deficiency is that it is so commonly missed.
Most providers will only check iron levels if they find that you have grossly abnormal hemoglobin or red blood cell levels which indicate iron deficiency anemia.
And because iron studies are not routinely checked, many hypothyroid patients are walking around with sub-optimal iron levels that are impairing their thyroid without even realizing it.
Symptoms of Low Iron In Hypothyroidism
So how do you know if you have iron deficiency?
One of the first places to look is at your symptoms.
If present, iron deficiency usually leads to a host of symptoms which we will go over in a second.
Unfortunately, because of the bidirectional relationship between iron deficiency and hypothyroidism, if you experience one you are likely to experience the other.
This complicates the picture because you may experience a combination of both hypothyroid symptoms and iron deficiency symptoms which do have some overlapping features.
As a result, you can’t always trust your symptoms but evaluating your symptoms can help you determine if you need further testing.

Symptoms of iron deficiency in hypothyroid patients include:
- Fatigue
- Weakness
- Pale Skin (especially in the creases of the palms)
- Shortness of Breath
- Dizziness, especially with exertion or exercise
- Cravings for ice (to eat or chew it)
- Cold hands and feet
- Brittle nails and thin/dry Hair
- Headaches
You will notice that many of these symptoms also closely match the symptoms of hypothyroidism.
For instance, both conditions can result in fatigue, weakness, and cold hands and feet.
How do you know if those symptoms are caused by your thyroid or by your iron status?
You won’t know for sure unless you get tested for both (more on that later).
Hashimoto’s Thyroiditis and Iron Deficiency
Do patients with Hashimoto’s also have issues with iron?
The answer to this question is a resounding yes.
While patients with Hashimoto’s thyroiditis are not your garden-variety hypothyroid patients, they still tend to have many of the same issues that hypothyroid patients experience.
The lack of thyroid hormone (or fluctuating thyroid hormone levels as the case may be) is still enough to cause changes to stomach acid (8) levels and alter iron absorption.

Proper iron levels are still required for optimal thyroid function in both hypothyroid and Hashimoto’s patients.
If you have Hashimoto’s make sure that you are also following the information outlined in this post so you can get properly evaluated.
Is your Iron Level Optimal?
When we talk about nutrient status we really need to differentiate between having ‘normal’ levels and having ‘optimal’ levels.
Most physicians are trained to look at reference ranges and base treatment on lab values that fall outside of the normal reference range.
But, unfortunately, the reference range for many nutrients (iron included) spans a wide range.
Take serum iron for instance:
The reference range is from 40-190 micrograms/dL.
Your doctor will most likely only care if you are less than 40 or higher than 190 mcg/dL.
But that leaves so much room in between where you may feel sub-optimal.
The difference between 50 and 150 is huge.
And your doctor may ignore your iron levels if your value is 45, but they may treat you if you are 38.
With this concept in mind, and when I give you my recommended reference ranges, I am always referring to the ‘optimal’ levels of iron in your body.
The optimal levels allow your thyroid to function optimally.
Because most physicians do NOT evaluate your labs with the optimal ranges in mind the chances are very high that you have suboptimal iron levels.
When it comes to evaluating for Iron deficiency I recommend these tests:
(Remember that you can ask your doctor to order these tests at your next visit, he/she shouldn’t have a problem doing this for you)
Iron Lab Tests: Ferritin, Serum Iron, % Saturation, and TIBC
To get your iron status evaluated you need ALL of the following lab tests:
Ferritin – This number represents the total storage of iron in your body.
Serum Iron – This represents circulating iron in your blood.
TIBC (Total Iron Binding Capacity) – This represents your body’s ability to carry iron (It will go up when the iron is low).
Percent Saturation – This is the ratio of serum iron and TIBC.
Your doctor will be used to ordering these labs, but the tricky part is in the interpretation.
I find that patients typically feel better when they fall within these ranges to both reduce symptoms and increase T4 to T3 conversion.
Instead of focusing on the standard reference ranges provided by the lab reporting your results focus on the following ranges.
Optimal iron levels for hypothyroid patients:
Ferritin – Optimal Levels = 40-50 ng/mL.
Serum Iron – Middle of the reference range.
TIBC (Total Iron Binding Capacity) – Middle of the Reference range.
Percent Saturation – 35-38%.
Falling outside of these optimal ranges may indicate that your iron is sub-optimal and may be impacting your thyroid function.
If this is the case then you will want to consider using treatments and/or supplements to bring your iron into the optimal range.
How To Take Iron Supplements Correctly
A word of caution for those thinking about taking an iron supplement:
You never want to take iron unless you know for sure that your level is low.
High levels of iron can be toxic to the body so make sure you check to see if you really need to supplement with iron before doing so.
If you’ve already checked your iron status and know that you need it then these guidelines should be considered:
Take your liquid iron away from food.
Avoid taking other supplements, coffee, or tea when you take your iron supplement (These may limit the absorption of iron).
Take your supplement with vitamin C or a glass of lemon water (both of these help your body absorb iron).
Take your iron with B vitamins – B Vitamins help with the absorption of iron.
Take your iron at least 4 hours away from your thyroid hormone medication (if you are taking any). Iron supplements can bind to thyroid hormone medication and prevent its absorption. If you are taking both then using one in the morning and the other at night works best.
Take your iron at least once per day.
The daily dosing of iron usually works best for those with sub-optimal ferritin but not very low ferritin levels (outside of the normal reference range).
If you find that your ferritin or iron are both below even the normal range then you may need to take your iron supplement several times per day.
Track your Progress by Following Ferritin Levels
When taking iron it is very important that you constantly monitor and track your progress every few weeks to months.
Not tracking may lead to really high levels of iron over time, or you may miss the fact that your body doesn’t tolerate the form of iron you are using.
Iron levels are easy to track.
After 4-6 weeks of taking an iron supplement, you can ask your doctor to recheck your iron panel (list above).
Once you have your results you can determine if the type of iron you are taking is working, if you need to cut back on your dose, or if you need to increase your dose.
Over time you should see your iron studies including serum iron and ferritin increase.
You should also experience a decline in your low iron symptoms and you may even see a decline in your hypothyroid symptoms.
Remember that iron is like Goldilock’s nutrient.
Too little is harmful to the body, but too much can be just as harmful.
You do not want elevated iron stores in your body as this can lead to inflammation and many other conditions (11).
What if your ferritin levels are elevated but you have low serum iron?
This lab pattern can and does happen, especially in patients with Hashimoto’s.
While ferritin is considered a marker of iron storage in the body it is also considered an acute phase reactant (12).
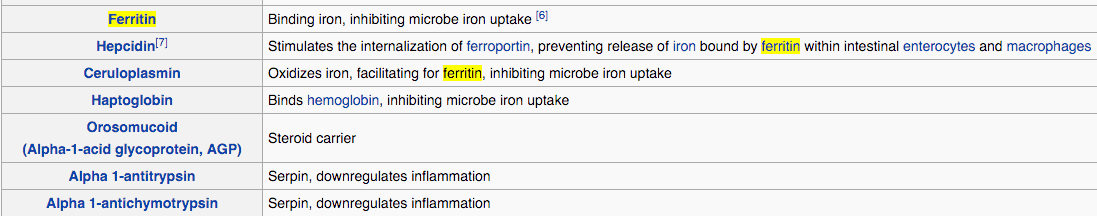
Acute phase reactants are measurements that can be tested in the body that elevate in states of inflammation.
And ferritin is one of these reactants.
This lab pattern of low serum iron with elevated ferritin is common in patients with Hashimoto’s thyroiditis and other inflammatory conditions.
Because Hashimoto’s is primarily a disease of the immune system, it makes sense that many patients with this condition also experience elevated inflammation.
The problem?
This pattern of high ferritin and low serum iron can fool you into thinking that your iron stores are high when in reality they are low.
The body is just in a state of inflammation which is masking the low iron storage.
For this reason, ferritin is a sensitive marker of iron storage when it is low but not when it is high.
If you have this lab pattern then you can often tease out what is really happening by ordering additional tests to check for inflammation.
This will help you determine if you actually need to supplement with iron.
Recap & Final Thoughts
Patients with hypothyroidism and Hashimoto’s frequently experience sub-optimal iron levels.
Iron is critical to thyroid function in the body and these sub-optimal levels can lead to symptoms that may mimic the symptoms of hypothyroidism.
Because of these changes, it is important that you have your iron levels evaluated with optimal ranges in mind.
If you are suffering from hypothyroidism and think you may also have sub-optimal iron levels then you should start by getting a full iron lab test panel.
Replacing low iron may help improve thyroid function by increasing T4 to T3 conversion and helping your thyroid medication do its job.
And while you are at getting your iron levels checked don’t forget to check for other nutrient deficiencies such as vitamin B12, vitamin D, and magnesium.
These are also very common nutrient deficiencies found in hypothyroid patients.
FAQ about Iron and Hypothyroidism
Can an iron deficiency cause hair loss?
Yes, iron is required for proper hair growth and may be one of the main causes of hair loss in patients with hypothyroidism and Hashimoto’s thyroiditis.
Unfortunately, low thyroid hormone itself can also cause hair loss or changes to your hair which can make identifying the true cause of hair loss difficult.
Many patients with hypothyroidism who also have hair issues (hair loss, damaged hair, etc.) have a combination of both iron deficiency and low thyroid hormone.
Replacing iron levels and replacing thyroid hormone in the body are both required for optimal hair growth.
You can read more about how to address hair loss and regrow your hair if you have hypothyroidism in this article.
Will iron deficiency make weight loss more difficult?
The answer is maybe.
Why?
This largely has to do with the interaction between iron and thyroid hormone.
When iron is low your thyroid function will also be blunted.
Low iron decreases thyroid function which may lead to a decreased metabolism which may lead to weight gain.
You can draw a line between iron deficiency and weight gain but it’s not as clean as you might think.
If weight loss is your goal you will want to take a multifaceted approach that addresses nutrient deficiencies, hormone imbalance, thyroid function, inflammation, diet, stress reduction, sleep, and so on.
So while iron is technically included in this list it’s not the most important part.
What is ferritin?
Ferritin is a marker of iron stored in the body.
It is also a marker of inflammation and is often elevated in inflammatory states.
At low levels, it is very sensitive to iron deficiency, but at higher levels, the value becomes less predictive of iron status and more predictive of inflammatory states.
Is ferritin required for hair growth?
Yes, a ferritin level of at least 30 ng/mL is required for optimal hair growth (13).
Studies have shown that levels less than 30 ng/mL may result in hair loss.
Low ferritin, along with low thyroid function, is probably the most important factor for hair growth in thyroid patients.
How long will it take for my iron/ferritin to increase?
As long as you are absorbing the iron supplements that you are taking then you should see an improvement in both measures within 2-3 months.
Ideally, you will want to retest your ferritin and iron studies after 8 weeks of daily iron use.
You may not see a large bump in either at that time, but you should see a slow and steady upward trend (even if minor).
If you do not see any positive change then you may need to evaluate the type of iron you are taking.
For instance:
Are you taking pills or are you taking liquid? What type of iron are you taking? How much are you taking? Is your intestinal tract allowing for absorption?
Answering these questions may help you make changes to your regimen.
What if iron supplements don’t work?
For various reasons, you may be someone who doesn’t respond to oral iron supplements.
If you fall into this category then you may need what is called an iron infusion.
This is a small procedure in which iron is directly infused into your bloodstream.
It is very effective at increasing iron stores in your body but it is typically only used for extreme cases.
This procedure is usually reserved for those suffering from acute iron deficiency, those who are having trouble with constant bleeding, or those who have repeatedly failed oral iron supplements.
This procedure does carry some risks (14) with it so it is typically performed in a hospital-like setting.
If you find that you are not responding to iron supplements, or if you fit any of the categories listed above, you may want to speak to your doctor about an iron infusion.
Now I want to hear from you:
Have you been suffering from iron deficiency as well as hypothyroidism?
What have you done to increase your ferritin levels?
What didn’t work for you?
Leave your comments below!
Scientific References
#1. https://www.ncbi.nlm.nih.gov/books/NBK448065/
#2. https://pubmed.ncbi.nlm.nih.gov/28202844/
#3. https://www.ncbi.nlm.nih.gov/pubmed/12487769
#4. https://www.ncbi.nlm.nih.gov/pubmed/12487769
#5. https://www.ncbi.nlm.nih.gov/pubmed/16500878
#6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4729155/
#7. https://www.ncbi.nlm.nih.gov/pubmed/12487769
#8. https://pubmed.ncbi.nlm.nih.gov/12754530/
#9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6185413/
#10. https://www.ncbi.nlm.nih.gov/pubmed/2507689
#11. http://www.irondisorders.org/iron-overload
#12. https://www.ncbi.nlm.nih.gov/books/NBK519570/
#13. https://www.ncbi.nlm.nih.gov/pubmed/23428658
#14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4518169/




I like the idea of liquid iron, however I have a MTHFR gene mutation and cannot take Folic Acid and B12 in the forms listed on the package label. Any other suggestions?
I have been diagnosed anemic, low iron deficiency. It’s been going on over 1 year. I was on iron pills first year 4 months and had no results. I had bowel obstruction jan 2019. Still no result
I was sent to oncologist. Had iron infusion for months. Then doctor ran test also, I still had a bleed. Hemoglobin went down to 6 and iron level 10. My doctor send me to another doctor. I had pilcam test. It got stuck and ended have another surgery. Bowel resection took 6 inches. 6 weeks after surgery, had 6 more iron treatments. Now my iron level is up now 40. Hemoglobin Is 11.2. Some of other levels are low. I have not been tested for Thyroid level.
My doctor tell me the section of colon cut out is the part that supplies vitamins B12 and iron
So I did get one B12 shot so far. I don’t go back to check iron and blood levels for 6 weeks
My friend came across these pills. So that’s when we both ordered a bottle.
To help with hair loss, breaking nails, dry skin, and dark spots on my face. I have gained weight and after surgery. If there is suggestions to lose weight on stomach and help hair thanks
Hi Kathy,
You would need to know the likely cause of the weight gain in order for me to give some recommendations. For instance, is it related to hormone imbalance, diet, exercise, or some other cause?
In regards to hair regrowth, please see this article! https://www.restartmed.com/treatments-for-thyroid-hair-loss/
The hair treatments listed there work for people with or without thyroid problems.
Gaia just has iron, no extra stuff. Did you find anything that worked?
Good evening,
Thank you for your blog which I found very interesting and frustrating. The contents of the article are not what frustrates me it’s where do I fit. I was born with a missing piece to the puzzle, my thyroid. I’m 50 years old but it was not diagnosed until I was 8. Every emotion you could imagine has been felt in the past 4 months since I found out that the chances are I have never been properly treated. That alone is a long story how I found out.
My question is, if I was born without a thyroid where do I fit in as far as treatment, diet. otc meds and every other place related to thyroid?
Please accept my apology for asking you but my doctor really doesn’t seem to have any interest in answering any questions. If I hadn’t found Pinterest the next 30 years could have been similar to the first 50, not good.
Thank you
Kelley-The Freak of Nature
Hey Kelley,
Almost everything on this blog still pertains to you, whether you have a thyroid or not. In order for thyroid hormone to be effective it must be converted from T4 to T3. And this is important because most doctors still only prescribe T4 medications (which means your body still has to activate it).
Looks like the last post here was 6 years ago- but I found this info helpful. My question is since I have had my thyroid removed, which levels are controlled by synthroid? And is low ferritin and saturation iron numbers suggesting something should be adjusted related to thyroid meds? I feel great. But at times I have idiopathic angioedema (Not urticaria) and am looking for the connections. It’s complicated.
Hi Barb,
If your thyroid is removed then Synthroid is controlling primarily your TSH and free T4 but will have an impact on T3, reverse T3, and total T3 as well. Your iron lab tests wouldn’t really be a good way to assess if you need to adjust your thyroid medication dose. That should be based on your thyroid lab tests. You can find a list of all 10 thyroid lab tests here: https://www.restartmed.com/thyroid-tests/
Dr. Childs,
Thank you for this article! I am searching the internet tonight for anything I can find on optimal serum ferritin levels at the request of my new chiropractic doctor. The first I heard of serum ferritin was when I was tested at a functional medicine clinic in November 2014 (at this point, I was 7 years into my journey of trying to figure out what was wrong with me. I was experiencing fatigue, weakness, brain fog, low libido, upper back & neck pain, heart palpitations, shortness of breath, brittle nails, RLS, etc etc). At that time, my ferritin was at 6.5. Unfortunately, at the time, I could not follow through with the functional medicine doctor due to financial reasons. I did follow up with a regular DO through one of our local mainstream medicine clinics. By the time I met with her in Dec ’14, my ferritin was at 5. My hemoglobin was at 11.8, so the DO was not very concerned. She told me to take OTC iron. I did that for 3 months, plus I bought organic beef liver and swallowed about an ounce of it, raw, every morning. By April 2015, my ferritin had only gone up to 13. I had a hysterectomy in May 2015 (due to complications with the Essure contraceptive device). In July 2015, my ferritin was back down to 7. At my insistence, my GP sent me to a hematologist. Because all my other iron indicators were “normal”, he wasn’t too concerned, but he agreed to give me Rx iron. I took 200mg 2x/day for 2 months. By September 2015, my ferritin was at 64, and I was feeling better. Many of my symptoms seemed to have resolved. However, by mid-December, I was again feeling fatigued, my pain was back, etc. I had labs done in February and my ferritin had dropped to 33. The hematologist I had previously seen was not concerned, so I asked to see another one. In the month I had to wait for that appointment, my ferritin dropped another 5 points to 28 (my level as of 3-18-16). He, too, was not concerned. In fact, he told me my ferritin was normal and could NOT be causing my fatigue. So much for mainstream medicine. In the meantime, I had an acute episode with my upper back which forced me to find a chiropractor. I also decided to go to a local women’s specialty/functional medicine clinic. The chiropractor I have found is very interested in helping me determine what is causing my ferritin to keep dropping (obviously, with having a hysterectomy, it’s not because I’m menstruating). The women’s clinic is testing my thyroid. In the clinic, I did a symptoms checklist and scored 30 (high score=11), which then prompted them to have me do the Thyroflex test. I scored 217 on the Thyroflex, indicating hypothyroidism. We are now awaiting blood test results. Perhaps it’s possible my low ferritin is related to a sluggish thyroid.
It’s rare that I post comments on blog sites, and I’m not sure what has prompted me to tell you my story, other than I am grateful that there are doctors such as yourself who are working to help others figure out their health issues when mainstream medicine fails them, as it has me.
Thank you,
Anne
Hey Anne,
Thanks for sharing your story! Your iron issues are most likely related to either poor thyroid function or a gut related issue or a combination of both. The sad part is that both are a relatively easy fix, you just need to be properly evaluated! Just make sure whoever you are seeing understands how to interpret your thyroid tests, and also make sure to check your serum b12 levels, homocysteine and MCV (these are indicators of low vitamin B12). I’m glad you are on the right track!
Thanks for your very informative info! I have not yet been diagnosed with hashimotos (but have had the test, just not the dr. appt. yet), but my ferritin is 20. I was recommended to go with Pure Optiferretin C pills – 1 pill with with meals, 2x day. My D and B12 are good, but I’m exhausted all the time. I started the ferretin a month ago and have not noticed any change. Do you know how long it should take? I have for 6 months or so supplemented with selenium. I’m on armour thyroid for 3 years now, along with other bioidenticals. Thanks for your input!
Hey Lynne,
It can take months to increase ferritin and iron stores in the body. You also need to consider that you may not be absorbing it 100% due to a combination of gut issues and/or no concurrent use of vitamin C, or that your thyroid dose is still too low.
Hey there, just a quick question, so I have low iron… because I have thalassemia minor, I’ve always been told not to take iron supplements, my mother has hemachromatosis (spelling?) it’s hereditary so I’m not sure if I have it too…. I’ve been struggling lately, feeling like my thyroid med levothyrocine, is just a placebo,cause I can’t get out of my way, and trying to get pregnant has been difficult, my memory and focus is so bad.. your articles have been so informative, I was curious if you’ve come across any patients with thalassemia minor,and what I should ask my doctor when I see him in a couple weeks, thank you so much I’ve saved this link and another.
Hey Gina,
I wouldn’t take iron if you have thalassemia and a history of hemachromatosis, this makes your situation a little more complex than normal. Your levothyroxine may not be effective because you have low circulating serum levels of iron, but that doesn’t mean you aren’t prone to storing iron in organs and other tissues.
In addition your thyroid medication may not effective for a variety of other reasons though as well and that’s why you need further evaluation into your symptoms with lab testing. Getting on the right treatment will be difficult in the conventional medicine model, but you can still ask questions and stay informed!
Hi Dr. Childs—
I am a hypothyroid patient who can’t tolerate the amount of T3 that I need because of low ferritin (around 40). However, my serum iron is 110ish, on average, and when I try to increase my iron and vitamin C intake (I do both through whole foods) my ferritin might climb to 70 or 80 but my serum iron will skyrocket to above 200! I do not have anemia or hemochromatosis (tested negative), although I do have pyroluria and am heterozygous for MTHFR C677T.
This one problem is preventing me from optimizing my medication, since my salivary cortisol levels are great except for the morning value (which is a bit low due to low FT3, I suspect). I have already gotten my Hashimoto’s into remission through diet and lifestyle, but have spent a year being quite under-treated (although no one thinks that I am) while trying to figure out why my body is not storing iron properly. Because of this iron imbalance, if I try to increase my dose of T3 I might feel okay for a little while but then inevitably get anxious, heart palpitations, and so forth, even though my thyroid numbers are still within the normal range. For reference, my TSH is currently above 3 (ugh), FT3 is quite low at 2.0 (sigh), and FT4 is 1.2. I am on some T4 and a low amount of Cytomel (5 mcg), and I am stuck. I haven’t switched to NDT because of this issue.
Have you ever had anyone with this problem of ferritin/serum iron balance, and what did you do? People on STTM suggest treating MTHFR (which I am, with B12 and folate) and zinc/copper imbalance (my serum levels of both are great). So I don’t know what else to do and it’s really frustrating, since I am a young person in my early twenties who is unable to work due to my condition, and relatives “don’t believe” in functional medicine and think that normal MDs will help me or that something else is wrong with me. So I research constantly and have few resources, but have yet to find how to alter this balance.
Also, in one recent post you mentioned someone with the rare condition, idiopathic thrombocytopenic purpura. I have lowish platelets, while still in the bottom quarter of the normal range. Do you think this condition is something I should look into, or that a general inquiry with a hematologist would be beneficial?
Thanks for your time; I so appreciate it. If you have any ideas of where else I can look for answers, I will. Best regards!
Hey Siri,
I wouldn’t focus on your lab values as an indicator of what you need. While it is true that most people do need and do well on higher doses of T3 it isn’t true for everyone. I have a handful of patients who are super converters of T4 and do great on T4 only medications and actually get worse on T3. In addition, you might want to try compounding slow release T3 (bound to methycellulose will slow down the absorption) which may reduce the symptoms you get with the additional T3.
I have seen and treated similar patients, you just need some trial and error and you need to make sure something big isn’t being missed. Remember too that ferritin is an inflammatory marker in addition to an indicator of stored iron levels.
Hello, I was diagnosed with hypothyroidism in 1992, right before I was going in for an Endolymphatic shunt surgery due to an autoimmune disease- Menieres. It wasn’t until 2013 I was I received the diagnosed of with the autoimmune thyroid disease- Hashimoto. I have been fighting with many doctors on my treatment, many not willing to lookout side textbook TSH levels and diagnose and treat by symptoms. I finally convinced my Endo to prescribe Armour, up until a three months ago I was on 90mg daily, I was on that dosage for 1 year. In Oct 2015, finally started seeing some improvements in my symptoms: hair stopped falling out, even saw some hair growth, nails were growing to the point where for the first time in 15 years bought nail polish as they grew past my finger tips, I actually so a fat loss, not muscle loss of 12 lbs. I carry most weight in belly area. Then in April 2016, my endo changed my dosage due to the TSH level results. I immediately started losing clumps of hair, gained weight, nails all broken. Basically I crashed.
July 2015, TSH- .633 (.450-4.50), Free T3. -3.0. (2.0 – 4.4)
Free T4. -92. (.82- 1.77). Ferritin -147. (15- 150 )Vitamin B12- 741. (211-946)
Vitamin D – 38.0. (30.0- 100 )Reverse T3 – 9.0. (9.2- 24.1)
April 2016- Based on the below results Dr changed my dosage. I told her that I was feeling so much better on the current dosage. She told me if I was feeling any symptoms that she would reevaluate.
TSH- .117 (.450-4.50), Free T3. -3.2 (2.0 – 4.4)
Free T4. -1.12 (.82- 1.77). Ferritin -218 (15- 150 )Vitamin B12- 1000(211-946)
Vitamin D – 44.8 (30.0- 100 ) Reverse T3 – 9.5 (9.2- 24.1)
Iron Bind Cap TIBC- 309 (range 250-450),
UIBC 234 (131-425 ) Iron, Serum. 75 (27-159),
Iron Saturation 24. (15-55)
I was tested for Cushings- negative, hepatitis- negative.
Dr has not once addressed my high ferritin levels, I am concerned with this off the chart results, does this require supplementing? I know it’s a inflammatory marker, Is this indication that I have another autoimmune disease? What should I additional testing should I ask for? I am in a sick body and no one can hear or wants to listen to its internal screaming for help.
Hey Kat,
Outside of malignancy or hemochromatosis the main reason for elevated ferritin is due to inflammation as an acute phase reactant. Conventional doctors don’t have a solution for it, so for the most part it will be ignored.
thanks for the reply. Another abnormality that I have found on my blood work since 2009, is an Elevated Glucose Serum. In 2009 it was 110 (65-99), 2011 it was 110, 2014 it was 117, in March 2015 it went to 122, in Dec 2015 it dropped to 115 but still high. In April 2016 my A1c was at 6.2 (4.8-5.6). Since people with one form of autoimmune disorder have an increased chance of developing other autoimmune disorders, I have three that I am aware of – Hashimoto, Meniere’s and Raynard., why wouldn’t any Dr be concerned that I haven’t developed diabetes and treat me. I am sure I have insulin resistance and the that high levels of insulin is combination to thyroid disorder is why it is impossible to lose weight.
In a broad scope shouldn’t my glucose history have been a sign? I don’t want to of course find anything new wrong with me, but I also don’t want to ignore it just because my Drs have if it really something to pursue.
I have been dieting in a yo-yo fashion. I am what i would concern 90% Paleo for the past two years, only eating quinoa and rice 2-3 times a month.
Yes, you definitely have insulin resistance as evidenced by your Hgb A1c. If you were to check your serum insulin I’m sure it would be > 15. Most Doctors will ignore your Hgb A1c until you hit 6.5, at which point you will be diagnosed with diabetes type II and likely started on medication.
That’s why it’s better to go outside of the insurance model to find better care (it just costs more).
Greetings from Canada!
I have Hashimoto’s, high cortisol, low TSH (around 0.5), less than mid range FT4 and bottom of the reference range of FT3. I tried 25mcg T4 + 5mcg sustained release T3 in mid-June and only lasted 3 days because I felt so much worse on it. I discontinued the meds 6 weeks ago and I still suffer from a myriad of more miserable symptoms than before meds, including depression, easy bruising and skin rashes.
I had my iron levels checked today:
Serum Iron: 14.9 (ref: 10.6-33.8 umol/L)
UIBC: 48 (ref: 24-61 umol/L) – for some reason, the labs here do UIBC instead of TIBC – are they much different?
Iron saturation: 0.24 (ref: 0.13-0.50)
Ferritin: 113 (ref: 15-247 ug/L)
I guess my ferritin is elevated (ie. >70-80) because of the inflammation from Hashi’s or something else???
I’m already on an anti-inflammatory diet (for the past 2.5 years), which most closely resembles the autoimmune paleo diet.
CRP is below the detection limit of the assay. I don’t think I’ve ever had an ESR done.
Is there a way to increase my serum iron without my ferritin going sky high?
Any other suggestions would be most appreciated!
Thanks!
I’m flying on instruments right now.
Hypothyroid. Low antibodies. Low TSH even with fT4 at the low end of normal. High revT3. On 1.5 grains NT.
Elevated homocysteine.
Iron 125. Ferritin good. TIBC less than they can measure. Saturation > 75%.
MCHC a touch low. MCV normal.
Cortisol metabolites low.
For now, just trying to figure out whether or not to avoid iron.
Hey Lianne,
Are you symptomatic? I wouldn’t worry about the iron unless you are symptomatic, there is no “magic” number for iron because it depends on how YOU utilize the iron in thyroid function.
My body takes anything and everything as an excuse for chronic inflammation. A mostly dry cough with hoarseness. Sinus headaches. Ears plugged. Digestion touchy. Skin lesions. Lymph glands swollen. Arthritis. Tendonitis. Sore neck muscles. Etc.
It honestly doesn’t sound like iron is really going to make much of a difference in those symptoms.
Hi,
I have hashimoto and my ferritin is low today is in 6 ng/ml and the TSH is 8.59 mcintUunits/ml. I cannot take the iron supplements since it cause me stomach ache and irritation of my intestine, the hemorroids get activated and can bleed. I really do not know what to do. Please let me know my possibilities. What is the best for me to do? I had never tried the liquid formulas should I try them?
Hey Rosa,
Yes you can try the liquid iron in this post which is usually much better tolerated than pill forms of iron and usually doesn’t cause constipation or other GI issues.
Hello Dr. Childs,
I stumbled across your page and I am hoping you can point me in the right direction. I am 43 years old, morbidly obese and have many symptoms so much so that I don’t know where to start.
I have hypothyroidism. I have been on Armor Thyroid since for 10 months now and started at 15mg on 11/12/2015. In 11/2015, my TSH was 5.33, Free T3 was 2.6 and Free T4 was 1.3 – Also, my MCV was 70.1 and my RDW was 17.1
At that time, My GP put me on A.T. 15mg for my Thyroid (I cannot take the Levothyroxine or Synthroid – bad heart palpitations) and she told me I had low iron, start eating more spinach and beef. We did a re-check 5 months later in April 2016 and my TSH had dropped to 4.44, T3 was 3.2 and T4 was 1.4 and lastly my Ferritin was 11. Those are the only tests she requested. GP had also bumped up my A.T. to 30mg from the 15mg.
We just did new tests in July 2016 and my iron is concerning me. My Ferritin is now 6 (was 11 three months prior). More tests ordered for Total Iron (22), Iron Binding Capacity 434, Iron Saturation was 5, my Hemoglobin A1C was 5.8 and then for my Thyroid, my TSH was 3.29, T3 was 2.7 and T4 was 1.4
I was experiencing some irregularity with my menstrual cycle so I backed down to the 15mg of the Armor Thyroid myself and informed my GP after the fact. It seemed to get my cycles back in order. I also began an iron supplement (Phyto Multi) with Iron. The doctors office sold it so it was recommended to me and I started taking it. I’ve read your article and I don’t know if it will truly help me and I think I’m getting some problems with it (darker colored stool and almost neon colored bright yellow urine) the last few days. My GP has no idea but I wonder if it’s the iron supplement or the Armor Thyroid.
My question is: Could the Armor Thyroid be causing my iron levels to have dropped significantly? Nothing else changed in my medication regime with the exception of starting A.T. in 11/2015 and increasing the A.T. and then my iron drops. I’m scared. I don’t know what to do, please help. Sincerely, Jill
Hey Jill,
Your Doctor should be looking for a source of your iron deficiency, dropping iron like that means you are either not absorbing or losing iron (usually through bleeding).
Thank you for your reply. My GP also said that about excessive bleeding. My menstrual cycles have changed in the last year and much heavier than they used to be. She thinks that may be the case but can’t be sure.
Does my iron binding capacity have anything to do with seeing if I cannot absorb iron?
What specific labs should she order to see if I am not able to absorb iron? Additionally, what can be done if my labs come back that my body can’t absorb iron like it should?
Thank you, Jill
Hey Jill,
Iron evaluation is very basic and every physician should have an understanding of what tests are required for evaluation – I can’t provide you with this information online because you aren’t my patient but I would go back to that provider for more help (or seek out a new one).
Hi Dr I have hypothyroid and my hemoglobin is 6.5,
Even my platelet counts are high,its been 11 years since I have been detected hypothyroid,
My r.b.c or hemoglobin have always fluctuated…
I always work hard to bring it to good number still it keeps decreasing,
My doc has now asked me to get ferritin iron vitB12 vitD bilirubin to get tested..my tsh is 17.5,
I am really depressed by all this ,
Isn’t there a solution to hypothyroidism,
It can’t be cured?
Hi Pooja,
It can be improved upon in many cases, you can read more about how to naturally improve thyroid function here: https://www.restartmed.com/thyroid-support/
I’m a teenager with hypothyroid, when they discovered my anemia my ferritin was as low as three, I was taking liquid iron for a couple months but it was aggravating my stomach ulcers I have from taking too much ibuprofen for my chronic knee pain so I had to stop with the iron by the time my ferritin got back up to eight, which is obviously still very low. My aunt got an iron IV when she was almost equally anemic, but when I asked my doctor about that she said my iron is “not that low” and won’t put me on a thyroid hormone because we have “bigger concerns” and won’t give me anything for my knee pain because she “doesn’t think it’s that bad”, though all three of these things I’m not getting treatment for are debilitating. I don’t know how to proceed.
Hey Sarah,
It sounds like it might be time to look for another physician who is more willing to work with you or at least seek a second opinion.
Hello!
I’m a twenty something with subclinical hypothyroidism (9.5 was my highest TSH). I have extreme fatigue and I can’t lose weight, dry HSN etc. Months ago I had a CBC the revealed a slightly low MCH and MCHC and a slightly elevated platelet count. My doctor said that was fine, but with my own research I have found this may have to do with an iron deficiency. Unfortunately my dr. won’t order the test. On levo, my TSH has gone down to a 3.5 but I feel terrible, if not worse!
She says it’s the stress of senior year of college, and I partly believe it, but I also know that my friends do not feel this way! The lab will do Iron Serum and Ferritin labs for me without the Dr, but without the other two parts is it pointless? I have 8 of the 9 Iron deficiency symptoms and all of the thyroid symptoms listed.
Thank you so much for any help!
Hey Kate,
You would be far better off finding a new physician more willing to work with you than checking your labs on your own. Having said that you can still find value in checking your ferritin + serum iron.
Hi Dr. Childs,
Thanks so much for the informative website, I am actually printing out several of your articles to share with my practitioners. Ultimately I’m curious whether you think my practitioners could be a bit less conservative, or if I should consider seeking new.
I’m dealing with both low ferritin stores and low T3 and am not getting the support I’d like from my PC and although a bit better, not what I’d like to see from my endocrinologist.
Over a 6 month period, my T3 scores have dropped more than 100ng/dL despite increasing my Synthroid from 137 to 150mcg, and adding first 5mcg and now 10mcg cytomel. Today my endo called to say my thyroid labs look perfect (TSH .7, FT4 1.1, T3 183). The nurse said that T3 is the least accurate value and can fluctuate – but this does not set well with me considering my values have been consistently dropping and have now gone far below reference ranges. I left a message in return and am hoping she’ll work with me (she has in the past when I don’t accept sub-par values).
Adding to the ongoing thyroid challenges, I have been dealing with low ferritin (but with normal to high red blood counts) for 8-10 months. It got so bad i had severe heart palpitations (4K PVC’s in 24 hour holter) and significant telogen effluvium. Supplementing with 65mg ferrous sulfate, eating an iron rich diet (guided by dietician) and adding 240mg ascorbic acid when taking the iron, has only raised ferritin levels to low 40s in 6 months of effort. My endo sent me to my PC, saying she wasn’t aware of the impact of iron on thyroid and she doesn’t treat iron issues. My PC did not respond to questions about how to dose iron supplements, or whether there are better (easier absorbed) types of supplement or prescriptions. She has instead suggested I should go see a hematologist.
I think there’s still room to work with the endo, but at this point I’m fairly sure the PC needs refreshed. Is it reasonable that I should go see a hematologist? Is my endo being too conservative or would I be better to find a more willing endo as well?
Thanks for your time and attention,
G
Hey Gretchen,
Generally if you have to push for more tests/treatment/etc. you will most likely not end up feeling significantly better because you are in the driver seat. It’s best to spend your resources finding someone who is willing to help guide you vs being dragged along.
You might also find this article helpful regarding lab testing: https://www.restartmed.com/thyroid-test/
Thanks so much for your prompt response Dr. Childs, and for the reference to the testing article, it is much more detailed than similar articles I’ve read to date. I very much appreciate how detailed your posts are; teaching me more about my condition helps me drive conversation with practitioners and how to better care for myself. I’m willing to do as much hard work as it takes to be at optimal health and look forward to finding doctors willing to do the same for their patients.
Indeed it is frustrating feeling like I have to ‘drive’ things forward, and yes I’ve felt sub-optimal for over a year now and have seen little in the way of progress without my pushing. Not sure what protocol these doctors are dealing with, but I don’t understand how they have a patient with active, impactful illness, and they only want to see me in the office on a 6 month schedule for PC and 4 month with the endo. I’ve been able to push the endo for 30 and 60 day visits, but dealing with T3 with its shorter half life than T4, and continuously falling T3 – 90 days is not cutting it.
To credit my endo, since becomming her patient last fall, she has tested every one of the items in the article you reference, and then some; insulin, glucose, cortisol, ACTH, aldosterone, sex hormones and more – the only test I had to push for (and just once) was RT3. However, I went from feeling critically ill to unwell under her 6 months of care. Unwell is not how I intend to live.
Thanks again for your response and knowledge sharing. I look forward to learning more by catching up on and following your blog posts!
G
This article was really informative. I do have a couple questions. I am in my early 20’s and pretty much always had irregular cycles (typically long) and low energy. A year ago, I was diagnosed with hypothyroidism and started on Synthroid. About 5 weeks ago, I switched to WP Thyroid after not seeing any improvement in my cycles (energy did improve somewhat) and wanting to regulate things before trying to get pregnant. I have never had super high TSH- my highest was 5.16 and lowest 2.36 in the past year. After switching to NDT, my last TSH was 3.55, so my doctor upped my dose to 3/4 grain. I honestly felt great on the 1/2 grain, but now on 3/4 have been feeling very fatigued, so I decided to get my iron tested. My results are Ferritin- 25, Total Serum- 92, TIBC- 344 and % sat- 27. Do you think from these numbers I would benefit from a liquid iron supplement? My ferritin is clearly low, but my TIBC is pretty high, so I’m not sure what that means. Could that be a sign of something else, like heavy metals or the MTHFR mutation?
Thanks for any insight!
Meri,
I can’t speak to all of your questions but can speak to the TIBC. It will be HIGH in iron deficiency. TIBC is a measure of the carrier proteins in the blood that are available to bind iron. When iron is low, your body increases its production of carrier proteins to try to “find” what little iron you have, so to speak. Low ferritin and high TIBC usually go together and both point in the direction of an iron deficiency so it’s probably worth trying an iron supplement to see if your fatigue (and lab values) improve.
Hi Dr,
I would like your advice on how to select a Dr who would be able to help me with the issues you’ve written about. I successfully managed to get my Ferritin levels into the 40’s after 4 years of on off iron supplementation, I finally found one that seemed to work and took it continually for a year to get that result. I was then advised to stop taking it, by a Dr, to see if my levels remained the same, unfortunately they dropped to the 20’s within 4 months. I’ve had thyroid checks over the four years, which haven’t produced any results leading to a diagnosis.
I’ve heard that some Drs treat sub clinical thyroid issues with success.
I suppose, I would like to know which kind of Dr should I choose or what experience should a Dr have to be able to put the pieces of the puzzle together, so I can finally know what’s responsible for the issues I’m having and what to do about it?
This is amazing! I have been on levo for low thyroid for about 8 years, but in January I started gaining about 1.5 pounds per week for no reason. I became so fatigued I had to start napping. My doctor ran tests and I tested positive for Hashi antibodies, something that had never been tested. I have also intermittently had hyperthyroid symptoms a couple of times this spring. My doc ran a bunch of tests and was going to skip the ferritin until I told her my hemoglobin was 12 during pregnancy, but ferritin had tested low. She tested it and though my hemoglobin was 12, ferritin was 3, TBIC was 516 and sat was 10%. My vitamin D was also 8.6. I am now on iron and vitamin D supplements for the past week. Feeling fatigue again, and still gaining weight despite not eating much. I’ve also been reading about glutathione, turmeric, and cordyceps for Hashimoto’s supporting the immune system/warding off attacks) and may also start those. Thoughts? My ana came back at 9.9 (units) and 6 is a strongly positive reaction. With joint pain, I am now getting additional tests for other CTDs in case the ana is not from a thyroid attack. I have also had alopecia, had asthma (congestive) return last fall, and have RA, vitiligo, alopecia, and hypothyroid in my family.
Hi! This is great information. I’m currently pregnant and my iron levels (the 4 active ones) came back close to optimal, but dropping since my last test and my ferritin has dropped from 24-13. I went in to have my thryroid labs rerun b/c I seemingly randomly began have crazy heart palpitations and I thought it was due to taking my afternoon dose of NDT, but my thyroid labs came back and that doesn’t seem to be the case – I am still waiting on RT3 though. I dropped my dose myself b/c I thought maybe I had moved into hyper, but that clearly isn’t the issue. My doctor suggested I go back up to my normal dose of 3.5grains and see what happens, while working to get my iron up and switching brands of iodine…I’m a little nervous b/c the heart pals have been terrifying and calmed some when I dropped the dose. Do you have any idea if I can stay on NDT while increasing the iron or will I have to do something to drop the NDT – which is scary while pregnant? Thanks of your wisdom…
Hi Gypsy,
I recommend you go back to the physician who provided you with the NDT for further recommendations, I don’t know the full story so I can’t comment. Each person is unique and different and this is magnified while pregnant.
Any thoughts on how to convince a doctor that my hypothyroidism is central? My antibodies are low. With my Free T4 at the low end of the normal range, my TSH is almost zero. It matters because I also have other issues that could be pituitary.
Hi Lianne,
Trying to convince your doctor of anything is usually futile and frustration. It’s far easier to simply switch providers or find someone more willing to work with you. At the end of the day it’s really not worth sacrificing your quality of life (at least in my opinion).
Hi, I am hypothyroid with Hashimotos. I just got lab work done with an iron level if 52 and a ferritin level of 9. My Tsh is 5.260. I am perimenopausal and despite low tsh I have list 20 pounds in the past year in a half due to extreme anxiety which I was told was due to the Peri menopause. I am in the process of finding a holistic doctor, but for now I need to know what type of iron and how much I should be taking. I am very cautious about supplementation and I usually feel most comfortable starting low and gentle and increasing dose as I see there are no negative effects. Also, is there anything I can buy over the counter? Any advice you can give me us greatly appreciated. I have been through so much thus year with the Peri menopause and anxiety. Thank you!
Hi Elizabeth,
There are links to my recommended brands in this article, they are both gentle and generally well tolerated.
Hello,
Is it possible to treat Hypothyroid issues without knowing your Iron levels? I have low T3 and low T4 with high RT3. I have been on 1/2 grain of NDT for a year and I felt better initially but now I feel terrible again. Can I up my NDT or add T3 only without worrying about my iron levels?
Please, please, please help me. I have been ACTIVELY seeking diagnosis, treatment, my life back for 20 years (since I was 14 yrs old). I’ve torn my trapezius in my sleep 3 times between 14 and 22 years old. And I’ve been in significant pain since the start. Neck and tension headaches that keep me at a pain level between 6-8 (out of 10) 24 hours a day. Blood tests over the last year show low B12: 141 (155-700). High c-reactive protein 13.8 (<3.0) High 8am, 4pm, 12am serum and salivary cortisol. But UFC test is fine. Low phosphate 0.77. High Chloride 109. TSH 3.85. Low T4: 8.6 (9.0-23.0). T3: 4.2. RBC 4.02 (4.0-5.6). Low hemoglobin 119 (120-160). Low hematocrit 0.351 (0.360-0.480). I Severe fatigue, muscle weakness, large recent weight gain, Intense mental fogginess, memory that has severely declined, anxiety, zero libido, hair loss, etc, etc.
I should add that I’ve tried all the typical medications. 6 different antidepressants including elavil for tension headaches. Medications that increase my norepinephrine send me to the ER. Fibromyalgia medications. Epilepsy medications. I tried taking B12 multivitamins but this caused my pain to skyrocket so now I get monthly injections. The injections have made me worse as well causing muscle weakness; I can no longer engage working out as this too makes me worse. I’ve tried all types of therapies: massage, chiropractic, physio, acupuncture, pain counseling, meditation, colon hydrotherapy. I’ve tried local anesthetic and botox injections. The only medications that have helped are the combo of muscle relaxer + ketorolac but unfortunately my body is starting to build up immunity to it. I now have to take percocet. When I took 2mg for the dexamethasone suppression test (to test for cushings), that was the first time I felt significant relief for a cpl days, but I’ve been told thus can’t be used as a therapy. I’ve been on synthroid 25mcg for about a month but haven’t noticed any benefit as of yet. Thank you for taking the time to read about my journey.
How do thyroid nodules affect function. Mine is 2.1 cm. I don’t know if it is cancerous. I think I am going to skip the cancer tests and just have it removed.
Hello Dr Childs – I am so sad. I have been dealing with hair loss since March. It has gotten worse the past month. My dermatologist tested my ferritin levels in March and they were 15. she prescribed me biotin forte and 100mg of iron supplement. i couldn’t take 100mg due to constipation so i took at least 50mg each day. She also suggested I get off my birth control pills or change to a different one. So I immediately stopped taking my birth control and started a new one in June.
When I went back to the dermatologist in August she saw my hair loss still continued and was honestly worse. She prescribed me spirolactone which i was afraid to take since I could not find any evidence of this drug to be used for hair loss only high blood pressure. When she ran my ferritin levels in august they went up to 67. But she said they need to be 70 for hair growth. Is this true? I started taking 100mg of iron now and use miralax for the constipation issue.
I changed my primary care physician to someone who is and internist/functional doctor. He ran some blood work but unfortunately, I did not quite understand what he was treating me for. I believe he said undertreated thyroid and adrenal issues. He has put me on the following: Lugol’s solution, selenium, adrenal, dhea and changed me from levothyroxine to nature throid. He also suggested i start taking probiotics and digestive enzyme. He does not want me taking the spirolactone that the dermatologist prescribed.
Could what he prescribed help me with my hair loss? I am so sad and feel lost. My hair loss is affecting my relationships, work, sleep, everything.
I went to a new dermatologist and she tells me that my hair loss is probably from medication (changing birth control pills) Her only recommendation was wait it out. She prescribed me fluocinolone acetonide .01 to put on my head every night. What will fluocinolone acetonide do for my hair? Is it safe?
I am scared and do not know who else to turn to. I found our page and you seem like a caring person who is very knowledgeable. Please help me.
Hi Cheryl,
Thanks for reaching out. I would take a look at this page which goes into detail about how to treat hair loss and gives many options that actually work: https://www.restartmed.com/thyroid-hair-loss/
The current therapies may help to alleviate your hair loss but it looks like you also might be missing some important factors.
God bless you for this article! You are above and beyond of all the physician!!! Sadly, it took me 14 years to learn that my hypothyroidism was due two low iron levels. Physicians just throw the drugs for your thyroid at you,they don’t tell you how important certain nutrition is for your thyroid( in my case it was iron), even the best doctors that I’ve known didn’t know that iron is so crucial for thyroid health. When I was anemic my body wasn’t converting T4 into T3. When I started taking iron on a daily basis my body started converting all T4 into T3 three like crazy. It got to the point I had to completely get off thyroid medication! And they tell you that thyroid condition is not curable and you have to take medication for the rest of your life. I am proving live that is not true. I’m just amazed how smart you are and would like to know how did you get so knowledgeable and smart in this area and the other Physicians are not trained and smart-ass you are when it comes to thyroid health. In fact it was your article about iron that give me the knowledge to stick with iron supplements, (I always struggled with iron) and gave me “cure”. You should educate the other Physicians! Thank you so much once again you’re the best!
Hi Yulia,
Thanks for the kind words and I’m glad that it is helping you. I just spend a lot of time researching 🙂
Thank you so much for taking the time to write this article and to answer concerns. I have Hashimotos and my TSH is currently almost 10. My T3 was in normal range and so was my T4. I was diagnosed with Anemia and my Ferritin is 9. I am also low in vitamin D and B12. I do feel somewhat tired but I am able to function. My question is should my vitamin deficiencies be corrected before my thyroid medication dose is increased? Is there a possibility that my thyroid will improve without increasing medication? I currently am taking Synthroid 50 MCG. Thank you so much for taking time to help people. God bless you!
Sincerely,
Elizabeth
Hi, both of my daughters have very low ferritin levels and autoimmune hypothyroidism and very low FT3. Both have started taking natural hormone replacement for about one month, 1 1/2 grain Naturethroid. I gave them the iron supplement (capsules) you mentioned in your article (thanks kindly for your well documented information as this is just what our problem seems to be) sometimes 2 or 3 times a day with vitamin C (1g to 3g) with and without food and complex vitamin B’s (same brand as the iron). Also, both girls have good RBC and hemoglobin numbers, indicating only ferritin between 8 to 23 to be below range. This just may need more time, more iron etc? We will be checking for new FT3 levels in about a month, and I will add in at least a ferritin to those tests. The problem is that my youngest daughter has severe chronic fatigue with headaches. And, to some extent my oldest daughter cannot lose weight.
Hi Dawn,
Unfortunately replacing iron takes several months, sometimes 6+ months depending on the person.
Hi Dr Childs, I found these articles brilliant as are you, but where can I find someone like you here in the UK? I live in south west Wales. I am at my wits end trying to get my GP here to understand and they stick firmly to the lab ranges. I am terribly short of breath, ferritin 28, folate 3.8, active B12 47 and have just finished 5 x B12 loading doses. How I persuaded my GP to do this was a long procedure. Lungs, heart and finger oxygen levels all OK. I have hypothyroidism and FT3 is 4.2. TSH 0.57, FT4 18.5. D3 was 61. Feeling dreadful. Just started D3,MK7, Methylfolate and iron supplementation with Vit.C at doses found on all the helpful forums. I take Omerprazole as I take NSAID’s and methotrexate for R.A so have just started ACV and lemon juice before meals to help with possible low stomach acid. GP will not test for iron but has tested for P.A and this was OK. Hg and haemocrit lower than normal, RBC DW high, MCV higher than range. Breathing is very laboured and I feel as if I have pressure in throat and chest area as if I’ve swallowed a tennis ball. Feels very similar to heartburn but higher up.
If you can put me in touch with someone in the UK I would be very grateful. Thank you for reading.
Thank you so much for this information.Im 44yrs old How much should I take,of the liquid or capsules a day? I went yesterday to get my result and ferritin level is “5” and iron,serum is 24 my next lab test will be in 6 months.Thank you ahead
Thank you for the informative article. I am hoping you might provide some information on why serum iron continues to rise (despite not supplementing) and concurrently ferritin levels continue to fall. I am finding it very difficult to find this information and my thyroid doctor doesn’t seem to think it’s a problem.
How do you feel about lactoferrin, or more halolactoferrin to raise iron and ferritin?
Wow this article has helped me so much. I had no idea that my consistently low iron levels could have anything to do with my thyroid. I have a goiter and thyroid nodules. Could these issues be related to my constant low iron levels? I’ve had to have iron transfusions twice.
Your website is AMAZING, my goodness! Thanks for all the detailed information and for freely sharing it! I’m finally making sense of what I’ve been suffering through all this time.
I’ve been on Synthroid for years and after increasing the dosage, my symptoms were somewhat better but I was still not feeling great and recently considered switching to NDT. I did my thyroid, iron and complete blood panel tests and my FT4 is a little lower than midrange while my FT3 is also in the lower mid range level. TSH is 0.56. The only extremes were my Ferritin (19 ng/ml) and my Vitamin D (20.6 ng/ml). My Total Iron and % Iron Saturation values are just suboptimal while my TIBC is great.
I’ve used a low dose of Cytomel/T3 with my Synthroid in the past and just felt awful on it so I’m slightly worried I’ll have the same reaction on a NDT. Do you think I should focus on raising my Ferritin and Vitamin D levels and seeing if that helps my thyroid symptoms and my FT3 levels before trying to switch from Synthroid to NDT?
Excellent article. My daughter is a puzzle! After showing severe fatigue, headaches and sudden weight gain (30 kg in 6 months ) we set out to find answers. She has had a diagnosis of hashimotos but also low iron. Put on NDT and iron supplements…. this is despite having heomchromotosis. Very pale, loss of hair, diagestion issues. Also diagnosed with pyroluria. So trying to put the heme issue together in my head!!!! She felt better for a short time on NDT but was taken off this and told she was borderline…. doctors keep telling her she has low iron but then say it is impossible to have hemochromotosis and be anemic! What do we try and investigate further? Energy levels have improved on zinc b6 and magnesium supplements but can’t shift weight even on very restrictive diet.
Hi Dr. Childs,
I have a question, I don’t see this addressed in your article. I just got my iron panel back. Here are my numbers:
Ferritin 48 optimal is 40-50
Iron 56 (range 35-175)optimal would be 105
TIBC 269 (range 250-400) optimal would be 325
% saturation 21 (range 15-50) optimal 35-38%
My Ferritin is neither low, nor high, but optimal, but all other numbers are low and I have a few symptoms of low iron, primarily fatigue, sometimes significant.
Would I need to supplement? Would that cause my iron storage to go up?
Thank you!!
Hello Dr. Childs.
Our family Dr. told me that I have a lazy thyroid by just touching the glands. Presently I am taking Levothyroxine 0.05mg once a day. I will like to stop taking this medicine because is not helping me. Every day I feel very tired. Do you recommend a natural treatment for it? Please advise.
Best wishes,
Carlos
Thank you, Dr. Childs, for the information on low iron and hypothyroidism. I have been suffering from increased hair loss and brittle hair. The information you provide has been very enlightening. My doctor told me I needed to take an iron supplement – but neglected to instruct me on HOW to take the supplement. I have been taking a liquid supplement, but I now know that I have been taking it wrong. I will follow your recommendations for a few months and have my levels rechecked. The information you have posted correlates to a lot of what has been going on with me. Hopefully, my iron levels will be optimal and my other symptoms (hair loss, brittle hair) will improve.
Thank you for the explanation and also to all the people who have shared their own situations, as it all helps people like me form a picture.
I have hemochromatosis which is controlled through venesection, together with hypothyroidism. I was recently diagnosed with low iron, 6 Hb, and 10 Stored Fr. This diagnosis after I suffered from anxiety, fatigue, high heart rate, weight gain, muscle weakness and aches and cold.
I have increased my thyroid medication (up from 50 ug to 75ug) but do not know if I should supplement with Iron? I am concerned that the Iron supplement will go directly to the hemochromatosis and I will end up back on weekly venesection (my levels were 23Hb and 890 Fr before venesection).
Hi Dr. Childs,
I just wanted to verify with you what was the actual optimal levels of Ferritin? In this post you say it’s 40-50 but in another post (https://www.restartmed.com/increase-free-t3-naturally/#tab-con-0)you say it’s 70-80 for women. So is 40-50 for men?
Thanks a lot! All your work is much appreciated!
Elo
Hi Elo,
The optimal level really depends on what you are using it for. Hair growth, for instance, requires a slightly higher number than for other conditions.
How about for optimal energy levels? I have had my thyroid removed due to cancer and wanna do everything that I can to get my energy back!
Thanks a lot!
I am so thankful that I found your website.
My Dr. has recently (in the past 6 months) prescribed Levo with my TSH currently at 11. My T3 was in normal range and so was my T4. I just left the hospital last week after I passed out several times and received a blood transfusion. My Hemoglobin was an 8 but I do not know my current ferritin level. It has been as low as 1 in the past. I was hesitant to take the levo because my t3 and t4 were normal. My question is should my iron deficiency be corrected before I start taking the levo? Is there a possibility that my thyroid will improve on its own without taking thyroid medication?
Hi Kelly,
It’s really up to you and I don’t think there is a wrong or right answer as it won’t take long to figure out if iron helps your thyroid function and you can go from there.
Hi Dr. Westin,
This is probably first time I am replying to blog post. It feels like after 20 years I am going to get correct diagnosis.
I am 39 (I have been diagnosed with Hypothyroidism when I was 20 but am sure I have it since childhood or may be from birth. When doctor checked me first-time when I was 20, TSH was 150+)
If I don’t take thyroid medication (T4 only drug) my TSH become 150+ (yes you read it correctly)
After T4 medication (100mg T4)- TSH comes normal but my T3 is far far at the lowest range and T4 is at middle range.
*Symptoms:*
I feel NO better.
I have very very thin hair
constipation,
pale skin and I have very dark circles around whole eye – peripheral dark circles (everyone new who meets me asks – if I am ill or something has happened to me)
Terrible mental fog
Extreme level forgetfulness
I take zinc, copper, iron, iodine (according to Doctor I don’t have Hashimotos and Antibodies test is normal), B-Complex, Omega-3-6-9
(and few other vitamins and minerals)
In India, we don’t get doctor who can prescribe NDT medicine, I have ordered and tried couple of from OTC meds USA (ThyroGold) and from Thailand
—> But I get common issue with these that my TSH goes very very low
(0.03 or 0.005) but T3 and T4 both extremely low too.
Adjusting the dose (lowering the dose doesn’t help)
So I can’t take NDT, and I am on T4 only.
My Ferritin is ALWAYS low (between 10-20) from years and years. High doses of Irons make it max 30-35. My Iron serum also is very low (40-50)
But my HB is 13. So my doctor thinks I am alright but I know I am not.
I have very light menstruation periods. (I am vegetarian)
Can you please help me/ guide me.
Is it possible to book an online appointment.
Excellent!!! I wish every woman could read this article! I neglected my health and as I entered my 40’s my health totally crashed. I ate pretty healthy but my iron stores for low. I let it go and when I was basically not far from death I finally decided to look for answers. Anemia went on undiscovered. When it was discovered (ferritin 0) we started a treatment plan. Three years later as iron improved hypothyroidism was discovered and started treatment for that recently. Doing better and still in recovery.
Hi Patricia,
I’m glad you are doing better now and thanks for sharing your story!
Dr. Westin,
I’m suffering from High cortisol levels, High TSH and RT3, insulin resistance, low testosterone hormones. In your article you mentioned it how Iron is critical for proper thyroid functions but I have been told by several doctors not to take iron supplement due to beta thalasemmia (minor). I haven’t take any medications or supplements yet since i just got my results few days back. What anemic people should do if they suffering from hypothyrodosism?
Hi Bindesh,
Your doctor is correct that you shouldn’t take iron if you have thalassemia. Because of your condition, you’ll have to focus more on the optimal ranges for thyroid hormone and “brute force” yourself into the necessary range. You can find more info about that here: https://www.restartmed.com/normal-thyroid-levels/
My low thyroid problem has been going on for years. My doctor knows I have low iron and problems with iron absorption from my hematologist; but she states that low iron does not have anything to do with thyroid function.
My hair is falling like crazy and she says that the only thing she can do is increase the potency of my thyroid medication.
Well, that has not worked for the last three years (by the way, she is a GP/almost) and my hematologist who checks my iron and my (almost doctor) will not talk to each other. She also refused to read your article.
I’m getting more tired each day and cannot focus. Also I have developed depression and anxiety issues. Again, she says that anxiety and depression are not related to thyroid function.
Can you please tell me what I can do since no one is listening to me and I am barely able to get up and function?
Thank you!
Hi Teresa,
It sounds like you need to seek out a second opinion and to find another doctor! You can use this resource for guidance: https://www.restartmed.com/thyroid-doctor/
I have been tested for thyroid but all levels are “normal”. I have 2 modules on my thyroid. Endo says everything ok because levels normal. Problem is I also have polycythemia vera – a rare blood cancer where my bone marrow makes way too many red cells and they are misshapen. I take chemo drugs and still need bi-monthly therapeutic phlebotomies. So the problem is my iron is very low and I cannot take ANY iron to supplement because it would cause my body to make more blood so how can I get my thyroid hormones to work for my body or is it just not possible to get help for this. I would like a Dr.who understands but I can’t keep shopping around.
Hi Judy,
If you can’t take iron it means you will most likely need to optimize your thyroid medication using T4 + T3 thyroid medication.
Hey there Dr. Westin,
Great website and Youtube videos. My situation in a nutshell:
About 6 years ago, I experienced 12 straight months of intense physical stress and ever since my sleep has been bad (restless legs). Blood work shows:
Free T3: low lab range
RT3 is high lab range (which makes sense after your explanation)
TPO AB’s at 35 so above range
Serum iron: very low lab range
TIBC/saturation: low lab range
My cortisol rhythm is out of whack too. Between iron, thyroid and adrenals, which one of these problems would you tackle first? Do you think healing my thyroid and/or adrenals will help with the serum iron issue somehow (therefore fixing my RLS)?
Hi Andrew,
There’s no reason you can’t tackle several at once (or all at once) as they are probably all related in some way. You’ll have much better results and experience much faster improvement if you take this approach.
At what point do you decide a patient is not absorbing oral iron and it is time to try something else?
I am currently pregnant and have struggled with low iron throughout my pregnancy. The fatigue this pregnancy has been unbearable. Around 12 weeks I had my levels checked and my ferritin was 8 and serum iron was at the bottom of the range. At that time my hemoglobin, hematocrit, etc. were on the low range of normal.
I began taking Optiferrin 3x daily. I had my iron tested at 24 weeks and my ferritin is 5, serum iron 15, transferrin 384, transferrin saturation 3%, Hgb 11.9, and HCT 36.9. I feel awful. I have restless legs, shortness of breath, and extreme fatigue. I asked my primary care doctor if she would send me for iron infusions and she refused, stating she would only do so when my hemoglobin got down to 7. She told me I was iron deficient but did not have anemia yet. So basically I have to get worse before my doctor will do anything. She prescribed oral iron ferrous sulfate 325mg and told me to take it twice daily. I did for a few days but got incredibly sick with painful gastic pain and diarrhea. I discontinued taking the oral iron because the side effects did not feel worth it. I would rather be tired than go through that. I cannot get through my work day without having to take a nap or nearly falling asleep. I bought a bottle of the liquid iron recommended and I am going to give it a try. But this feels like such a slow process.
Hi Stormyshay,
Usually, if the patient hasn’t seen a noticeable improvement in a few months.
Hello! I would appreciate some help. I have Hashimoto’s. Currently taking 180 Armour.
Most recent labs:
Iron, Total: 43 (range 45-160 mcg/dl)
Iron Binding Capacity 321 (range 250-450 mcg/dl)
% Saturation 13 (range 11-50%)
Ferritin 53 (range 10-232 ng/ml)
TSH 0.193 (range 0.45 – 4.50 ulU/mL)
T3 Free 3.6 (range 2.0 – 4.4 pg/mL)
Should I be supplementing Iron? what does it mean when all of these iron tests seem low except for the IBC?
Thank you!
Hello, thank you for the information. What to do when you have an extremely low ferritin level(7) but your thyroid panel is within “normal” range?
Hi Angela,
Treat the iron to see if the thyroid improves 🙂
Is it common that you start to gain weight rapidly when you start taking iron supplements? I’m taking 50-100 mg a day, and I can feel myself blow up like a balloon even though I’m eating the same way I have before when my weight remained stable.
I’m quite anxious about this as I desperately want to get my life back, but I definitely don’t want to end up overweight 😐
Hi Kaitlin,
And no, that’s certainly not common.
Dr Childs,
I have had a thyroidectomy. I am struggling with fatigue and I recently had my ferritin levels checked and they were 57. I have been reading on other sites optimum is 70-100 for women? Do you think this may be true for me especially because of no thyroid? I am fatigued but I struggle with exercise intolerance and sire made sense to me reading symptoms of low iron?
Hi Kim,
No, I don’t think it needs to be that high. Most people with hypothyroidism are under-treated but have been told their labs are “normal” which could be happening in your case. Iron is dangerous and you really don’t want a lot of it in your body.
Hi, thank you for this. What if you have high iron but low (30) ferritin?
Hi Lily,
It means your iron stores are low.
Hello Dr. Childs,
I read this article and found it very helpful…especially the relationship between iron and thyroid. Thank you so much. What I didn’t see mentioned is how to adjust the saturation.
I can see that my Ferritin is high and I do know it is due to inflammation. I’m also on T3 only for thyroid.
What is confusing me tho is that my iron labs look normal to me except for the saturation which is considerably low.
Ferritin 40-50 61
Serum Iron Middle of the range 64 (27-159)
TIBC Middle of the range 338 (250-450)
% Saturation 35-38% 19
How do I raise saturation when the rest looks ok? Do I take iron supplements?
Thank you,
Elsa
What about hemochromatosis? Is there considerations or connections here? Any differences/extremes if you carry 1 vs 4 genes?
Hi Dr. Childs,
I was lucky enough to get two iron infusions about a month ago. Since then my hair has begun to fall out more, and I’ve gained about 4-5 pounds (which goes a long way when you’re short). I’m hypo and taking nature-throid. Is it possible that infusions could affect my thyroid functioning?
I didn’t see my particular scenario on here. Iron was 133, saturation was 48%, which was flagged high, and ferretin was 47. Do results like that correlate with anything like a methylation problem? My B-12 was slightly under 400 and Iodine was flagged low. My Dr said that was fine but why would the saturation be flagged? I have all those symptoms above except for hair loss.
Is there a contradiction regarding ferritin..?
In one weight-loss case study (https://www.restartmed.com/weight-loss-hypothyroidism-success/) you are writing:
“Through treating hundreds of patients I’ve found that optimal thyroid function happens when Ferritin is around the 70-80 range.”
..while on this page you say it is 40-50 range.
(“Ferritin – Optimal Levels = 40-50”)
That’s a bit of a difference – which one is correct..?
For someone with BOTH iron deficiency & hashimotos – is it unusual for TIBC to also test low and outside the normal range? TIBC should be higher with low ferritin levels, but my TIBC is also low. Is there any additional testing I should ask my doctor for? Thank-you
Can the liquid iron be safely added to your hypothyroid bundle + your Vit D and Thyroid Regrowth?
It is my understanding that using Turmeric/Curcumin can block absorption of iron. Do you think that spreading out the dose of each by several hours would be ok? I would like to take Turmeric to help with inflammation and nodules from Hashimoto’s, but have very low ferritin that I am trying to resolve as well. I’m just not sure if just taking it in general will negate the iron I take.
Hi Diana,
I’ve never seen it interfere with iron absorption in any meaningful way but if you were concerned then taking it apart is probably a good idea. When it comes down to importance, iron/ferritin would take precedence over turmeric/inflammation, though, so keep that in mind as you make any changes.
Hi, Dr. Childs,
I want to thank you so much for this article. I have been dealing with shortness of breath for nearly three years. I take Armour for Hashimoto’s and my doc and I assumed the breathless had something to do with Hashi’s and/or the medication. After I read your article and recognized that many of the symptoms you listed I was experiencing (and thinking they were thyroid related), I asked my doc to do the tests you recommended. All of my numbers were in the low end of the normal range and my %saturation was 18 (range 20-50). My doc suggested that I eat more foods containing iron, but to no avail. I started using liquid iron about 5 weeks ago. At week four I noticed an absence of breathlessness one day. It was the first day in three years. Although the shortness of breath has not completely resolved, I believe I’m finally headed in the right direction. (In addition, I have more energy, less hair loss, and I’m thinking more clearly too.) So, thank you so much for the work you do, and specifically for this article. I had almost given up.
Best to you.
Hello, can we take the iron capsules with your thyroid daily essentials multivitamin? I notice that multivitamin doesn’t have iron, am I correct?
Hi Esperanza,
It would be best to space out your iron capsules with all of your other supplements and medications including thyroid daily essentials. And, yes, you are correct in that it does not contain iron.
Hi Dr. Childs, I just received lab work and have low iron (66 mcg/dl), 355 binding capacity, 19% saturation, and ferritin of 93 (down from 156 last year). I have been taking homocysteine supreme due to MTHFR that I believe had helped with the ferritin. I have been borderline anemic my whole life which I am now correlating with gluten sensitivity. I also just started cytomel for a high reverse T3 (free T3 3.1, reverse 23).
My instinct was to see if iron levels rise now that I have converted to a gluten free diet. Will the wait and see approach inhibit the ability to feel well and lose weight? Would it be better to start an iron supplement and then taper off once a midrange level is achieved and see if it can naturally be sustained? Thanks for your wisdom!
Hi Corrie,
I would probably try to eat iron-rich foods and go gluten-free to see if you can naturally increase it. You can always try this for a few months to see where this puts you and then determine if you should be using iron at that point.
Hi Doc,
Just a quick question…
When someone who (according to your ranges) is low in ferritin (17 ng/mL) but optimal in serum iron, TIBC and % saturation starts supplementing iron, can they make the assumption that not only the ferritin will increase but the three optimal levels will change, as well? Or is there a way to ensure just the ferritin increases while the other numbers remain optimal and are not thrown out of range?
Thanks for these informative articles – I refer to them frequently!
Hi Victoria,
Taking iron will impact your serum iron levels somewhat but as long as you are dosing correctly you shouldn’t see a big change.
Hi Dr. Child’s. I’ve been suffering from low iron and a have had a host of different strange adverse reactions due to my hypothyroidism.
I take 120mg every day and they started me on 125mg of iron. I take a biglycinated iron. After a week, I went to bed and woke up from a flush throughout my body and my heart shot up to 169bpm followed by terrible tremors.
Since then I’ve been lowering the iron from 3, to 2, to 1 pills a day. I’ll be fine for a while until it happens again. But my iron levels haven’t improved much, even after months. I’m out of danger for anemia, but just barely. My doctor also lowered my thyroid meds believing it was the culprit. We’ve reversed course since that decision.
Today, I’m off the iron and hoping I’ll be ok (looking at liquid iron maybe), and my thyroid meds are back up to 120mg.
But I want to know… What happened? Was it cortisol? Low t3? What caused this sudden, scary side effect?
Hi Dr Childs. Been following your posts for years. This one about Iron and the Thyroid really hits home. Although TSH is 1.7 (I am not on meds) my hair is thin and falling out. It may be my iron which test shows: TIBC 525; UIBC 467; Iron saturation 11. Is it safe for me to take iron supplementation? My Ferritin is 54. Thanks! Denise
Hi Denise,
There are some who think that pushing a ferritin up to 70 or 90 is ideal but I am not one of those people. Before using iron supplements I would first check to make sure your thyroid is optimized and make sure there isn’t some other issue causing your hair loss.
There are also plenty of other treatments that can be used such as those listed here: https://www.restartmed.com/treatments-for-thyroid-hair-loss/
Hi Dr. Childs,
I recently had iron levels checked along with b12 . My iron was 157 (mcg/dl) with a range of 45-160. Saturation 44 (16-45), IBC 358 (250-450) and ferritin was 31 ng/ml. B12 was 623 pg/ml. My question is can I still supplement with b complex vitamins or do I run a risk of pushing my iron even higher? I am 62 so menopausal. I wish I could get my ferritin higher but don’t think I should supplement with iron as Im close to the top part of all ranges. Your thoughts?
Thank you for your time.
Ann
Hi Ann,
You should be fine to continue to use a B complex without the concern of pushing your iron higher. Sometimes it makes sense to use iron to bring up the ferritin but I usually make the decision on a case-by-case basis.
Dr. Westin, I have learned so much from your articles. But I have a question about Iron that this article did not touch on. I recently had my Iron checked. My Iron was 152 Range (45-160), sat. 40 (16-45), TIBC 376 (250-450), Ferritin 26 (16-232). What would be the explanation that serum Iron is high, and Ferritin is low.
Thanks!
Hi Tammy,
Ferritin is a marker of iron storage, not iron in the bloodstream. You can have low iron storage but adequate iron ready to be used in the bloodstream.
My labs say serum ferritin at 141. But I am low TIBC at 206 and UIBC at 98. My doctor didn’t do anything, but I was anemic about a year previously, eating ice like crazy! And diagnosed with Hashimoto’s then. I’ve been hypo for a long time and on Levo.
So what can I do? My ferritin was elevated probably bc of inflammation like you stated. I’m so weak lately especially after exercise. I have all the symptoms except nail spooning. I took a liquid iron at one time and it really helped with energy, hair loss, etc. I just ordered it again.
Hi Janel,
In cases such as this you will want to look at inflammatory markers such as ESR and CRP to see if the higher than normal ferritin is indeed from inflammation. Other things can contribute such as hemochromatosis which should be ruled out. You really don’t want to assume high ferritin is from inflammation without ruling everything else out first.
Dr. CHILDS, Hashimoto’s for over 12 yrs, recently gone hypothyroid despite being on same Tirosint level for over 5 yrs. Thanks to Covid, doc says, since reports are coming out that virus affects thyroids, whether or not u previously had thyroid issues, and iron. Fighting iron deficiency with levels in single digits for over 8 yrs and only this past Oct got to see hematologist. Despite 100mgs iron pills per day with vitamin C, and a 750mg Injectafer infusion back in Feb, my ferritin went from 5 in Oct to 39 in May. Been trying to get to 100, doc says ideal. Thinking it dropped even more though due to recent D&C to remove polyp and fibroid, and increased fatigue. Considering going to liquid iron, but 3 questions…
* I cannot do Floradix because B12/ Cyanocobalamin aggrevates cobalt allergy/ raises eosinophils, so I like the look of Gaia, just iron. Familiar with that?
* Also, with only 10 mgs of iron in this Gluconate, can it actually be faster than 100mgs of pills, and why/ how?
* My doctors will not test iodine or selenium, nor does endocrinologist think digestive enzymes will help. Should I try to add small amount of selenium and enzymes to try out? Can I take at same time of iron?
Hi MaryC,
I’m not familiar with the iron supplement you mentioned so I can’t speak to it. In regards to your other question, liquid iron is better tolerated but typically requires higher doses for longer periods of time to match the capsules. Lastly, you can take selenium if you’d like but I wouldn’t say it’s required and if you did take it you wouldn’t want to take it at the same time as your iron. Iron should be used away from pretty much everything else.
Hi and thanks for your invaluable articles in a world where noone seems to know much about this. I am on T4 medication and just started a drop of T3. My problem with iron is mysterious-if I do not take iron supplements my nails do not grow -end of story. I start and they grow normally, I stop and they stop and instead split into slices. My ferritin is allegedly high 171 mcg/L, iron 13 mcmol/l which is considered normal? CRP 2mg/l (so no inflammation). (Only other abnormal blood test is cobalamin high (790 pmol/L). Any idea why this is? Should I take iron supplements or not? Its a mystery
Can you speak to the role copper plays with iron deficiency? I was reading about the importance of copper and ensuring it is optimal before resorting to iron supplementation…your thoughts…?
Hi Paula,
Copper deficiency reduces how much iron can be absorbed by the body so taking copper (when deficient) may improve iron levels.
I was today-years-old when I learned about the thyroid/iron connection. I just got my bloodwork back and my T3 is low at 67, so I was searching for reasons this could be and found this blog. I’m a bit of a complex case because I have hereditary hemochromatosis as well as Hashimotos (I also have hEDS/MCAS/POTS). I’m on 88mcg of Levothyroxine and my TSH is 1.48, my Free T4 is 1.23 and my T3 is 67/low. I’m still waiting for my most recent Iron panel, but the last time it was tested 6 months ago: Iron/103; Sat %/31; Ferritin 6.6. My hematologist says she isn’t concerned about my low Ferritin. It’s been below 21 since July 2020. I’ve been controlling my iron levels with diet, so I don’t eat any foods high in iron. I haven’t had to have a phlebotomy for a year. If I eat foods with iron or supplement with iron, then my Sat % gets too high. I can’t take Vit C because I am oxalate toxic. I’m wondering if it makes more sense to add back in some moderately high iron foods and risk my Sat % getting too high – then getting a phlebotomy to balance things out regularly. I guess the short question is: Is it better to get iron levels up to support my thyroid function and get regular phlebotomies? Instead of eating low iron to keep my Sat % in a good range and risking low thyroid function? I definitely have had symptoms arise over the last year of low energy, weight gain, and afternoon energy crash/tiredness. Thanks in advance for any insight you’re able to share…
Hi Kris,
In general, you don’t want to take iron supplements unless absolutely necessary as iron can be toxic to the body which is what occurs with hemochromatosis. There may be situations in which it makes sense for therapeutic phlebotomies but there are so many other contributors to low T3 that starting with iron wouldn’t be a good idea. Other basic factors should be addressed first like diet, lifestyle, sleep, stress, etc. All of these impact thyroid function as well.
Dear Dr Westin Child
I had a compete removal of my thyroid due to Follicular cancer 8 weeks ago and i am on 100 microgram Levothyroxine tablets, my blood test at surgery on the 14 December 22 for Thyroid function test was:
Serum free T4 level 18.5 pmol/L Range (9.0 -25)
Serum TSH Level 0.08 miu/L Range (0.3-5.0)
I am a bit concerned about the low THS Level.
Your blog and information thyroid is very good in good clear manner to understand.
Hi Manoj,
After thyroid removal for thyroid cancer, doctors are generally ok with lower-than-normal TSH levels because it’s thought to reduce the risk of cancer recurrence.
Dr. Childs,
I always love your blogs. I am so happy to see this on ferritin. I’m kind of neurotic, in that when I found out I had low ferritin (after 12 conventional doctors couldn’t figure it out) I learned everything I could about iron and ferritin. I found that I became drastically better with a ferritin above 50, but really I needed to be above an 80. Once I supplemented enough and got above 80/90 I felt better and better. My hair grew like crazy and it’s like a lion’s mane now down to the bottom of my back.
I then went the functional route because the ordeal terrified me. They found I had subclinical hypothyroidism when this occurred. I forget what stage of hashimotos- 3??? (I didn’t know it at the time- learned it later from your video). I also ordered labs (ordered by my doctor or myself) almost every month for 3 years and correlated it. I studied and studied and used old thyroid meds (broke in half) to add to the ones I have to become optimal. I’m finally optimal in both the thyroid and ferritin and feeling soooooo much better.
It blew my mind how in sync my thyroid was with my ferritin labs. When my thyroid labs tanked my ferritin labs did too.
Now it has me thinking- did I ever need to supplement that heavily to begin with? All I needed was for someone to optimize my thyroid correctly! But how would that have happened with a TSH of 2.35 and slightly low T3? It was always missed by doctors. Then when I was given thyroid meds they never got my T3 right. The Dr freaked when my TSH was a 0.3 even though my T3 was low. Then my Dr moved away.
Thanks to you and Dr. Amie’s podcasts I was able to test and optimize myself and my ferritin is sitting nice at around 100, TSH is low and T3 is 3.9. 🙂 🙂 best of all I feel better.
Thank you for helping people like me. I know you don’t give medical advice because you can’t but you definitely provide the tools for us to figure it out.
Hi Robin,
Glad to hear you are figuring this out and it definitely sounds like you are doing great! Thanks for sharing your story and I’m glad you find the information helpful.
Hi! Very interesting article with helpful information. I’m trying currently to get to the bottom of some of my health-related issues. I’m struggling with my doctors either not really listening/taking my symptoms or tests seriously, or not ‘talking’ to one another. I’m struggling to understand my most recent test results. Iron panel shows saturation at 17, TIBC 323, Iron 56, but Ferritin only 11. My endocrinologist referred me to my PCP to discuss these results for either further testing or iron supplementation. I had also had a thyroid testing done, and while my TSH is 1.8 my free T4 is just .64, which I know is low and marker for Hypothyroidism. My doctor said she is not concerned because this low T4 would only be a concern if my TSH was high. I’ve read otherwise, so do not know what to think or if I should get a second opinion. I also do have a confirmed Pituitary microadenoma (4mm)that has not grown in 3 years and has been determined to be non-functioning, though I am awaiting a new cortisol test. I’ve just been unable to reconcile any of this with my symptoms. I know I’m not well but can’t determine if this all truly could be only the iron stores or if there is also something going on with my thyroid, or who to try and go to at this time, another endocrinologist or my pcp or someone else? thanks for any thoughts!