Getting a complete thyroid hormone blood test is critical to understanding and evaluating your thyroid function.
Complete thyroid testing includes so much more than the traditional TSH (which can be inaccurate in certain medical conditions).
Without the right thyroid tests, you won’t understand if your body is converting thyroid hormone appropriately or if your cells are taking up enough thyroid hormone.
The lack of these functions results in hypothyroid-like symptoms and specific changes to thyroid hormone that you can pick up with testing.
In this post, I am going to break down the most important thyroid lab tests, why they are important and how to interpret your results…
Thyroid Testing – What’s Important and Why
There’s a lot of confusion surrounding thyroid testing which can make things complicated if you are a patient suffering from hypothyroidism.
In most cases, you are left to believe that the single best test for your thyroid is your TSH.
But is this actually true? Is it supported by scientific evidence?
The answer to that question is not really, and not in every situation.
There are actually many situations in which the TSH falls short and doesn’t tell the “whole story” of what is going on in your body.
In some cases, patients understand that getting a full thyroid panel is important, but they still don’t quite understand how their results fit into their current treatment regimen.
And this is really important because certain thyroid medications influence your thyroid values in different ways.
In some cases, these changes can be misleading to the inexperienced eye, unless you know what you are looking for.
But first, let’s start with the complete thyroid panel:
- TSH
- Free T3
- Reverse T3
- Free T4
- Thyroid antibodies
- Sex hormone-binding globulin
- Total T3
This list represents the entire and complete thyroid panel.
This entire list isn’t necessary each and every time you get your blood drawn, but this should always be drawn to completely and entirely evaluate your thyroid function.
This list should be drawn BEFORE you start taking medication and it should be drawn if you are worried that your symptoms are consistent with hypothyroidism.
Remember that while testing is critical to proper diagnosis and evaluation, accurate diagnosis and treatment is still required for optimal results.
Taking this list to your doctor and demanding them to order these tests may not be helpful for the following reasons:
- If you have to ask for these tests there is a high probability that your current provider may not treat you appropriately.
- Thyroid hormone replacement is nuanced and may require a combination of T4 + T3 for optimal results, this is contrary to the standard of care which is to provide patients with T4-only thyroid medication.
- Many physicians are set in their ways and unwilling to change their practice style regardless of the data.
Instead, a better option may be to find someone local to you who is experienced in dealing with thyroid issues and can help you further.
We will touch on more of this later, but for now, let’s jump into the evaluation of each of these lab tests:
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
TSH (Thyroid Stimulating Hormone)
The TSH level stands for thyroid stimulating hormone and it is secreted from your pituitary gland.
Under normal physiologic function, TSH acts on the thyroid gland itself and stimulates thyroid hormone production.
High levels indicate that your body may not be producing enough thyroid hormone.
This relationship can confuse patients because a high TSH means that you are likely hypothyroid.
TSH levels usually rise in response to a feedback loop in the body that exists to tell the brain when enough thyroid hormone is present.
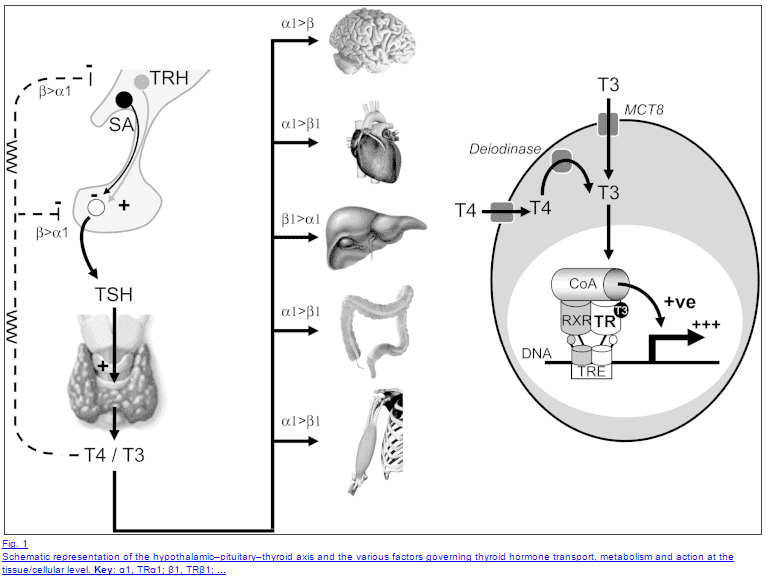
If there are low blood levels of thyroid hormone your pituitary will sense this and it reacts by increasing TSH levels in an attempt to tell the thyroid gland to produce more thyroid hormone.
This logic is then applied to thyroid hormone replacement.
When doctors give patients thyroid hormone they then use the TSH to determine when the body has “enough” thyroid hormone in the body.
As you take thyroid hormone your TSH level will fall as the pituitary senses this thyroid hormone in the blood.
Eventually, your TSH level will drop and your doctor will say that you are “optimal”, but is this really true?
In some cases, it may be, but in many cases, the TSH by itself isn’t the best marker for assessing thyroid hormone status in the tissues.
Some conditions may alter TSH levels and make using TSH inaccurate:
- Low T3 syndrome or euthyroid sick syndrome – This condition results in hypothyroid-like symptoms but patients tend to have “normal” TSH levels with very low T3.
- Autoimmune thyroiditis syndromes – Conditions like Hashimoto’s can alter peripheral conversion of thyroid hormone and result in reduced production of thyroid hormone from the gland. Many patients feel symptomatic with relatively preserved TSH levels.
- Inflammatory states that alter peripheral conversion of thyroid hormone – Inflammation in the body will result in reduced T4 to T3 conversion in peripheral tissues. The pituitary lacks deiodinase to create reverse T3 which can “trick” the pituitary into thinking more thyroid hormone is available.
- Leptin and insulin resistance – Hormone imbalances can alter thyroid hormone function at the cellular level. Even if circulating thyroid hormone levels in the blood are normal that doesn’t mean that adequate cellular uptake is achieved.
Beyond these conditions that may alter the effectiveness of the TSH as a marker of thyroid status, there are also some studies that refute this point.
Some studies have shown that patients who take T4-only thyroid medication to lower their TSH to the “normal range” still exhibit lower T3:T4 levels compared to age-matched controls (1).
What’s even more interesting about this comparison is that the patients taking thyroid hormones were likely to have more weight gain and were much more likely to be taking medication for depression, high cholesterol, and high blood pressure.
Patients taking T4 to a “normal” TSH also consumed fewer calories per day and showed a slower metabolism compared to matched controls with the same TSH levels.
These findings match my observation in clinical practice as it relates to hypothyroid patients being treated with T4 thyroid medication.
Most of my hypothyroid patients are consuming very few calories, have a big problem losing weight, and are usually taking multiple medications.
Obviously, our understanding of TSH as the “ultimate” thyroid lab test is limited, and as a result, it’s a good idea to use other lab values in conjunction with the TSH for a better understanding of what is happening in each patient.
While the TSH may not be the best test it still has value so don’t discount it completely.
Normal & Optimal Ranges for TSH
So how can you use the TSH appropriately?
Monitoring your TSH while taking thyroid medication is very important, but it shouldn’t be used by itself to alter your dosing.
Instead, it should be used with the other lab tests listed below.
In addition, what constitutes a “normal” range?
The optimal range for TSH, assuming you aren’t taking thyroid medication is less than 2.0.
This assumes a standard range of 0.3 to 4.5 (or 5.0 as in the case below).
Generally, healthy patients exhibit a TSH of less than 2.0 (2) and patients with a TSH higher than 2.0 usually have hypothyroid symptoms.

The example above is a patient with obvious hypothyroidism because their TSH is outside even the “normal” range.
In most cases, the TSH will likely fall between 2.0 and 4.5 which is probably the worst range to be in.
Patients in this range will be told that they are “normal”, despite being symptomatic.
Many physicians will use the standard reference range of 0.3 to 4.5 instead of the optimal range of less than 2.0.
When you are first evaluated (prior to taking thyroid medication) make sure you evaluate your TSH with this optimal range in mind.
Free T3 (Triiodothyronine)
The next test we need to talk about is probably more important than the TSH and that is free T3.
Free T3 is critical because it is THE active thyroid hormone in your body.
All of the positive actions we associate with proper thyroid function is from T3.
T3 directly activates nuclear receptors on each of your cells and changes genetic transcription which results in increased metabolism, increase hair growth, increased energy production, etc.
Free T3 represents the amount of free and active thyroid hormone floating around in your blood.
Some of this thyroid hormone is bound to a protein for transportation (this number is included in the total T3), but we are more interested in the part that is unbound and free.
By assessing your free T3 levels you some insight into how your body is metabolizing thyroid hormone.
In order for T3 to be created your body must cleave off an iodine moiety from T4 through enzymatic activity.
This process is known as thyroid conversion and it occurs in peripheral tissues, in the liver, and in the GI tract.
Conditions that alter your conversion of T4 to T3 may result in low T3 syndrome or euthyroid sick syndrome.
In some states, your body may produce enough T4 which may result in “normal” TSH levels but inadequate T3 due to reduced peripheral conversion.
This state presents with hypothyroid-like symptoms and is frequently missed by many providers and patients.
Conditions that cause low T3 and reduced peripheral thyroid conversion:
- Systemic inflammation (high ESR/CRP or ferritin levels)
- Chronic yo-yo dieting
- Rapid weight loss (as in the HCG diet)
- Certain medications: Beta-blockers, antidepressants, anti-seizure medications
- Chronic illness or recurrent chronic infection
- Chronic stress
- Hormone imbalances and hyperglucagonemia
Evaluating your free T3 is necessary to understand how your thyroid is functioning in the peripheral tissues.
Free T3 normal & Optimal ranges
Like TSH, taking thyroid medication will certainly alter free T3 levels.
Doctors give patients T4 thyroid medication with the supposition that the body will take the T4 and turn it into T3.
It turns out that this can be evaluated by testing your T4 and T3 both before and after treatment.
If you see that T4 levels have increased, but T3 levels remain low (or slightly increased) you can infer there might be a problem with thyroid conversion.
Remember that T3 thyroid hormone is about 3-4x more powerful than T4 at lowering TSH (3) (but varies from patient to patient), so taking T3 thyroid-containing medications will likely dramatically drop your TSH level.

Despite this studies have shown (4) that when treating with T3-only thyroid medication (compared to T4) and even down to a “normal” TSH, patients taking T3 medications have more weight loss than those on T4-only thyroid medications.
If you are taking T3-containing medication then evaluating your free T3 level becomes more difficult and less reliable.
However, assuming you are not taking T3 thyroid-containing medication, then the “optimal” range for free T3 should be in the upper 50% of the reference range.
Low free T3 levels, even with a normal TSH, generally present with hypothyroid-like symptoms.
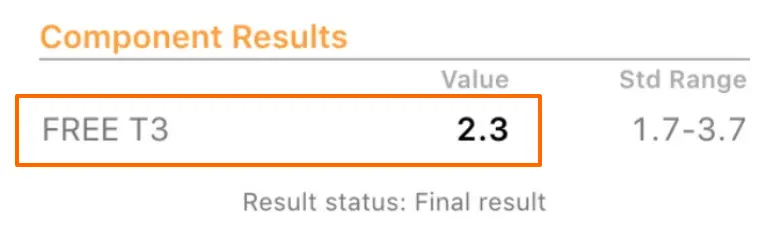
You can see an example above of a suboptimal free T3 level but still “normal”.
Reverse T3 (Reverse Triiodothyronine)
Reverse T3 is another VERY important thyroid lab test and it gives a lot of information.
Reverse T3 is an inactive thyroid metabolite.
Remember when we discussed that your body can convert T4 into T3?
It can also turn that T4 into reverse T3 instead of T3 which inactivates the thyroid metabolite.
This system is meant to act as a brake and is a good thing in certain situations.
However, like many other processes in the body, this normal system can go haywire.
States of chronic stress, illness, dieting, weight loss, etc. can trigger the conversion of T4 to reverse T3 and act as a brake to your metabolism.
Checking your reverse T3 can give further insight into the conversion process in your body.
Patients with poor thyroid conversion will usually present with high reverse T3 levels, low to normal TSH levels, and a low T3.
Reverse T3 can also give insight into how much competition your body has for cellular binding between T3 and reverse T3.
In most cases, you want this spectrum to be in favor of free T3 binding (so that you get the benefits of thyroid hormone).
Patients with high reverse T3 will often present with weight gain, very slow metabolism, and other symptoms of hypothyroidism.
Reverse T3 normal & Optimal ranges
If you are taking T4 thyroid medication you will want your reverse T3 to be less than 15.0.
The standard reference range usually varies between 9.0 to 25.0
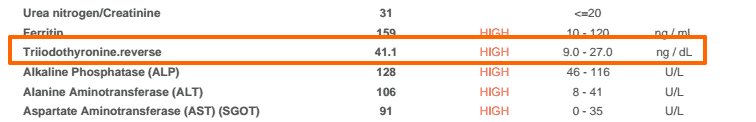
A reverse T3 greater than 15 with a lowish T3 is usually compatible with symptoms of hypothyroidism and a condition known as tissue-level hypothyroidism (5).
This is another syndrome where TSH levels can falsely predict peripheral tissue levels of thyroid hormone.
In most cases, you will probably have to ask for the reverse T3 to be tested as this is not a standard thyroid test providers are used to ordering.
Remember to evaluate your reverse T3 in conjunction with both the TSH and free T3 levels.
Reverse T3 levels are closely associated with weight loss and metabolism:
The more rapidly you lose weight the higher your reverse T3 will be and the slower your metabolism will be.
This usually occurs with extreme calorie restriction.
The example above is from a patient who just finished the HCG diet and presented with rapid weight gain and symptoms of hypothyroidism.
This high reverse T3 is likely a compensatory reaction from the dramatic drop in weight and is meant to help lower her metabolism to “protect” the body from the rapid weight loss.
Safe weight loss does not result in this type of rising in the reverse T3.
Free T4 (Thyroxine)
Your free T4, while not the active thyroid hormone metabolite, still has value and is worth evaluating.
Free T4 can give you insight into how your body is absorbing thyroid hormone.
In some cases, usually due to gastrointestinal issues, patients do not adequately absorb thyroid hormone.
This has given rise to newer thyroid medications with fewer inactive ingredients like Tirosint which can help in absorption.
By assessing free T4 levels before and after initiating thyroid hormone you can determine how well you are absorbing thyroid hormone.
T4 levels also give insight into how well your body is converting thyroid hormone.
High levels of free T4 with low levels of T3 may indicate a conversion problem.
But be careful:
High or normal levels of T4 do not necessarily indicate that your body is utilizing thyroid hormone in peripheral tissues.
Free T4 normal & Optimal ranges
Free T4 levels can change depending on the type of thyroid hormone you are taking.
Your free T4 level, like free T3, should be in the top 50% of the reference range – assuming you are NOT taking thyroid medication.
Your T4 levels will increase when taking T4-only thyroid medications like levothyroxine, Synthroid, or Tirosint – but this isn’t necessarily a good thing unless you are also converting this T4 to T3.
Conversely, your T4 levels may drop dramatically when taking NDT and/or T3-only thyroid hormone.
Your T4 level in these cases is usually not as important as your free T3/reverse T3 ratio, but it’s still worth evaluating.
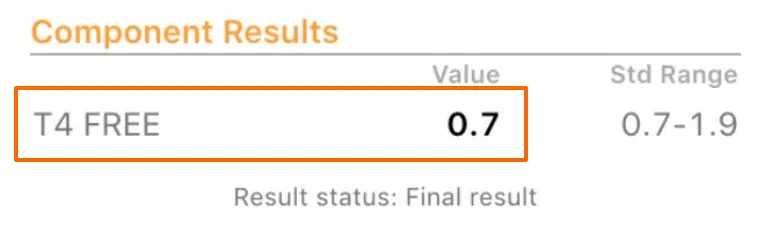
The example above is very common in patients with hypothyroidism who are not already taking thyroid medication.
This TSH represents a “normal” level but certainly a “sub-optimal” level and is most likely consistent with hypothyroidism.
Thyroid Antibodies (TPOab & TGBab)
Checking your thyroid antibodies should also be a necessary part of a complete thyroid panel.
This is important for several reasons:
#1. The presence of these antibodies indicates that a likely autoimmune and inflammatory component may be the underlying cause of your hypothyroidism.
#2. Autoimmune thyroiditis is thought to be the #1 cause of hypothyroidism in the US.
#3. The presence of antibodies indicates a condition that can be treated through lifestyle and dietary changes and alters treatment.
The presence of elevated antibodies (with hypothyroidism) may indicate an autoimmune attack on your thyroid gland.
This is important because, if untreated, may result in thyroidal gland damage over the long term.
The conventional approach is to take a “wait and see” approach.
That basically means waiting until the autoimmune process has caused enough damage to finally alter your TSH to a certain level so as to require thyroid hormone replacement.
Does this sound like a good approach for patients?
Not really.
Instead, it presents an opportunity for significant change to your lifestyle which may (but not necessarily) help reduce the attack on your thyroid gland.
It has been well-established that various factors including environmental triggers (6), viral infections (7), and even stress can trigger, initiate and potentiate autoimmune diseases (8).
Doesn’t it make sense, then, to try and reduce the impact that these factors have on your body?
Of course, it does.
This is why it is important to know if antibodies are elevated in your body!
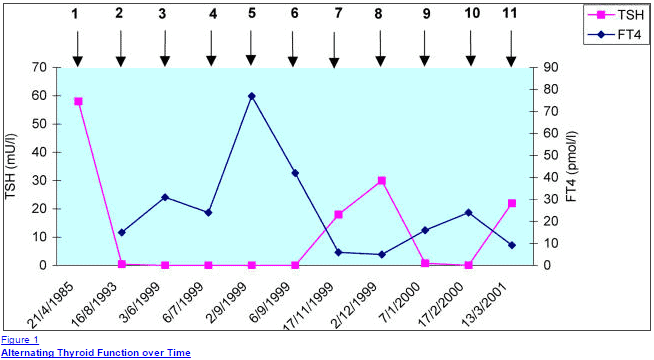
Another important reason to identify if antibodies are present in your body is that your thyroid function tests may change over time due to this issue.
Patients with autoimmune thyroiditis may experience episodic episodes of hyperthyroidism and hypothyroidism and flare-ups which can be confusing if the entire picture isn’t clear.
You can find more information about testing and treating elevated antibodies in this detailed post.
Thyroid antibody normal & Optimal ranges
Testing for thyroid antibodies is relatively easy:
Your antibody levels should be as close to zero as possible.
In most cases the reference range is accurate as in the case below:

The reference range indicates that normal antibody levels should be less than 6.
This patient on the other hand obviously has elevated antibody levels with an actual level of 1317.
This represents an opportunity to make changes to try and lower or change this value.
Sex Hormone Binding Globulin (SHBG)
Sex hormone binding globulin is one of the few tools we have which can attempt to give insight into how your body is absorbing and utilizing thyroid hormone.
Sex hormone-binding globulin is released from your liver in response to two hormones:
#1. Estrogen
#2. Thyroid hormone
Assuming estrogen levels are normal (and assuming you aren’t taking OCP or estradiol) this test can help determine if your liver is assimilating and converting thyroid hormone in your liver.
This information can then be used as a surrogate marker for other peripheral tissue levels of thyroid hormone.
It’s not a perfect test, but it can give further insight into your thyroid function.
In women, an optimal sex hormone-binding globulin is usually in the 70-80 nmol/L range.
In men, this number is usually in the 20-30 nmol/L range.
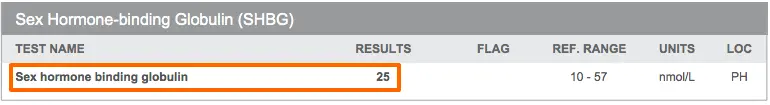
In hypothyroid states (states where tissue levels of thyroid hormone are low) the SHBG will be low.
You can then track the SHBG, which should increase with thyroid hormone replacement, to help determine if your body is converting thyroid hormone appropriately.
Sex hormone binding globulin normal & Optimal ranges
Sex hormone-binding globulin can only be used in certain instances.
If you are taking oral contraceptives or oral estradiol then your sex hormone-binding globulin will be artificially elevated and the absolute value of this test diminishes.
Likewise, the SHBG can be used to determine if your thyroid dose is too high (again assuming estrogen levels are normal).
High SHBG levels may have consequences on other sex hormones in the body, which is one reason you don’t necessarily want abnormally high SHBG levels in the body.
SHBG should be part of the complete thyroid panel but its use is somewhat nuanced.
Final thoughts
Because of emerging trends in thyroid function and an increased understanding of various clinical states that alter peripheral thyroid hormone levels and conversion it’s becoming increasingly important for patients to have a complete thyroid hormone panel.
Beyond obtaining these important tests it is also equally important (if not more important) to understand how these values change or alter treatment.
As a reminder, it’s important to start with these tests to have a complete understanding of thyroid hormone PRIOR to initiating thyroid hormone replacement therapy.
The full thyroid hormone panel includes the following tests: TSH, free T3, free T4, reverse T3, thyroid antibodies, sex hormone binding globulin, and total T3.
Now it’s your turn:
Are you having trouble getting a complete thyroid panel?
Has it helped determine what is happening in your body with your thyroid?
Are you converting thyroid hormone appropriately?
Why or why not?
Leave your comment below!