Are you frustrated with trying to lose weight with your sluggish Thyroid?
In this post, I am going to go “behind the scenes” of what I do inside my clinic and show you how balancing your hormones is the KEY to weight loss success in patients with Hypothyroidism (or any medical condition!).
Note: This is an actual patient from my office, and this is what THIS patient needed for her weight loss. I don’t recommend you use any of the therapies listed below for you personally unless you are evaluated by a Doctor.
Let’s jump in:
This patient presented to me with multiple symptoms and was looking to lose weight and balance her hormones.
She is 69, a mother of 3 kids, and has been struggling with her weight ALL of her life.
Her primary goals of treatment:
- Lose weight (100 pounds ideally)
- Feel better and have more energy
- Improve her sleep
Throughout her life, she tried numerous diets including the HCG diet x3 (she lost 40 pounds the first time, 20 the second, and 10 the last time) and different yo-yo diets throughout the last 20 years…
**Update: Patient now has lost a total of 60 pounds which is 20 pounds lower than what she was able to do with her gastric bypass surgery – more info at the end of the article including testimonial**
- My Thoughts: Chronic yo-yo dieting leads to increased levels of Reverse T3 and Thyroid resistance. It can also lead to Leptin resistance. NEVER do this kind of diet!
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Dieting & How It Affects The Thyroid
Before she came to see me she was most recently seen by another “holistic” provider who put her on a ton of supplements – but she never actually lost weight.
- My Thoughts: Stay clear of providers who only want to put you on a diet or supplements to help you lose weight. Weight loss is a problem with your hormones, NOT calories.
As part of trying to lose weight, she had a lap band surgery, and with the lap band, she was able to lose 40 pounds initially – but eventually plateaued and over the last several years put all of that weight back on + 15 pounds.
Her weight has been a huge source of stress in her life and is taking a toll on both her self-esteem and her health. She has elevated blood pressure, high cholesterol, and diastolic dysfunction stage II.
A brief review of organ systems:
Gastrointestinal tract: She has daily diarrhea – and has for many years (ever since her surgery).
Energy Levels: 4-5 out of 10 on good days. (10 being “optimal” energy levels)
Sleep: Suffers from insomnia, is unable to “slow down her mind” at night, and requires the TV on at all times to fall asleep.
Exercise: She gets on a bike daily for 30-40 minutes
Pain: She suffers from chronic pain in her neck, back, and both knees.
Diet: Consists of Salads every day, very little fat, and high protein in the form of lean meats.
- My Thoughts: Low-fat diets with lots of low-intensity exercises do NOT help with weight loss. For more information, you can see my recommendations on diet and exercise for those with hypothyroidism here.
After our initial consultation, I sent her for a Comprehensive Functional Blood Chemistry Panel, which I will go over below:
Comprehensive Functional Blood Chemistry Analysis
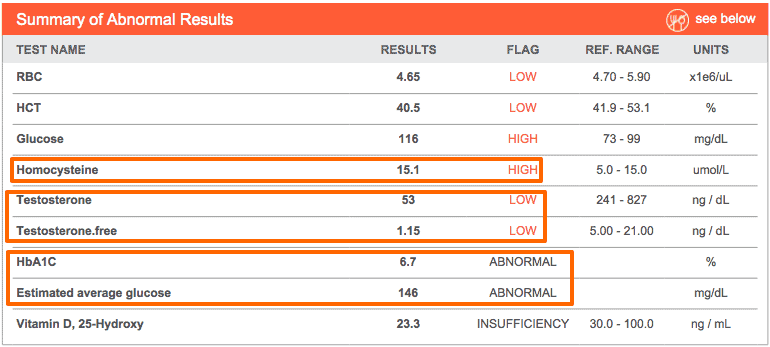
The following labs were “out of range” by the laboratory standards, for the tests that were “in-range” but suboptimal we will go over below (including thyroid studies):
Elevated Homocysteine – An inflammatory marker and high levels are associated with an increased risk of developing heart disease.
Low testosterone – Women need testosterone too! Low levels of testosterone are associated with a depressed mood, inability to lose weight, and inability to create and maintain lean muscle mass (lowers overall metabolism of the body).
Elevated blood sugar – By conventional standards, she falls into the Diabetes range (we will go over this below).
Low Vitamin D – Low levels of Vitamin D make hypothyroidism worse, and low levels are associated with an increased risk of developing autoimmune disease.
Now for going over the more subtle (but probably more important), functional lab tests that are in the “normal range” but still sub-optimal.
Cholesterol
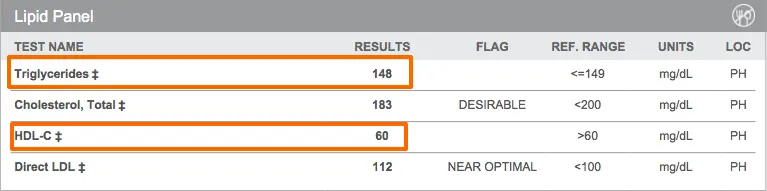
This patient was on a Statin medication (Simvastatin) when she came to see me, which explains her lowish LDL.
In this patient, I’m more interested in her high triglycerides and HDL. This ratio can act as a surrogate marker for insulin resistance (which she does have) and when combined with elevated homocysteine makes me worried about her overall risk of developing heart disease (1).
She is also suffering from Diastolic heart dysfunction and High blood pressure – which can stem from insulin resistance (2).
Luckily these conditions can be reversed VERY quickly – in fact in as little as 1-2 months with intensive diet and exercise routines.
*Note: If a patient doesn’t have a history of heart disease (previous heart attack), the data does not necessarily support the use of Statin medications – Statins have been associated with an increased risk of developing diabetes (3), muscle damage (4), and are associated with an increased risk of developing breast cancer (5).
Blood Sugar and Insulin
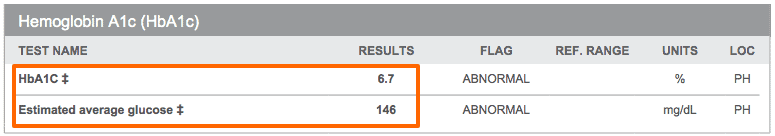
Insulin resistance and blood sugar issues are VERY common in hypothyroid patients.
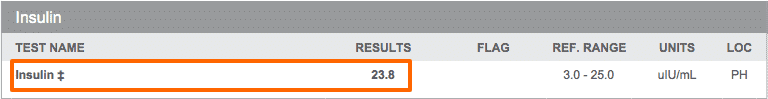
As you can see above this patient has Insulin resistance AND elevated blood sugar which puts her in the range of Type II diabetes mellitus.
Her insulin is also elevated – which is a huge part of the reason she is unable to lose weight.
Recall that with high levels of insulin (I use 5 as a cutoff) your body will store all calories you consume as FAT. Insulin literally turns off the enzymes in your body that allow you to burn fat as an energy source.
In this patient, a FASTING (12-hour) insulin level of 23.8 will be a huge issue for her and explains her inability to lose weight – especially when combined with her other hormonal imbalances.
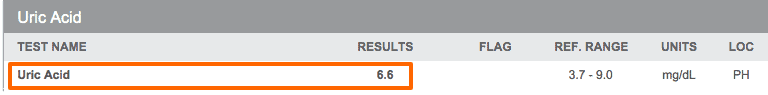
As you can see her Uric acid is also elevated – this tells me that her liver has a problem metabolizing fructose (6) and that she is likely consuming extra sugar in her diet.
Thyroid Studies
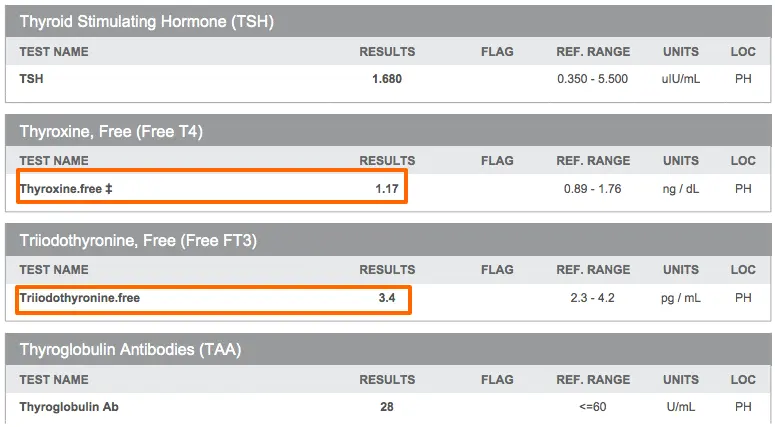

These thyroid studies definitely fall within the “normal” range by the definition of the labs.
Despite that, this patient suffers from multiple hypothyroid symptoms and also has several other signs of hypothyroidism including low resting pulse, decreased body temperature, and symptoms of hypothyroidism.
Because of these findings and because insulin resistance is associated with low levels of T3 in the serum (7) and a hypothyroid state – I treated her with thyroid hormone.
As you can also see, her free T4 and free T3 levels are suboptimal – both falling within the lower first and second quartile of the reference range.
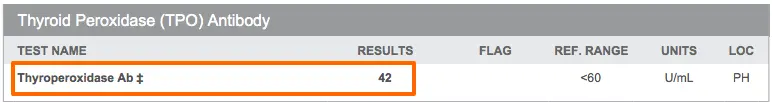
In addition, her Reverse T3 is elevated which is causing an inappropriately increased free T3 level (8).
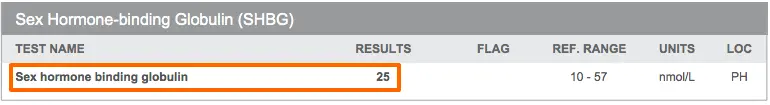
In tricky cases, you can also look to Sex Hormone Binding Globulin to assess liver tissue levels of thyroid hormone.
Low SHBG is associated with tissue-level hypothyroidism, and tracking SHBG levels (9) with treatment can be used to get an idea of how much Thyroid Hormone is actually getting to the target tissues.
In this case, you can see that low levels of SHBG are consistent with tissue-level hypothyroidism and high levels of reverse T3.
Note: It’s unclear to me whether her insulin resistance caused her hypothyroidism or if her hypothyroidism contributed to her insulin resistance – but in either event, both need to be treated!
Iron Studies
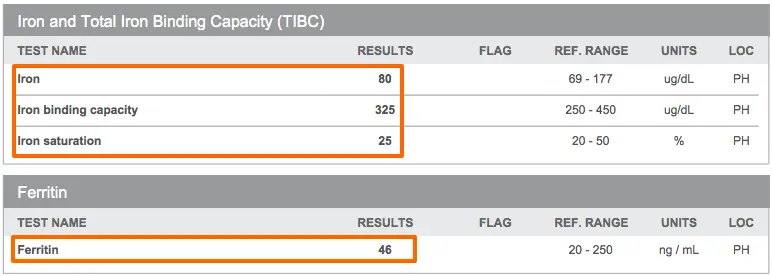
Iron is critical to measure because low levels are associated with decreased thyroid function (10).
In this patient, you can see that her levels are “normal” but they all fall within the lower portion of the reference range.
Through treating hundreds of patients I’ve found that optimal thyroid function happens when Ferritin is around the 70-80 range.
Vitamin B12
Vitamin B12 deficiency (11) is a BIG deal and often missed by many providers who aren’t looking for it.
Absorption of B12 is dependent upon hydrochloric acid, and with hypothyroidism, stomach acid is generally low – this results in decreased absorption of Vitamin B12 in many hypothyroid patients.
In addition – subclinical vitamin B12 deficiency is VERY common (12) and often undiagnosed.
Because of this, I treat patients with vitamin B12 if they have: Low or mid-range serum B12 levels, an MCV > 92 on red cell analysis, or elevated homocysteine levels.
This patient has several of these lab values so I opted to treat with methylcobalamin injections to saturate the tissues with B12.
Diagnoses
After going over the results with her above, and assessing her symptoms she ended up with the following diagnoses:
- Thyroid Resistance, Hypothyroidism
- Insulin Resistance, Type II Diabetes Mellitus
- Low Testosterone
- Adrenal Fatigue
- Insomnia
- Diastolic Heart Disease
- Iron Deficiency
- Chronic Diarrhea, with multiple nutrient deficiencies
- Vitamin B12 Deficiency
- Vitamin D Deficiency
- Hyperlipidemia
- Hypertension
As a side note:
Don’t let this list of symptoms and diagnoses scare you.
These are just names of her conditions, what we really care about is WHY.
In this case, my suspicion is that something like this occurred:
Her history of multiple episodes of recurrent yo-yo dieting led to her thyroid resistance. In an attempt to lose weight, her gastric bypass likely led to malabsorption of iron and B12 with chronic diarrhea, further worsening her hypothyroidism.

Her insulin resistance and Hypothyroidism are likely contributing to her high blood pressure and abnormal cholesterol panel.
High levels of stress lead to adrenal fatigue and symptoms of insomnia, extreme fatigue, and food cravings.
Following this logic, our treatment should be aimed at reversing these conditions (which I will go over below)…
Treatment
Here I will go over the treatment that this particular patient needed, and then give some follow-up thoughts on why I did what I did.
Please remember that this treatment is specific for THIS patient!
Do not take any treatment recommendations and apply them to your health. Every patient needs to be treated differently because no two patients are alike.
How to use Functional Medicine for Optimal Treatment:
Hormones and Medications:
In her case, I replaced hormones that were identified as being suboptimal with her blood work:
- Armour Thyroid
- Bio-identical Testosterone (In an organic base)
- Phentermine (To be used with fasting protocol)
Even though it is likely that her thyroid and testosterone are both low due to insulin resistance, I still prefer to treat patients in this position because they will often get faster results and will feel better quicker.
My goal is to always reduce medications whenever possible, so if her hormones balance out after treatment I will attempt to decrease her dosing of these medications.
Because of her age and symptoms, I started with 30mg of Armour Thyroid (She is currently on 60mg and doing well).
Supplements:
Her supplements were targeted to her comprehensive functional chemistry panel:
- Zinc + Selenium to boost thyroid conversion, 2 capsules daily
- Vitamin B12 injections once per week x10 weeks (Methylcobalamin)
- Vitamin D3 10,000 IU per day
- Adrenal Support, 2 capsules twice per day
- Liquid Iron 1 Tsp per day
- High potency probiotic 1 sachet per day
To learn more about what supplements I use and why I use them I encourage you to check out this post here.
Most of these supplements were targeted at specific deficiencies in the blood work, the only exception being adrenal support.
The probiotic was used to help balance out intestinal dysbiosis from the gastric band and chronic diarrhea.
Physical Work:
This patient had significant pain and multiple tender points along her neck, mid back, and lower back.
My suspicion is that these tender points were potentiated by low levels of thyroid hormone.
Because of this, I recommended soft tissue physical manipulation and low-intensity vibration therapy on a weekly basis, in addition to cranial sacral work.
Fasting Routine:
Elevated insulin levels (especially in the fasted state) contribute to weight loss resistance.
Unfortunately, fasting can be tricky in patients with Hypothyroidism. Especially when most Hypothyroid patients also suffer from adrenal fatigue.

As you can see below she dropped her fasting insulin from 23.8 (12-hour fast) to 10.3 (24-hour fast).
Our goal is to get insulin levels below 5 but each time her body drops her insulin level it will become more sensitive and subsequent fasting episodes will further drop her insulin level.
Before and after each fast I checked her percent fat mass, muscle mass, and water weight.
Stress Management:
Emotional and Stress reduction therapies are critical to managing both weight loss and overall health.
This patient had a history of being unable to sleep due to her mind being constantly “turned on” at night.
Because of this, I had her practice a combination of biofeedback, mindfulness, and guided meditation to lower stress levels and help her sleep.
This therapy was done in the office.
Dietary changes:
Diet is critical to weight loss, but by itself isn’t always enough.
In this case, I started the patient off on a gluten-free, dairy-free, soy-free, and sugar-free diet.
Her diet was high in healthy fats, nutrient-dense, and filled with real whole food.
She met with my health coach/nutritionist weekly to help her integrate new food groups and menu plans into her daily life.
Exercise:
Due to her untreated hypothyroidism and adrenal fatigue, I started her off on low-intensity exercise.
After 1 month I started her on HIIT – in the form of 10-15 minute bursts once per week.
Detox:
Many hypothyroid patients need to eliminate endocrine disruptors from their bodies in order to improve their thyroid function.
In addition, as the body starts to burn fat stores for energy, the fat cells can dump excess fat-soluble toxic compounds into the body.
This is especially important during fasting routines when the body burns TONS of fat for energy.
I had this patient do weekly FAR infrared sauna therapy for several reasons:
- Activate heat shock (13) proteins in the liver for detoxification
- Help the body burn extra calories (14) for weight loss
- Help eliminate toxins through sweating
- And help the body relax by reducing cortisol levels (15)
Results
In using this multi-faceted functional medicine approach to care, the results can be very impressive.
This patient was able to improve almost ALL of her symptoms within 1 month of treatment – which I will go over below:
Weight loss:
*Note: Weight loss is measured in percent fat mass lost by impedance analysis of the body. Note that the total weight did drop more than just percent fat mass, but I consider this a more accurate measure (along with body measurements) of fat loss.
Week 1 – 5 pounds of fat mass lost
Week 2 – 7 pounds of fat mass lost
Week 3 – 4 pounds of fat mass lost
Week 4 – 5 pounds of fat mass lost
Total lost over 1 month of treatment: 21 pounds of fat mass
This weight was lost without losing any muscle mass and without persistent calorie restriction.
Insomnia:
By the end of week 2, this patient was sleeping a full 8 hours through the night and was able to sleep without turning on her TV at night for background noise.
In her case, I believe her insomnia was due to a combination of adrenal fatigue and some degree of undiagnosed anxiety.
Both were improved with hormone balancing, supplements, mindfulness, and physical work.
Energy:
Current Energy levels = 8/10, an increase from 4-5/10
Energy levels are subjective but can be used as a general “marker” for how well her thyroid and adrenals are functioning.
Chronic pain:
At the end of 4 weeks of treatment, her pain had almost completely resolved, and at this point, she no longer has back pain.
In this patient, I believe her pain was due to her elevated insulin levels and anatomical changes which were dealt with by physical work and a fasting regimen.
Final Thoughts
This patient is still undergoing treatment with me, and I will continue to update her results from time to time.
At this point, I believe she will continue to lose fat mass and improve her energy over the next 4-6 months.
I wanted to use this patient as an example to show what a comprehensive, functional medicine approach to care actually looks like.
Many people are stuck in the conventional medicine mentality and they wrongly believe that changing up their medication from Synthroid to Armour thyroid will solve all of their health problems.
This couldn’t be further from the truth.
In many cases switching medication will help symptoms, but it won’t be enough by itself.
Whenever possible your doctor should attempt to go after the primary cause of your symptoms and reverse that.
Updates:
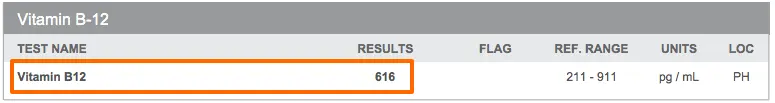
The patient is now down a total of 60 pounds (20 lower than she was able to achieve after her gastric bypass) continuing her fasting protocol and adding in a GLP-1 agonist for her leptin resistance.
Her weight loss plateaued at around 50 pounds of weight loss, so we checked her leptin level:
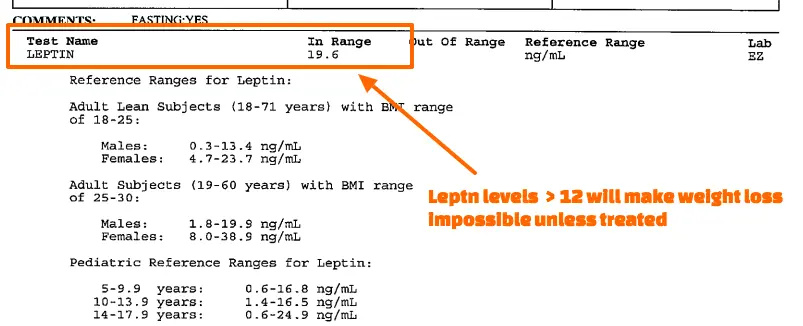
You can see from the above that her leptin levels are > 12 indicating that she has leptin resistance.
Even though she was able to lose weight initially this was the cause of the plateau at around 50 pounds.
After adding a GLP-1 agonist to her regimen she was able to lose another 10 pounds total.
You can find her review and testimonial below:
I want to hear from you!
What kind of treatment have you received for your thyroid? What worked and what didn’t? Is your doctor using a similar approach to treat you?
Let me know in the comments below!
Scientific References
#1. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2664115/
#2. http://www.ncbi.nlm.nih.gov/pubmed/7512468
#3. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4118294/
#4. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2849981/
#5. http://www.ncbi.nlm.nih.gov/pubmed/23833125
#6. http://diabetes.diabetesjournals.org/content/62/10/3307.full
#7. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3647563/
#8. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1628409/
#9. http://www.ncbi.nlm.nih.gov/pubmed/1618999
#10. http://www.ncbi.nlm.nih.gov/pubmed/16500878
#11. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3257642/
#12. http://www.ncbi.nlm.nih.gov/pubmed/16537043
#13. http://www.ncbi.nlm.nih.gov/pubmed/11741035
#14. http://jama.jamanetwork.com/article.aspx?articleid=360118
#15. http://www.ncbi.nlm.nih.gov/pubmed/3788622




I’ve had Hashimotos for at least 2 years but only just been put into Levothyroxine about a year ago as my doc said my levels were “normal” which turned out I had Hashimotos I have gained at least 20lbs my hair is falling out, my joints are in agony and I’m physically exhausted most of the time! Please could you help ?I’m so unhappy feeling so uncomfortable all the time, I feel this is affecting my quality of life, many thanks j Wingate
Hey Joanne,
I’m sorry to hear about your situation – unfortunately it isn’t that uncommon nowadays. The best advice I can give is to look for a functional medicine doctor close to you (you may have to travel to one) to help put you on the right path.
It sounds like you may benefit from adding T3 to your regimen in some form, but realize that this is just a small piece of a larger puzzle.
Dr.childs so when you put your patient on a gluten free sit free dairy free diet and was sent to a nutrionlist was she following her macros ? Im 5’9 30% BF and 180 pounds. I’m just wondering since I am on the same diet I was out on levothyroxjne 75mg started to loose the weight was down from 180 to 175 in 3 months but weight gain came back. She added a t3 supplement to my regimen and seems to be working. I’m eating twice a day at 800 calories and doing HIIT everyday. Should I be following my macros which come out to be 1600 calories! I’m just scared to eat that much since I have a slower metabolism, but I no it’s important to eat what your body needs , as well as lifting I just don’t want to end up loosing fat and still being big. My goal is to be 150 What are you
So what’s one to do? I have a doctor’s appt next week and I will ask to change my prescription to Armour, but then what? I don’t have the energy to educate my doctor. And I shouldn’t have to. I am willing to take the supplements you outlined but what if i need further tests? I guess I will have to wait and see what he says.
Hey Jennifer,
Each person is unique and needs to be evaluated based on their personal history and treatment should be targeted to their lab tests and symptoms. I can’t say for sure what tests or treatment you would need. I would also point out that changing to armour is only a small part of the equation for some people (not even everyone needs it or does well on it), the rest is going after your specific hormonal imbalances and treating those.
In general, you will find the most help in seeking out a doctor that practices functional medicine.
Hi! I had hypothyroid since 1991 two years ago í moved to the border of texas and when ivstart seeing a de. Here he took my levothyroxin away he said It was normal . í went to other doctors and they said since í do not have a record here in the valley.So they wont give me meds for my thyroid. I feel really fatigue, gain alot of wait, cold and in pain. What should I do? Please help
Hey Maria,
The first step is to get properly diagnosed with the right tests. You can find out what tests to ask your doctor to order here: http://www.restartmed.com/68-of-the-most-commonly-reported-signs-and-symptoms-of-hypothyroidism/
If your weight problem is primarily related to your thyroid then you should have improvement in your symptoms. If it’s not, then you will need more advanced testing. Most likely if you need further testing and treatment you will need to see a specialist to help you.
My doctor told me to go on slimming world diet and just up’d my thyroid tablet to 150.
Hey Claire,
Increasing your thyroid hormone is a good place to start, but you can’t ignore all of the other hormones that may be interfering with your weight loss! Make sure to get properly evaluated and have your other hormones checked as well.
Hi Dr. Childs,
Do you pay much attention to the TSH test? I used to see a doctor (who is now retired) and he and I agreed that if you are taking thyroid medication your TSH will likely be suppressed. Why would your body tell your thyroid gland to make more thyroid if you are giving your body thyroid with medication daily? I can’t seem to find another doctor who shares the same view. I’m more concerned with it being too low than too high because everyone thinks you’re HYPERthyroid when the TSH is low even with many obvious hypothyroid symptoms. What are your thoughts on TSH and do you think there is an optimal range for it?
Hey Nicole,
Taking thyroid medication (T4 or T3) will ALWAYS decrease the TSH. The reason is because the pituitary is the most sensitive tissue in your body to thyroid hormone because it has special deiodinases which do NOT create reverse T3 which compete for free T3 binding. As a result using the TSH to measure peripheral tissues for thyroid hormone is horribly inaccurate. I will order the TSH as part of the picture, but I employ a host of other tactics including resting heart rate, resting pulse, subjective symptoms, and a complete thyroid panel when diagnosing and hypothyroid patients.
I will write a post about your question, because it is far too complicated to get into in the comments section here – but after monitoring hundreds (if not thousands) of patients on thyroid medication and watching the TSH I’ve found that thyroid blood tests in general do not always give a clear picture on what is happening in the body.
You are not likely to find Doctors who share my view (or the view of your previous Doctor) because it differs from the standard of care. It’s far easier to order the TSH and call it “normal” and kick the patient out of your office than it is to do what I do.
Great question, though!
Hi Dr. Childs,
I’m so glad I stumbled across your website. I was recently diagnosed with Hasimoto’s disease. I have gained about 40 lbs in the past year with constant fatigue. My synthroid was increase to 150mcg a day for 3 days a week and 300mcg a day for the other 4. I still feel awful. I have tried to get the doctor I see prescribe Armour Thyroid but they are sticking to Synthroid. I have been dealing with thyroid issues since my early twenties and now I’m 36 and 225 lbs. I’m only 5’4″. I just want to feel good again! HELP!
Hey Katie,
The best thing you can do for yourself is to find a Doctor who is willing to work with you. I do online consultations for this reason, but if you can’t do that then search around your area for someone local!
Hello Dr. Childs,
You have a good site here and I appreciate your work. Thank you so much. 🙂
I am seeking more direction and info because I feel I have a sub clinical thyroid condition even though I have been addressing my health for the last over 3 years. I have studied non stop for 3 years about health and my conditions and follow Dr. Ron Rosedale and Dr. Richard Bernstein who recommend low carb high fat diets to correct Leptin and insulin resistance and diabetes, with good result. I was pre-diabetic and morbidly obese with extreme insulin resistance. Blood pressures up and arthritis.
I have been following a low carb high fat whole foods diet and eliminated all grains and starches. I eat very healthy and well. I make my own pro-biotic sauerkraut and take organic turmeric daily for inflammation, bone broth, organic and clean food. I managed to lose 90 lbs in 3 years. At Christmas I took a fall and blacked my eye badly, ( my first shiner), found out I had a heart condition ( no intervention required as it turns out) and suffered a personal setback. I ate a bunch of bad juju and because of my insulin resistance put 20 lbs back on instantly. I need to lose more than that. Now I am back to eating low carb, 30-50 grams per day and not losing or gaining.
My thyroid labs are normal per my doc but I am have dry skin,a little hair loss, cold hands and feet and plummeting body temps. Using a basal thermometer I check when I am cold. Yesterday it was at 96.54 at my coldest.
I am so energy-less I feel like crying/dying because I have so many projects and no energy to do them. I am a massage therapist and have no motivation due to tiredness. I have little stress and know how to manage that at least. ( Yin person. :-)I need to make money. Yesterday I barely got through a massage and was perspiring profusely and weak in my muscles. Hadn’t eaten for about 4 hrs., possible Keto flu…
Chris Kressor says a very low carb diet causes low T3 conversion to T4. He recommends 150 carbs. If I eat that I can’t lose weight either because of leptin and insulin resistance. I have a clear understanding of those. Makes sense that my body seems to have down-regulated more due to this diet but my blood sugars and pressure are awesome compared to what they were as long as I don’t eat sugar. If I do they both shoot up drastically almost instantly and I feel like DEATH! My energy levels and body temp were better before I began the diet.
Recent thyroid labs were all in the normal mid range. I did not have a RT3 done. My insurance won’t pay.
What’s scary is sudden plummeting of the body temp and energy. It does come back up if I eat/ rest and relax for awhile.
I am in good general health other than a screwed up metabolism which I am trying to repair.
No stomach issues, digest well, a bit of constipation which sometimes goes with this diet but offset with coconut oil, food enzymes, psyllium, lots of fluids.
One day this month I had energy that I hadn’t seen in forever and chortled all day long to everyone I met!! I was joyous! And I probably did too much.) All that day I felt normal. 🙁
I take a full range of supplements including Berberine and Selenium, Zinc, Vitamon D3, K2 etc.
I must take Cocoa Well to get fake caffeine energy, 146 mgs. if I have to do a lot in a day just to get through.
Some advice says cook all veg, and get off dairy which will be hard but I am prepared to do if necessary. I tolerate it well and love it but I am willing.
Please advise me on these points when you can.
I appreciate any advice you can give.
A healer trying to heal myself.
Gratefully,
Susan
Hey Susan,
I don’t know how much else you can actually do on your own without the addition of bioidentical hormones. It would be helpful for you to take thyroid medication (preferably T3) and a leptin sensitizer to get your body back on track. The last thing you could try is fasting, but I’m not sure I would recommend it without addressing your thyroid first.
I have been seeing a Holistic doctor for about 5 years, he dx’d me with hyperthyroidism and adrenal fatigue. The doctor put me on a compound of c-t3/t4 1:4 75mcg caps he also had me take Homocysteine Supreme, Dr. Wilsons Super Adrenal Stress Formula, Adrenal DMG, Grapeseed, Fish oil. I have had alot of test over those 5 years and the doctor said I have high histomine levels and that I am at an incressed risk for a heart attack, he alos had me on a hormone replacement compounded for me and used vaginaly. Never got optimal results, never had weight loss after being faithfull to WW for a year and a half. He took me off the hormone replacement when I told him I didn’t want to do another expensive saliva test. I went to my GP and he said he would take over my thyroid disease and put me on synthroid 75MCG tab, I am shakey,not sleeping, and irritable. I checked my resting pulse it was 84, but my axiallary temp was 96.7. I have gained 3 pounds in 2 weeks with incressed activity and continued diet. I feel like stopping everything. PLEASE help.
Hey Nancy,
It sounds like you need someone to manage your thyroid hormone replacement. Going off of all of your hormones is not likely to help and it doesn’t matter how much you exercise or diet if your hormones are off – you will continue to gain weight.
Dr. Childs,
This is fantastic info. I’m 34 yrs old and have hypothyroidism. I’ve been on Nature Throid and more recently Armour Thyroid and have optimal levels on full Thyroid panel. I’ve had a sonogram done on my neck as it seems to be very swollen and they mentioned it was very thick, possibly hashimitos. However, the tests came back normal (I’ve been on meds for years). Not sure if this could be related, but I feel I might actually have hashi’s because I’ve also broken out in shingles 3 times within the past year and I’m very healthy. The docs ALWAYS ask if I have an autoimmune disorder.
I cannot seem to lose a pound and take CrosFit workouts 4 times a week with a healthy diet. I also have zero sex drive. I wonder if I might need an additional hormones to assist?
Thanks! You seem to be VERY educated on this!
Hey Wendy,
Yes, you most likely do have hormonal issues or you’re under treated. The hard part is finding a doctor to help you figure out what is going on and how to fix it.
My story is JUST like your patient. FINALLY. A gastric bypass patient who had trouble losing weight!! I had a gastric bypass surgery (RNY) in January of 2008. Back then, I couldn’t find evidence of anyone like me.
I lost 60 pounds within 6 months and then *POOF* nothing. Everyone kept telling me it’s “just a plateau”. I exercised more, ate less. I drank more water, changed the type of exercises, more fruit, less fruit, less carb, more carb, more protein, different types of protein . . . on and on and on.
I went back to my endo, back to doctors. No one could tell me anything, including the doctors who coordinated my surgery. The only thing that showed up abnormal in THEIR tests was my Vitamin D. I point-blank asked if that could stop me from losing weight. “No” was the answer.
It was devastating to go to the doctor to get help and be treated as if you’re lying about what you’re eating. Pray tell: if you go to the doctor, aren’t you supposed to tell them what’s wrong? And guess what? If they don’t believe you, YOU CAN’T GET HELP. The shame I would feel when a doctor’s mouth would fall open at the words, “I had gastric bypass and can’t lose weight.” I could only affect my weight if I ate less than 1000 calories. But I knew it was only water – not fat. And my thought was, “If I’m 235 pounds right now, how in the world am I going to lose another 65 pounds if I plateau again? I can’t go lower STILL!”
The doctor who initially authorized my surgery thought he knew my motives for seeing him and thought he would preempt it by telling me, “You can’t have a revision.” He didn’t know what to say when I told him, “I don’t WANT a revision. I want the surgery I HAD to WORK.”
I went back to my surgeon 2-3 times, went to several endos, all within my HMO. I drove 45 minutes in Los Angeles traffic to see one endo, only to cry all the way home. My tests always said I was normal. They flat-out said they didn’t know why I couldn’t lose weight. And I couldn’t find any testimonials online of any RNY patients who were having the same difficulty I did. Maybe I was stressing my body? Maybe I needed a break? All I DID know was that I was regretting the decision to have the surgery.
I am 44 years old and have been overweight ALL my life. I don’t remember what it’s like to be thin. Having surgery and not being able to lose the weight felt like a cruel joke. Before the surgery, my body worked but I didn’t have the motivation. Now I had all the motivation in the world, and nothing I did would get the weight off.
So for the last 8 years, I have had a cycle of give up, start again — over and over. Weight loss is hard enough as it is. If it was easy, I wouldn’t have had the surgery. But to be doing all the right things AND get no results is maddening. I’d get tired of being fat and somehow gather up the courage to try again. I’d tell myself I just didn’t stay consistent long enough the last time. All the while I’m making the decision to start again, I’m scared that I still won’t get any results.
I am currently 276-281 pounds. I started a lifestyle change (again) on July 28. I was all in. I went out and bought free weights, a weight machine and a treadmill. I have exercised 5x per week faithfully since that time, except for the week I was sick. I’ve dropped my calories to 1/2 of what I was eating before, cutting sugar, cutting carbs, cutting even artificial sweeteners, eating salads, increasing protein, tracking it all on FitnessPal.com. The result: all I did was yo-yo back and forth between the SAME 5-6 pounds. I can gain fat, but I can’t lose it. I can’t get below 276.5.
That kind of drastic change in my lifestyle should produce a change! Weight fluctuates daily, but there should be a downward trend. There isn’t one. I also measure with a tape measure regularly, so it’s not like the scale is going up but my inches are coming down. Not so. No inches lost. In three months. I’m not burning fat. As I’ve been trying to tell my HMO doctors – something is WRONG.
A ferritin test hasn’t been run on me since 2009. I asked for a Free T3 test several years ago and was told that Kaiser “doesn’t run that test.” I was prescribed 50,000 ius of Vitamin D2 for my low vitamin D – instead of Vitamin D3. And the ONLY reason they ran a Vitamin D test was because I ended up having to call Member Services and submit a grievance when my doctor refused to run one. Her reason? She said she didn’t know how to read it.
I understand that weight loss isn’t supposed to be easy. I’ve lost weight enough times to know that. I’m not looking for a miracle. I know that 1-2 pounds a week is reasonable. But what weight loss ISN’T supposed to be, is impossible. I, doctor, am living in the realm of the impossible. After 8 years, I know that for sure now. It’s like trying to run a marathon with your leg chained to a tree. No matter how hard I run, I’m not going anywhere. It’s not about me or my habits or my effort. It’s about my body – the “tree”.
I am usually a very driven person. In the last two years, I have struggled with a lack of motivation. I have described it to my husband as “feeling weary on the inside”. I sweat a lot in my sleep, but maybe that’s menopausal. I can, however, go to sleep any time I sit down long enough. At about 7-8 p.m., I’m DONE for the day. And it’s very hard to get up in the mornings.
I’ve told myself, “If I just make myself exercise, I’ll have the energy I need. Maybe I’m to blame for how I feel.” But, as you exercise, your fitness level is supposed to get higher, and you should be able to do more as your body gets lighter. I’m not getting any lighter, so I’m stuck at 20 minutes. Because I am not burning fat, I can’t get past doing more than 20 minutes.
I looked at the lab ranges in your article above and was SHOCKED.
Her RBC was considered low at 4.65. Mine was lower than hers — 4.41 on 3/12/16. Her lab’s range was 4.70-5.90. The Kaiser range is 4.20-5.40.
Her HCT was considered low at 40.5. Mine was lower than hers — 39.1 on 3/12/16. Her lab’s range was 41.9-53.1. The Kaiser range is 37-47.
The point: as long as I continue going to Kaiser on this matter, they’re never going to say there’s anything wrong with me. But I don’t even know where to start to get help . . . what kind of doctor to see? What to ask for? Kaiser isn’t going to cover it. If I’m going to get help, I’m going to have to pay for it myself. I’ve been trapped for eight years, so I’ve finally conceded that this is the ONLY way I can get help.
Hey Sheryl,
You are right that you will most likely have to seek care outside of the insurance model. No matter how hard you try, or how many tests you ask for, you won’t be able to make a Doctor treat you a certain way and in the end that is all that matters.
Hey, found this article very interesting. Especially the mention of leptin levels as my Doctor has never mentioned this.
I was diagnosed with hypothyroidism in 2013, after my initial diagnosis I managed to lose 42lbs in weight. I felt great.
However….. my weightloss has hit a huge plateau. I’m now stuck at 215lbs and nothing is shifting the weight! I actually work as an exercise therapist, so I know my levels of exercise are what you would usually prescribe for fat loss. This makes me even more frustrated!!
I would like to lose another 20lbs or so, so any advice you could give me would be great.
I’m currently trying the 16:8 intermittant fasting ‘diet’ but after 2 weeks of this i’ve seen no change. Exercise wise i’m completing 4 20min HIIT workouts per week, plus a 5k run.
I’m currently on 175mg of Levothyroxine a day.
Any advice would be gratefully recieved.
Hey Mark,
You will need to have the following levels tested: insulin, leptin, testosterone (free and total), reverse T3.
No amount of exercise will help you lose anymore weight until those hormones are addressed above. I wouldn’t waste time getting them checked by your PCP or endo either, they won’t really know what to do with the results.
Hi,
What is the fasting protocol you put her on and for what reason? You mentioned it in the post but didn’t go into detail. Is water fasting harmful if you have hypothyroidism?
Also, do you offer online or phone consultations. I live in canada but I would love to do blood tests and discuss them with you as I have yet to meet a doctor that is as informative as you. We have free healthcare, but I would still rather pay and discuss effective solutions with you.
Hi Bianca,
I go into detail about fasting including how to use it, how long you should use it, how to tell if your body is ready, etc. in my weight loss guide here: https://www.restartmed.com/hormone-mastery/
There is also an option for a consult in a premium package if you think that is something you would benefit from.
Do you have an option for only s consultation? Without the other stuff. I am on Keto and do Orangetheory theory hit 3-4 times a week. I’m mainly only interested in discussing my hormones after I get the results and what I should do moving forward to get it back on track.
Are there specific things you suggest I get test results for before having a consult with you?
I plan on requesting thyroid panel, insulin tests, estrogen, adrenals, cortiosol, selenium & iodine ( I feel like there’s a good chance I am deficient in these which could be one of the reasons for my thyroid issues).
Hi Bianca,
At this time I only have a 30 minute phone option which you can learn more about here: https://www.restartmed.com/hormone-mastery/
I also notice you considered her b12 deficient even though her blood test showed up as pretty high. Why is that?
Hi Bianca,
Serum B12 levels are notoriously inaccurate at establishing cellular B12 concentration. You can use other serum markers to assess cellular B12 concentration like MCV, homocysteine or MMA. Most people are B12 deficient even if their serum B12 level shows up as “normal”.
Hello Dr Childs. I know this is a stretch but are you willing to take patience via-skype? In 2014 i had extensive test ran that was $8000 worth, praise God for Insurance. After all the testing I found out I have a lot of food allergies, hypothyroidism, estrogen dominance, low progesterone, MTHFR gene which I was never explained about. Several other things on my lab results that are in question since I was never given an explanation for. The day I was there to receive my lab results they were running an hour behind. My visit was cut short and sweet. Afterwards I found out the practitioner I was seeing was leaving that practice. So I fell in the cracks. The next practitioner continue running labs with no results nor help even to the point of lowering my Thyroid dosage. All the while having a low grade temp of 96.6 which was never discussed with me and how that connects with your thyroid. Yea this is a holistic practitioner I was seeing. After all this with no results of improving I began to take my health in my own hands. However, after reading your information above. I know I need to take some lab testing. I am just exhausted and fearful of looking for another Dr only to be strung along and not helped.
Hi;
It sounds like you do amazing work and actually interpret test results instead of just going through the motions!! Kudos to you!! I have had a thyroid issue since I was 26 (I am currently 52). It started as over-active thyroid, which the doctor at the time treated with a Radio-Iodine treatment, which, as you know, killed my thyroid completely. He then treated me for hypothyroidism and for years I was on Levothyroxine, and felt terrible. After many years I switched doctors and the first thing my new doc did was put me on Synthroid, which did improve my energy level a bit, but never resolved my thinning hair, constipation or feeling cold all the time. I was also severely overweight (over 300 lbs), was pre-diabetic and showed signs of insulin resistance.
About 15 months ago, I joined Nutrisystem and since then have lost 115 lbs. I feel better, my A1C went from 5.9 to 5.4 and my blood sugar went from 116 to 78. I also exercise 3-4 times a week, walking/running on a treadmill. Recently (within the past month), my weight has plateaued and I still have constipation (unless I take Senna), thin hair and feel cold all the time. What would you recommend?
Hi Dr. Childs! Just wanted you to know how much your postings are helping me unscramble the issue of sub-clinical hypo and IR. … and believe it or not, my HORSES, who have been battling the same for years. SO.. Many Thanks as I love them so much! For me at age 60 it has been lifelong, with menopause being the catalyst which threw me over the edge. I am better but still not there and recently was put on a tiny dose of Naturethroid by FM doc which seems to be helping a little. We are starting slow since I have gastritis and don’t want to increase stomach acid too quickly. Clearly digestion and dysbiosis is a big part of the picture. RT3 was 16 (range 9-24) but don’t have rest of the labs yet although TSH had been climbing since 1/2 thyroid removal a few years ago (adenoma, not cancer… WHAT A WASTE, UGH) Meanwhile much of what you suggest here has helped my horses immensely.! My piggy little boy was being starved to death with vet saying I was feeding him too much (I was NOT but this is classic response in vet and human medicine). He was gaining out of control. When I INCREASED his feed to a normal amount he started dropping weight like a hot rock. In doing so he was also getting more of the CRITICAL nutrients ZINC, SE, and Iodine. Same for me as I was always starving myself to try to loose weight. With your helping me understand things better I hope to have us all on track eventually. I have changed my own probiotic and have added one for them, and can see signs of inflammation (swellings and curliness of mane and tail) going away slowly. Using spirulina and will add Milk Thistle, and already using TMG for liver support for us all. There is no placebo effect for them, so I hope this post will encourage others to keep on fighting! There is a way out of this! Hugs to you for caring for those of us who know it is not all in our head, LOL! Kim C 🙂
Thank you for posting such insightful and detailed articles. I found this particular one through a link in one of your posts about contributors of increased testosterone levels. I started researching this due to adult acne along my jawline and higher than normal glucose levels. I have a family history of diabetes and want to ensure my body chemistry and levels are healthy (correct the why). I live in Denver CO. Are there any physicians you could refer me to who are as passionate about the topic as yourself?
-Thank you!
Hi, Dr. Child’s,
Thank you so much for the article. I read it along with my recent lab work to help translate it into terms I could understand. Turns out my ferritin is low so I will talk to my doctor about iron supplements (there is a family history of hemochromatosis so I will see how that corresponds).
My main question about this patient is the use of Phentermine and it’s long-term safety. My doctor recommended this years ago and I have used it at different times and had great results but was ultimately taken off due to pregnancy. Each time I went off, any weight I lost was immediately regained plus 20 pounds with no diet or exercise change (which I attributed to the significant decrease of energy levels and increased appetite which the phentermine previously addressed).
Are there alternatives to Phentermine that you would recommend and was this patient able to wean off and not regain the lost weight?
Thank you!
Thank you for the wealth of information you provide…I feel like I have been looking for someone like you all my life. I am listening and rereading your material over and over to educate myself on how to get my weight under control. Like your patient in this post, I’m older…I am a 65-year-old woman who has struggled with weight issues all my life. I have tried all kinds of diets, fasting, gastric bubble back in the 80’s, lapband in 2004, which resulted in no weight loss and had it removed, with horrible complications in 2006. Nothing has resulted in any lasting success.
I actually learned I had hypothyroidism when I was diagnosed with uterine cancer in 2016. I did not have insurance and resolved my cancer with holistic methods (after my tumor markers were normal, I opted to have a hysterectomy). This year I finally got on Medicare and was able to seek further assistance with the thyroid issue. My TSH is 12.260, my Free T4 is .90 (those are the only two test that was ordered at the time), I am told I’m prediabetic, low vitamin D and B12 (even though I have been taking them for some time) and I have the signs of adrenal fatigue…I’m sure I’m leptin resistant as well. The Endo put me on Levothyroxine for a month and I gained 5 lbs. I had been prescribed WP Thyroid back when I had cancer and lost weight on it. He refused to prescribe the NDT and said I didn’t stay on the Levo long enough…clearly, I need to gain some more weight (I am over 100 lbs. overweight). I was able to convince my GP to put me on Nature-throid and in the past 4 days have lost over 5 lbs. I intend to follow your protocol and my doctor also prescribed Phentermine, so I will take that in conjunction with your fasting protocol.
Since I have not heard you address the high TSH level, as in my case, can you recommend any other things I could be doing to find success in my lifelong struggle with my weight?
Thanks,
Cheryl
Is it safe to do the infrared sauna on a fasting day? Could that damage the body in any way, or enhance the sauna’s detox effects?
Also, another fasting-related question: what should one do if they’re taking medication/supplements that are fat-soluble, but it’s a fasting day? Skip them that day, or take them while fasted? Thanks!
Hi Amelie,
Most people are able to use the sauna on fasting days but it just depends on the person, their goals and their medical conditions. When in doubt make sure to touch base with your physician.
Levothyroxine causing high blood sugars. Why?
Hi Lee,
Levothyroxine shouldn’t be causing high blood sugar.
I have been suffering for about 8 years this website just gave me hope! I’m finally seeing a doctor at Lenox Hill Hospital who doesn’t think it’s all in my head! I feel for the people on this site. Nothing worse then begging for help and they look at you as if your crazy!
Hi Kathleen,
Glad you found it helpful! Keep us updated on your progress.
Hi, Dr. Child’s.
I am a 48 yr old woman. Please forgive me for such a long post. I’m a bit at wit’s end. My issues are as follows:
Hashimoto’s thyroiditis
PCOS
Adrenal fatigue
Insulin resistant
Super low progesterone
low cortisol(adrenal fatigue)
fibromyalgia
Constant lower back/hip pain
30lbs overweight (can’t get it off for anything)
Perimenopausal
Chronic migraines (3+ month)
Horrible memory issues
Also: I smoke 1/2 of cigarettes a day. About to start Chantix (been trying to kick the habit for a long time.) I also drink between 2-4 cups of coffee per day.
Current treatment:
.05mg levothyroxine
5mcg liothyronine
200mg progesterone beginning 2weeks after the start of cycle
Additionally, I practice mindfulness (breathing techniques), daily prayer and I have a life coach (trying to help me be more organized and accountable.)
I am writing to you because I need to know if there are any docs like you in southern California. I have been seeing a D.O. for several years now. He just retired and closed up office although I don’t feel like I was getting very good results anyway. So I found a new D.O. Just had my first appointment with him and I don’t think we are going to be a good fit because he did a very poor job of listening to me.
My first appointment I was asking why I can’t manage to lose any weight in spite of regular exercise and he started in on I’m just eating too much and not exercising enough. I can flat say that’s not the truth. I only walk for exercise now (about 10 miles per week) because it WIPES me out. Last year I joined one of those boot camps that also do the macro/micro diet and about 10 days into the program I quit. I quit because I managed to Gain almost 5 lbs And I was practically in a coma for the next two days after every workout day. I felt beyond horrible. Like I said, I just walk now, but even that can do the same thing if I walk for more than a half hour. And I can truthfully say that I consume between 1200-1700 a day. (I can even tell you the nutrition content for everything I eat!)
I keep a very busy schedule. Mom of 2 girls under the age of 10. I’m a realtor. I am PTA president. I exercise every other day. Very involved in church. So, I am very definitely not sedentary.
I should add that I did not have any of these issues before I had my 10 yr old. Maintained my weight between 115-120 lbs. Had extra low blood pressure. Did have chronic hip pain on one side and migraines but no other complaints. 2.5 yrs of fertility treatment and after I had her, my body literally fell apart.
I’m so tired of not really being heard. I need a Dr. like you. Can you please point me in the direction of someone? Please? Again, sorry for the diatribe. I’m kinda at wit’s end.
Hi Chanda,
With such a complex history your best bet is to seek out a knowledgeable physician to help guide you. There’s no replacement for professional help in situations such as yours. You can find more info on how to do that here: https://www.restartmed.com/thyroid-doctor/
Hello Dr Child’s,
Thank you for your posts and info. This further tells me that all the Dr’s I have seen just overlooked all my issues because almost if my results are “normal”. I have high insulin levels and was referred to a endocrinologist but he said my levels weren’t high enough for him to treat. I also have high levels of testosterone with excess hair on my chin and thinning hair on my head. I feel dizzy often, fatigue, insomnia, sleep apnea, chronic pain from a laberal tear on my hip, pain in back and a 10mm tumor on my kidney. I was just referred to a urologist for the kidney and see a pain management Dr for my hip. I just started having confusion when I wake in the morning, not knowing what is needed to do or what day it was. I have no energy to clean house or even make dinner for my family. I also have cysts on my ovaries, a fatty liver, and mood swings. I was referred to a therapist for my anxiety. I also have low vitamin D, and am over weight. I’ve tried doing exercise but it takes 3
Days to recover from pain which makes it not worth it. I also have a tumor on my arm which hurts often, not
Allowing me to do much. I had a endometrial ablation 10 years ago from heavy periods. I still get pelvis pain and was told I also have uterine fibroids but nothing done about it. I’ve been dealing with this for over 15 years. What should I have my Dr look into next? I am just lost with all the rest I’ve done and multiple ER visits from not feeling well as if I had a heart attack or about to faint. Please help.
Hi Evangeline,
The single best thing you can do is find a doctor who is knowledgable and willing to look at the whole picture. The only way to find out where to start first is by taking that approach.
Dr Childs I have taken the last 2 days and have read through everything on your website. I have hypothyroidism been on eltroxin (levothyroxine) for 24 years. I immigrated to Australia after I got married and my weight was always and issue after the thyroid diagnosis, before I got diagnosed I was very skinny. I could not fall pregnant naturally with my first 2 daughters had to get injections and clomid. (With each pregnancy I gained 55pounds and lost about 22pound of this weigh after each pregnancy) Then after the birt of my second daughter I just felt horrible I want to a new GP who referred me to an endocronologist who put me on 20mcg T3 with 50mcg levothyroxine. The I naturally fell pregnant with my son and the cycle started again we moved to the middle east and T3 was not available and I found HCG and dropped the weight only to struggle with keeping it off and today I am heavier than when I fell pregnant. (I have a small frame).
I was diagnosed with PCOS (slightly enlarged ovary with wall cysts) in November 2018 just a month before we moved to new zealand my endo in middle east said there is nothing that can be done but I to eat less and exercise more and to see a psychologyst (as he said I am depressed). He did suggest metformin 2000mg (this took away my appetite) a day and saxenda (which did not work). I was diagnosed with fibrocystic breast change too. My period have been all over the place and my cycle has always been around 34-37 days with 2 days on 3 days off another 4 days on and some spotting, which the gynecologist also just said is normal.
So 2 weeks ago I got T3 from my endocronologist in australia. I started with 20mcg again however I have been experiencing extreme muscle pain walking like a 90year old (Im 46). Also HDL, LDL and total cholesterol is high and triglycerides is normal.
I also started HCG again in desperation to lose weight as absolutely nothing fits me. In the last 13 months I have gained 24 pounds.Then I came across your website.
Now Im wondering if I should continue with T3 (maybe up the dose I have seen no change in 2 weeks so it might be too soon) and add the metformin 2000 per day back and the take HCG every other day at a higher dose (currently I take 180IU). Then with this just do a higher protein diet, lower fat and lower carbs (low GI) at around 1800 calories. I have also bought lugol’s solution (10% potassium iodide, 5% iodine).
I would appreciate your thoughts on this.