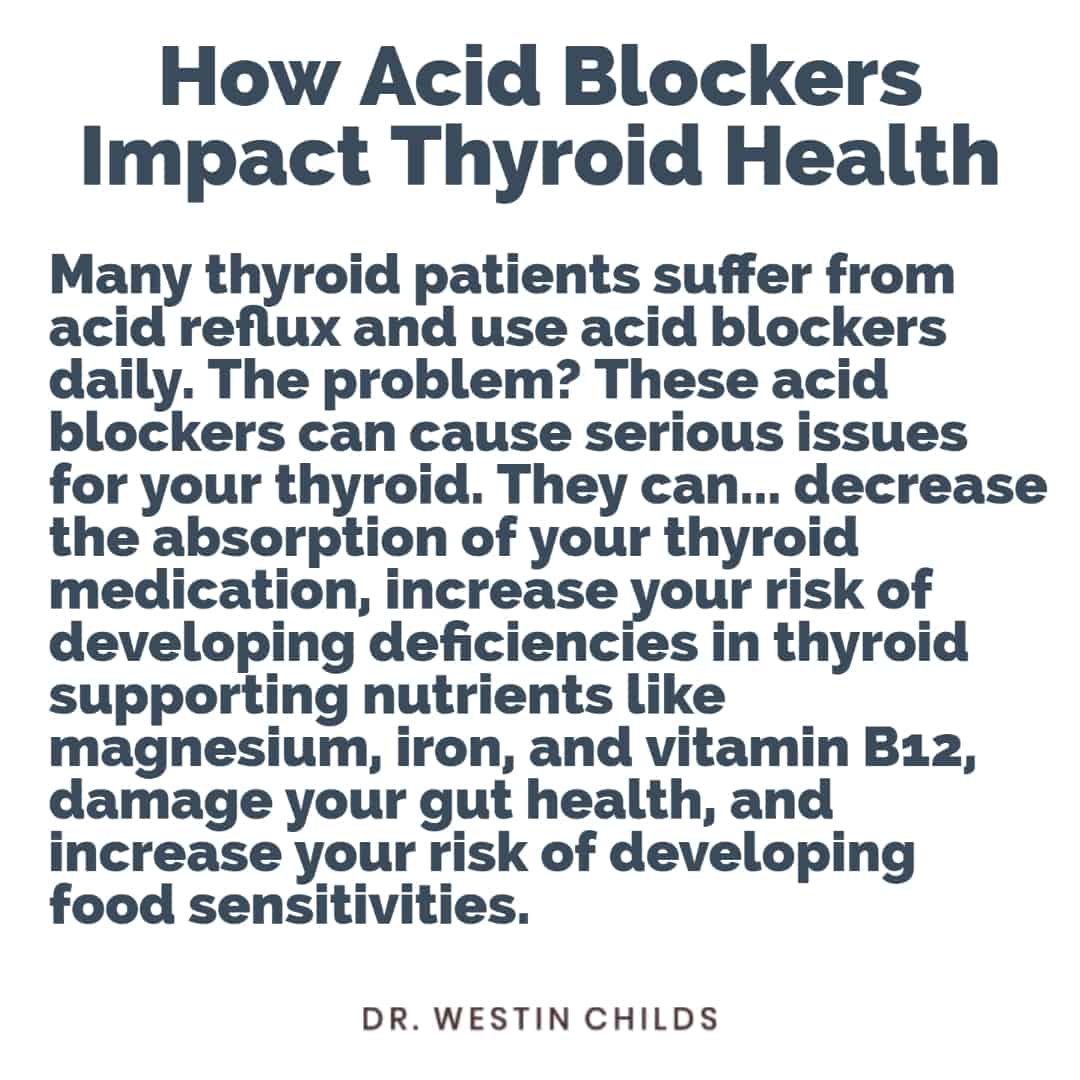
Acid blockers are used by millions of people each and every day and yet they have the potential to cause profound problems.
Nowhere is this more apparent than in thyroid patients where acid blockers can wreak havoc on thyroid function in a number of ways.
And, in case you think I’m joking about how common these medications are, consider these statistics:
Levothyroxine (a prescription thyroid medication) is the third most commonly prescribed medication in the United States with over 101.9 million prescriptions out there right now.
Omeprazole (a common acid blocker) is the 7th most commonly prescribed medication in the United States with over 68 million prescriptions out there right now.
We don’t know how many people are using BOTH levothyroxine and omeprazole simultaneously but we can make an educated guess that this number is in the millions of people.
If I’m taking a stab at the number, my personal guess would be definitely over 10 million people who use both simultaneously primarily because acid blockers are available over the counter and don’t always require a prescription medication.
In fact, you may be one of these millions of people!
So what’s the big deal? Why is it a problem to take acid blockers if you have a thyroid problem?
In this article, I’m going to outline 7 reasons why thyroid patients, in particular, need to be wary about using acid blockers.
These reasons range from its interference with thyroid medication absorption to increasing your risk of nutrient deficiencies and many others.
And this is really just the tip of the iceberg.
Let’s jump in:
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
What Are Acid Blockers?
Let’s start with some basics.
What is an acid blocker?
An acid blocker is a medication that reduces how much acid is either produced or pumped out into your stomach.
Acid blockers are used for many medical conditions but are most commonly used for treating acid reflux.
If you aren’t using an acid blocker for treating acid reflux then you may be using it for treating H. pylori (1), a stomach ulcer (2), or a gastrointestinal bleed.
It doesn’t really matter why you are taking them, the effect is still the same as far as your thyroid is concerned.
Why would you want to reduce the amount of acid in your stomach?
The idea goes something like this:
Acid that your stomach produces naturally can be potentially damaging for tissues outside of your stomach.
If you have acid reflux, that means that you may be pushing up stomach acid into the bottom of your esophagus which can damage the esophagus if it happens over many years (3).
Your doctor will tell you that the best solution for managing this problem is to reduce how much acid your stomach produces.
That way, if your stomach juices get pushed up into your esophagus then it won’t cause problems!
Doctors get really concerned about acid reflux because prolonged damage to the esophagus may increase your risk of developing esophageal cancer.
And patients get really concerned because acid reflux can cause chest pain (4) and really hurts!
In theory, this method of managing something like acid reflux makes sense.
The only problem is that using acid blockers is like playing a game of whack-a-mole.
Using an acid blocker may solve the damage to the esophagus (even though it doesn’t actually stop the refluxing from occurring) but has the potential to cause more problems downstream.
It turns out that your body needs that stomach acid that your acid blocker is blocking!
Stomach acid is used to digest food, to break down nutrients, to help your body absorb the nutrients you get from food, and even to absorb and break down medications!
There’s also some evidence that stomach acid is beneficial to the little bacteria that populate your intestinal tract.
The funny thing is, this is well known in the medical community and they know that using acid blockers long-term can cause problems.
In fact, if you look at the back of the box of your acid blocker it will tell you that these medications were never designed to be used for longer than 2-4 weeks (5).
But this doesn’t stop doctors or patients from using them for years and years and even decades in some situations.
Long-term use of acid blockers has been associated with developing gut infections like Clostridium Difficile colitis (6) and increases your risk of breaking a hip or bone (7).
These are just some of the downsides to using acid blockers, we will get into more in just a minute.
For now, just realize that while acid blockers may temporarily solve some issues in the short term, they create way more problems than they solve in the long term.
List of Acid Blockers (Check to see if you are taking any!)
Let’s do a quick check to see if you are taking an acid blocker.
One quick thing to note is that acid blockers are available both over the counter from your local drug store as well as via a prescription from your doctor.
So don’t assume you aren’t taking an acid blocker if you don’t have a prescription from your doctor!
Because they are so readily available and because they go by so many different names, it’s a good idea to check if you picked one up from the grocery store at some point.
There are 2 main classes of acid blocking medications.
- Proton Pump Inhibitors (commonly referred to as PPIs) – Medications that fall into this category include: Dexilant, Nexium, Prevacid, Prilosec, and Protonix. Any medication that ends in -prazole is considered to fall into this class of medication.
- H2 Blockers (an older class of medication but still available over the counter) – Medications that fall into this category include: Zantac, Pepcid, Tagamet, Fluxid.
A couple of things to note when looking at this list:
The first is that this isn’t a complete list and you can still be on one if your medication isn’t on this list.
Medications often take on different names in other countries or as generics flood into the market.
Be sure to check your medication against the list of names found here.
The second is that these medications are very effective at doing what they do.
In other words, even if you are taking a small dose of either type of medication they are effectively blocking most of your stomach’s ability to produce acid.
The potential side effects of this are seen when using low doses of acid blockers from either class of medication.
Reasons to be Cautious of Acid Blockers as a Thyroid Patient:
Let’s talk specifically about how acid blockers negatively impact thyroid patients.
I came up with a list of 7 reasons why you want to be cautious using acid blockers if you have a thyroid problem but there are probably additional reasons not listed here.
#1. They can decrease thyroid medication absorption.
The first reason to be cautious of using acid blockers has to do with its ability to limit thyroid medication absorption.
And here I’m talking about ANY thyroid medication including medications such as levothyroxine, Synthroid, Natural Desiccated thyroid, Cytomel, and liothyronine.
Regardless of whatever thyroid medication you are taking, there is a risk that your body will not be able to absorb that medication if you are taking it with an acid blocker.
And when I say “with” an acid blocker I’m not talking about taking it at the same time or anything like that.
If you are using an acid blocker AND taking thyroid medication then you may have a problem.
The reason is that acid blockers decrease acid production ALL day long and it is the reduction in acid that limits thyroid medication absorption.
So even if you were to take your acid blocker in the evening and your thyroid medication in the morning, you may still experience this problem.

Why is it important to ensure you are getting your thyroid medication into your body?
Well, if you have low thyroid function then it is your thyroid medication that is helping you feel better.
If you don’t get enough thyroid hormone into your body then you will continue to experience low thyroid symptoms like fatigue, weight gain, hair loss, and cold intolerance.
You may also find that your thyroid lab tests fluctuate significantly if you take your acid blocker off and on.
This problem won’t occur if you take your acid blocker faithfully but you can imagine a scenario in which your TSH and free T4 levels fluctuate if you only use your acid blocker occasionally.
This can make nailing down a dose that works for your body difficult and provide unnecessary diversions in getting to the root cause of your thyroid condition.
Again, let me reiterate, this problem exists for ALL thyroid medications because your body needs acid to help break down the thyroid medication itself for absorption.
#2. They increase your risk of developing magnesium deficiency.
You will see a trend as we talk about the problems that acid blockers cause and many of these problems stem from nutrient deficiencies.
For #2, we are talking about magnesium levels.
If you don’t produce enough stomach acid then you will be more prone to developing magnesium deficiency.
But why does that matter?
Well, outside of its impact on thyroid function, we know that magnesium acts as a cofactor for over 300 enzymes in the body.
But specific to the thyroid, we know that low magnesium impacts your immune system which may put you at more risk for developing autoimmune diseases such as Hashimoto’s thyroiditis.
It’s probably not the magnesium deficiency itself that CAUSES the autoimmune disease but it is the magnesium deficiency state that fans the flames of autoimmunity, so to speak.
Magnesium helps to keep your immune system in check and helps fight and prevent inflammation by helping to produce anti-oxidants such as glutathione.
We also have studies that show that supplementing with magnesium may positively impact thyroid function lab tests by improving the TSH (8).
Magnesium is also required to produce the energy necessary to get iodine into your thyroid gland.
Low magnesium means that the iodine you take or get from your diet will be less effective.
As a thyroid patient, reducing your level of magnesium may put you at increased risk for not only making thyroiditis worse but also impacting thyroid function itself.
What can increasing your magnesium level do for you?
People who increase their magnesium level report that they get better sleep, have less anxiety, have more regular bowel movements, and have more energy.
As a thyroid patient, you definitely want to ensure that you have proper magnesium and that may start with improving how much magnesium you are absorbing!
Magnesium is primarily found in plant rich foods but you can also take it in supplement form which may be ideal for those on acid blockers.
Even though you won’t absorb all of it, increasing how much goes through your system is still better than nothing.
#3. They increase your risk of developing iron deficiency.
Acid blockers also increase your risk of becoming iron deficient.
And iron is another very important nutrient for thyroid function.
Iron is required for an enzyme known as thyroid peroxidase to function properly.
If thyroid peroxidase is not working correctly because you don’t have enough iron then your thyroid will not be able to use iodine to create thyroid hormone.
Aside from its impact on thyroid function, iron also plays an important role in helping your hair grow!
Hair loss is definitely a top concern for many thyroid patients as it is frequently a side effect of both low thyroid function and high thyroid function.
Iron also helps you feel energized because of its role in providing oxygen to your cells for energy production.
As a thyroid patient, you should be very concerned about iron because iron deficiency leads to impaired thyroid function which leads to decreased iron absorption and worsening iron levels.
This downward cycle can only be solved by fixing both thyroid function and your iron levels simultaneously.
Women are at higher risk for developing iron deficiency (with or without acid blockers) because of their menstrual cycle.
Because most patients with thyroid problems happen to be women, this problem is amplified.
Be sure to keep an eye on your iron status and ferritin levels if you have used an acid blocker in the past (or if you are using one now!).
#4. They increase your risk of developing Vitamin B12 deficiency.
Vitamin B12 is another huge vitamin for thyroid patients and it’s something that acid blockers can make you more deficient in.
We already know that a huge number of thyroid patients suffer from sub-optimal vitamin B12 levels, somewhere around 40% (9).
And this is concerning because of B12’s importance in helping your body to produce energy.
Vitamin B12 deficiency can lead to symptoms ranging from decreased energy, to weight gain, to brain fog, and even depression.
If these symptoms sound familiar to you it’s because they are some of the same symptoms that low thyroid can cause.
This makes it all the more important to ensure that your B12 levels are optimal so that they do not cloud your picture or prevent you from feeling better!
Vitamin B12 is absorbed in the gut and stomach acid is required for its absorption (10).
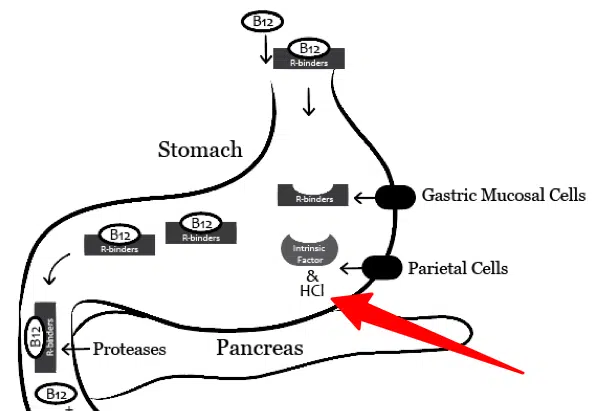
Low thyroid status reduces acid production in the stomach which is why so many thyroid patients suffer from B12 deficiency.
When you add on further acid suppression from acid blockers, the problem often gets exacerbated significantly.
As a thyroid patient, you should put a priority on testing your B12 status using the correct tests.
Many doctors tend to order the wrong tests which may lead to undiagnosed B12 deficiency in thyroid patients, especially those that are also taking acid blockers.
In some cases, thyroid patients may need to supplement with sublingual forms of B12 or vitamin B12 shots to bypass the intestinal tract.
Bypassing the intestinal tract can help ensure that you are getting vitamin B12 into your body even while taking acid blockers.
Obviously, it’s not recommended to take acid blockers and vitamin B12 at the same time, but if you plan to do this using sublingual or B12 shots is definitely better than using capsules or tablets.
#5. They increase your risk of developing intestinal dysbiosis and small intestinal bacterial overgrowth.
Suppressed acid production also leads to downstream changes in your intestinal bacteria.
Your gut bacteria, known as your microbiome, play a synergistic role in maintaining the health of your entire body.
Your job, as the host, is to put food down into your gut that helps healthy bacteria to grow and thrive.
In return, healthy populations of gut bacteria then help your immune system to function, they can help alter your appetite, regulate neurotransmitters such as serotonin, and help reduce inflammation.
This all assumes that you have a good relationship with your gut bacteria!
Many thyroid patients, especially those taking acid blockers, do not.
Changes in your stomach acid alter how your food is digested.
If you are not able to break down your food at the right time then you may inadvertently feed the wrong bacteria further down in your intestinal tract.
Low stomach acid also changes the environment in which these bacteria can thrive.
The use of acid blockers seems to create an environment that is favorable for the type of bacteria you don’t want growing in your gut or colon.
This is why some people who take acid blockers over the long run have an increased risk of developing C. Difficile colitis.
But even in the short term, you may develop overgrowth of bacteria in the intestinal tract known as small intestinal bacterial overgrowth (SIBO for short).
SIBO leads to gut inflammation, further impairment of nutrient absorption, and additional symptoms such as constipation/diarrhea, abdominal pain, bloating, excess gas production, and more.
Getting off of acid blockers can help restore your gut bacteria to its normal healthy state but you may also need additional treatments such as probiotics and prebiotics.
#6. They may increase your risk of developing food sensitivities.
Studies in both children and adults show that using acid blocking medications increases your risk of developing food allergies.
In children, for instance, the use of acid blockers in the first 6 months of life results in a higher risk of food allergies compared to taking antibiotics (11)!
It’s not exactly understood why acid blockers increase your risk of food allergies and sensitivities but it’s thought that it’s related to two areas:
The first is through its impact on intestinal bacteria and your microbiome (which we discussed above).
And the other is through its impact on protein breakdown.
When your stomach acid is low your body is not able to adequately break down certain proteins which leads to larger protein fragments that then may react with your immune system (12).
The end result is that your immune system starts reacting to foods from those protein fragments and you end up with food sensitivities.
Aside from the fact that you don’t want food sensitivities at all, thyroid patients already have to be very vigilant about what foods they put into their bodies.
If you limit the foods that you can eat even further with the use of acid blockers then you are making your job at finding the right diet for your body that much more difficult.
#7. They may lead to inflammation in the gut which can negatively impact thyroid conversion.
Finally, through some of the mechanisms previously mentioned, acid blockers can result in inflammation in your gut.
This is a problem for thyroid patients because the gut is a big source of thyroid conversion and the creation of T3 thyroid hormone.
Conditions such as gut inflammation, intestinal dysbiosis, and even SIBO may limit how well your gut can convert T4 to T3 which may have an impact on your free thyroid hormone levels.
Clearing up gut inflammation is a quick way to indirectly improve thyroid function through this mechanism.
Getting Yourself Off Of Acid Blockers
After reading this, you may be asking yourself how the heck are you supposed to get off of your acid blocker.
After all, some people, perhaps even you reading this, may have been taking an acid blocker for years or even decades.
People in this situation always get frustrated because they know if they stop taking their acid blocker they will end up with acid reflux because of acid rebound (13).
What are you supposed to do in this situation?
It starts with understanding what actually causes acid reflux in thyroid patients.
In many cases, thyroid patients suffer from acid reflux because they are not producing ENOUGH acid.
Remember, low thyroid states reduce stomach acid production.
As a result, many thyroid patients are incorrectly placed on acid blockers which can make the problem even worse.
On the flip side, even those with high acid content often benefit from taking additional stomach acid.
Taking additional acid, in the form of supplements, can help your body digest food and improve your microbiome.
It may not sound intuitive to take acid if you have a problem with acid but it works by treating the root cause of acid reflux.
If your acid reflux doesn’t stem from low stomach acid (as it does in many thyroid patients) then it probably stems from an unhealthy microbiome from consuming processed foods, dairy, gluten, or even another stomach condition such as H. pylori.
The key to fixing acid reflux is finding out the source of your acid reflux and fixing that problem.
Once you do, you should be able to throw your acid blockers away and never look back.
Wrapping It Up
Acid blockers, including proton pump inhibitors and H2 blockers, are among the most commonly prescribed medications in the United States.
Thyroid patients, because of their propensity to experience acid reflux, are often taking both thyroid medication and acid reflux medications.
This promotes a problem in thyroid patients because of the importance acid plays in absorbing nutrients, gut health, and thyroid medication.
The result may be worsening thyroid function for patients who take acid blockers!
If you are a thyroid patient using acid blockers then fixing the root cause of your acid reflux will help you to get off of your acid blocking medication and improve thyroid function.
Are you a thyroid patient currently taking an acid blocker?
If so, do you think you have experienced any of the negative side effects mentioned above?
Have you had your nutrient levels for vitamin B12, iron, or magnesium tested?
Did you know that you shouldn’t use your acid blocker for more than 2 weeks?
Have you tried getting off of your acid blocker? If so, how did you do?
Leave your questions or comments below!