Up to 7.5% of all pregnant women may experience a thyroid condition known as postpartum thyroiditis.
Even more staggering is the fact that up to 25% of these women, who go through postpartum thyroiditis, will develop PERMANENT hypothyroidism as a result (1).
This makes diagnosing and identifying this condition incredibly important.
This guide will teach you how postpartum thyroiditis presents, how long it takes to recover, and how to test for it, and includes natural treatment options.
Let’s jump in:
What is Postpartum Thyroiditis?
Postpartum thyroiditis is a thyroid condition that MANY women will experience after they have a baby.
Fortunately, this condition tends to be self-limiting (meaning it resolves on its own without treatment) but it’s still very important to understand.
This immune confusion comes from pregnancy in which your body naturally alters your immune function to prevent damage to your developing baby.
These changes in immune function carry over into the postpartum period which can occasionally “confuse” your own immune system into attacking your thyroid gland.
This confusion occurs in up to 7-8% of women or, in other words, 1 out of 12-13 women who have a baby.
Postpartum thyroiditis can be confusing because it can cause both high and low thyroid problems (hyperthyroidism or hypothyroidism) which means that no two women will present exactly alike.
Despite this, most women will go back to normal over a 12-month period.
But that doesn’t mean they will be “fine” during this time period.
While your thyroid is going haywire it’s normal to experience symptoms such as palpitations, anxiety, hair loss, depression, and so on.
These symptoms can easily be confused with normal postpartum symptoms, but they can be differentiated with special tests.
In addition, up to 25% of women who have postpartum thyroiditis are at risk for developing PERMANENT hypothyroidism later in their life.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Symptoms of Postpartum Thyroiditis
How do you know if you have postpartum thyroiditis?
It can sometimes be difficult to determine what kind of symptoms you are experiencing, especially in the postpartum phase.
Are you experiencing postpartum depression or is it really your thyroid?
Is your hair falling out a symptom or a normal part of hormonal changes which occur after delivery?
Are you not returning to your typical pre-baby weight as quickly as you want?
All of these slight changes can be an early indicator that your thyroid is off and that something may be a problem.
But as you can see, some of these problems would be considered “normal” in the postpartum period as well.
So how do you differentiate between the two?
The best way is to combine your symptoms with your lab tests.
Your symptoms may not be clear by themselves, but when accompanied by abnormal lab tests you can easily identify the issue.
We will discuss lab tests below (you can skip to that section if you want), but it’s also important to talk about how postpartum thyroiditis tends to progress.
Women with this condition can present with either HYPERthyroid symptoms or with HYPOthyroid symptoms.
This means that two women can have the exact same condition (postpartum thyroiditis) and yet present with the exact OPPOSITE symptoms.
Because of this, you need to understand the symptoms associated with both conditions.
Women with this condition tend to feel overwhelmed, jittery, anxious, and so on.
Around 50% of women with postpartum thyroiditis will go through the hyperthyroid phase.
Symptoms of the hyperthyroid phase include:
- Heart palpitations
- Fatigue
- Heat intolerance
- Irritability/nervousness
- Insomnia
- Up to 33% of women may be hyperthyroid but asymptomatic
These symptoms tend to be mild but may be enough to bring you into your doctor’s office to try and figure out what is going on.
These symptoms tend to peak about 3 months after delivery as well but can start earlier and proceed later than that.
Another 50% of women will experience the symptoms of hypothyroidism (either, to begin with, or following the symptoms of hyperthyroidism).
Hypothyroidism is the exact opposite condition as hyperthyroidism and is the result of decreased thyroid hormone in the body.
Symptoms of the hypothyroid phase include:
- Fatigue
- Hair loss
- Weight loss resistance (or minor weight gain)
- Depression
- Constipation
- Dry skin or dry brittle hair
- Decreased lactation/milk production
The symptoms of hypothyroidism tend to peak around the 6-month mark and usually tend to completely subside by month 12 (after delivery).
These symptoms may vary in intensity from one person to the other.
This variance is the reason that some women may need thyroid medication while others can go without it.
Testing for Postpartum Thyroiditis
Testing for thyroid conditions in the postpartum period can be done quite easily and should be routine if you are experiencing any of the symptoms we listed above.
If you suspect you have postpartum thyroiditis then your next step is to get the following lab tests:
- TSH (thyroid stimulating hormone) (3) – In the hyperthyroid phase your TSH will be LOW (usually suppressed) and in the HYPOthyroid phase your TSH will most likely be high (somewhere between 5.0 and 10.0 uIU/mL. The higher your TSH the more likely you are to develop permanent hypothyroidism.
- Thyroid antibodies (TPOab & TGab) (4) – Up to 80% of women with hyperthyroid postpartum thyroiditis will be positive for thyroid peroxidase antibodies.
- Thyroid stimulating immunoglobulin (TSI) (5) – TSI can help differentiate between Graves’ disease (another disease that causes hyperthyroidism) and postpartum thyroiditis during the hyperthyroid phase. A small percentage of women with postpartum thyroiditis may show receptor positivity for TSI even though this is generally a marker for Graves’ disease.
The point of testing your labs is three-fold:
#1. To help identify and diagnose your condition.
#2. The second is to help you determine how to proceed with treatment and what kind of options are available to you.
#3. And the third is to help you monitor and track your disease course over time.
Many women will just be happy to know where their symptoms are coming from and they are happy to understand what is happening in their bodies.
But beyond this comfort, it’s also important to diagnose your condition because it affects your treatment options.
The severity of your lab tests (in terms of how abnormal they are) can help you to determine how aggressive you want to be with your treatment.
Some women, especially if their symptoms are relatively easy to manage and their lab tests are not grossly abnormal, may be fine with the “wait and see” approach.
Other women, may benefit tremendously from additional thyroid hormone replacement therapy to help manage depression, weight gain, hair loss, and so on.
This type of consideration can be taken on an individual basis.

Lastly, it’s also important to track your lab tests over time (with tests at least every 2-3 months) so you can determine if you are actually improving.
The typical course of postpartum thyroiditis is one that usually resolves in 12 months or so, but what if your symptoms persist beyond that time?
Checking your lab tests and monitoring them over this period can help you to determine if indeed you are getting better (or worse) and help you manage your expectations.
Postpartum Thyroiditis Typical Course & Recovery
So what can you expect as a patient if you have postpartum thyroiditis?
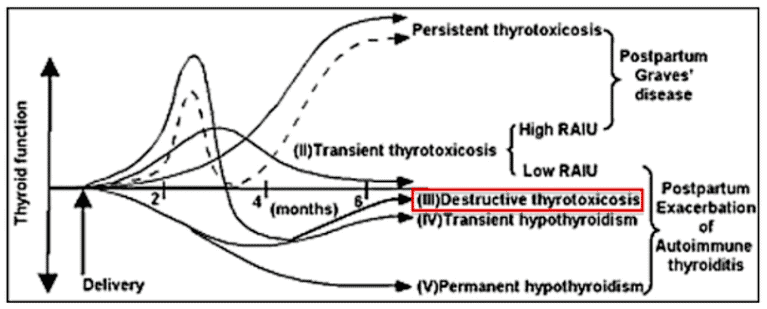
There are really four main outcomes that can come from this disease state.
#1. Some patients (around 32% of all patients) begin with hyperthyroidism which peaks around 3 months postpartum and then goes back to normal by about 6 months postpartum.
#2. Other patients (around 25% of patients) begin with hyperthyroidism which then bounces to hypothyroidism around the 3-month mark (postpartum) which then rebounds back to normal thyroid function around 12 months postpartum.
#3. Other patients (around 43% of patients) skip the hyperthyroid phase (outlined above) and head straight to hypothyroidism which peaks around the 3-month mark. This hypothyroidism then slowly improves and tends to resolve around the 12-month mark. This represents the most common course for most patients.
#4. Lastly, another subgroup of patients skip the hyperthyroid phase and head straight for hypothyroidism but these patients never recover and end up with permanent hypothyroidism. This is the most serious consequence of postpartum thyroiditis and is the option that you want to avoid if possible. Up to 23-29% of women with postpartum thyroiditis will end up with permanent hypothyroidism several years after pregnancy.
You can see an image that outlines these options below (6):
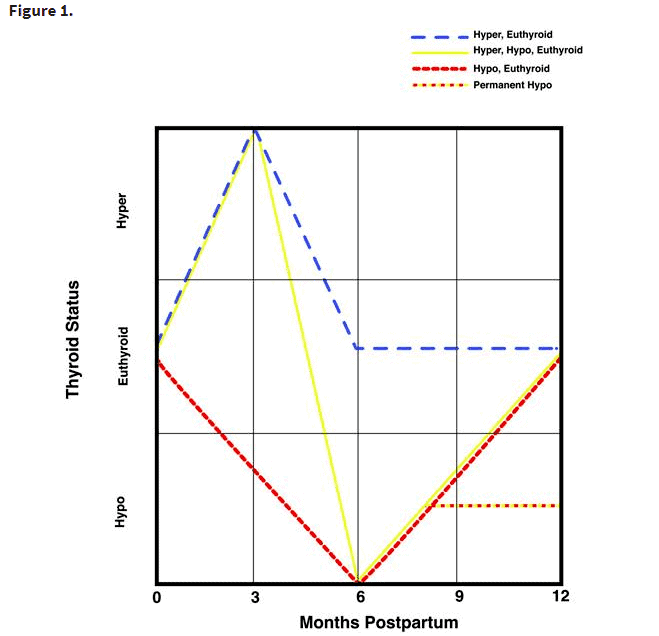
The main takeaway here is that up to 80% of women who present with postpartum thyroiditis will COMPLETELY recover without any long-term consequences.
That does leave, however, up to 20% of women who will end up with permanent hypothyroidism as a result of this condition.
With odds as high as 1 in 5 women developing complete hypothyroidism (meaning you will require thyroid medication for life) it’s a good idea to take this condition seriously.
Because these odds are quite high it’s a good idea to review the treatment options (listed below) with the goal to improve the odds that you will recover without permanent issues.
Natural Treatment Options + Thyroid Medication
One of the most frustrating aspects of postpartum thyroiditis is that there aren’t really any concrete therapies that physicians can use.
Instead, most of the treatment largely depends on how you feel, what your doctor is comfortable with, and how aggressive he/she wants to be.
Because of this, most patients (about 70%) will be told to “wait and see” with frequent lab tests over a 6-12 month or so period.
This can be incredibly frustrating for patients who may be suffering from a multitude of symptoms such as weight gain, depression, hot flashes, and so on.
But don’t let this discourage you, because there are some natural treatments that you can potentially start.
The first two listed below can be started by all women, but the third will require a physician’s prescription (more on that below).
#1. Diet
The first therapy is to adjust your diet.
If you haven’t done this already then there is a decent chance that you will notice a significant improvement with this change alone.
The good news about postpartum thyroiditis is that most of the time, it is transient (meaning it will go away on its own without permanent side effects).
You can take advantage of this by using some very specific diets which are high in vegetables/fruits and low in processed foods.
These types of diets also cut out gluten, sugars, dairy, and other common allergens which commonly cause issues for thyroid patients such as those with Hashimoto’s thyroiditis.
I would strongly encourage you to consider altering your diet instead of hanging out and waiting to see if your condition will pass.
With a 20% chance of developing permanent hypothyroidism later in your life, it’s worth it to be aggressive with your diet in the short term.
The exact diet you use can vary (based on your needs, tastes, and so on), but you should be good to start with any of the following diets:
- Autoimmune protocol diet (AIP) – Generally I don’t recommend this diet, but it seriously packs a punch in the short term (1-2 months) and may be worth a try to really balance immune function during the postpartum period. It’s also not a bad idea to be eating healthy for your kiddo!
- Whole 30 Diet – This diet isn’t quite as restrictive as the AIP diet and so it may be easier to follow for many women. This diet is high in all-natural whole foods, fruits, vegetables, nuts, and meats.
- Whole-food Vegan Diet – The whole-food vegan diet is primarily high in whole plant-based foods such as fruits, vegetables, legumes, nuts, and seeds. If you opt for this you will need to make it gluten-free as well.
- Basic or Strict Paleo Diet – The paleo diet automatically restricts
If these diets are confusing for you, then you can do your best to follow these basic guidelines and eat foods/meals which fit into them:
- Avoid Gluten, Dairy & Soy
- Avoid processed foods (anything in a box)
- Avoid eating out
- Avoid sugary drinks, coffee, and other novelty drinks
- Eat whole foods
- Avoid processed fats
- Avoid extra or added sugar
These diets do not necessarily need to (or should be) continued forever, but they may help calm down the inflammation and autoimmunity in your body in the postpartum period.
#2. Supplements
Supplements play an important role in providing your body with nutrients it may be missing or with nutrients that may act to calm down inflammation and promote normal immune function.
The most commonly used (and safest in the postpartum period) include:
- Selenium – Selenium is required in many enzymes in the body including those which help promote thyroid hormone creation. Selenium deficiency has been implicated in the pathogenesis (7) of Hashimoto’s thyroiditis and supplementing with selenium has been shown to reduce antibodies in women with postpartum thyroiditis (8). It has also been shown, in these studies, to reduce thyroid inflammation (both things you want!). Taking selenium may also reduce the risk that you will develop permanent hypothyroidism.
- Zinc – This trace mineral also helps promote thyroid function (9) but, perhaps more importantly, it’s required for optimal immune function. Zinc is commonly used in “flu and cold” remedies because of its properties. Taking zinc in combination with selenium is a great place to start if you have postpartum thyroiditis (10). Many women in the US may be at risk for zinc deficiency due to soil depletion and poor diets.
- Fish oil – Fish oil is added to this list because of its special properties in reducing inflammation in autoimmune diseases (11). Fish oil can help calm down the body by normalizing the ratio of omega fatty acids. It also has special properties which may help promote normal fat metabolism.
- Curcumin – Curcumin, like fish oil, is helpful in reducing inflammation. Curcumin is the active ingredient in the spice turmeric and is well known for its ability to help balance blood sugar, help reduce inflammation, improve metabolic function, and so on (12). Fish oil and curcumin can be used together or without the other. The goal here is to just use something to help reduce inflammation.
Supplements provide an added boost for your body to get the nutrients it needs, especially those which may be difficult to get from foods alone.
It’s certainly possible to get all of your nutrients from food, but it may require massive consumption of certain types of foods which can be difficult to get.
Adding supplements helps cover your bases and provides a continuous supply of nutrients and vitamins that your body needs.
#3. Thyroid Hormone (Not always Necessary)
While not necessarily a “natural” treatment, it’s still important to discuss the value of thyroid hormone for women with postpartum thyroiditis.
Thyroid medication is used to treat people who have LOW thyroid hormone (hypothyroidism) and is used to help supplement your body with whatever your thyroid is unable to make on its own.
Most women with postpartum will recover over a 12-month period (or so), but that doesn’t mean that they wouldn’t benefit from the temporary use of thyroid hormone in the meantime.
Thyroid hormone, for use in postpartum thyroiditis, is predominately used to help alleviate your symptoms, help you feel more like yourself, and help you take care of your child.
Taking thyroid medication can help improve your energy levels, reduce (or eliminate) depression, reduce the amount of hair you are losing, and so forth.
With benefits like these, the use of thyroid hormone should be considered in women with postpartum thyroiditis, especially if they are suffering considerably from their condition.
Up to 30% of women with this condition will take thyroid hormone medication (so about 1 in 3 women) which makes it fairly common.
The general stance from your doctor may be to “wait and see” but, depending on your labs and symptoms, you may want to push for thyroid hormone replacement therapy.
This should be left up to you (as the patient) and your doctor.
Final Thoughts
Postpartum thyroiditis is one of the most common endocrine conditions that women will face after they have a baby.
The good news is that this condition almost always resolves on its own over a period of time.
The bad news is that this condition can cause some serious symptoms which may impair your quality of life and prevent you from spending quality time with your new baby.
By understanding the signs and symptoms of this condition you will be well-equipped to help diagnose it or prevent your doctor from missing it.
If you do have postpartum thyroiditis make sure that you look at all of the therapies available to you, especially natural treatments.
Most doctors tend to take the “wait and see” approach, but that doesn’t mean you can’t change your diet, take supplements, and do your best to treat your condition.
Now I want to hear from you:
Are you suffering from symptoms in the postpartum period?
Do you suspect (or know) that you have postpartum thyroiditis?
Have you been able to treat your condition?
What has worked? What hasn’t?
Leave your comments below!





Dr. Childs: Thank you for this article. I’ve waited years to find anything close to what I have felt for years. #4 above describes my feelings before and after pregnancy like night and day. You stated above: “This immune confusion comes from pregnancy in which your body naturally alters your immune function to prevent damage to your developing baby.
These change in immune function carry over into the postpartum period which can occasionally “confuse” your own immune system into attacking your thyroid gland.” Can any of this be passed on to the baby? Can the baby be born with hypothyroidism, deficiencies, allergies, etc. due to the effects of this on the mother? Thanks.
Hi there!
Yes, the baby can be born with deficiencies if the mother is also deficient. I’m not aware of any studies that show babies to mothers with postpartum thyroiditis have an increased risk of developing the disease themselves, but there is a genetic component to Hashimoto’s which is worth considering.
Thank you for the article, it was very helpful. I had postpartum thyroiditis after my second pregnancy but it resolved on its own (was on medication for a few months). I got it again after my last pregnancy and have been on medication for 1.5 years now. My hormone levels seem to have been hovering around TSH of .2-.4, total T4 around 7.8 and and free T3 around 2.7. My question is, at any point is it worth seeing how my thyroid functions off of medication or am I stuck with this forever?
Hi Radhika,
It’s worth it to see if you can come off of the medication, but up to 20% of women who have postpartum thyroiditis will end up with permanent hypothyroidism.
Hello! This was an extremely beneficial article, thanks! I’m wondering how do doctors differentiate between PPT and Hashimoto’s?
Hi Lynn,
The timing is usually sufficient, if it’s in the postpartum period then it’s PPT and if it extends beyond that then it would be considered Hashimoto’s.
Thanks for this article. I had PPT after my 1st, was symptomatic with hyperthyroidism until 8 mo PP. I’m now 12 mo PP with my 2nd and have been suffering since he was 3.5 mo with debilitating hyperthyroid symptoms. They come and go with my cycle and my doctors have written me off because my TSH runs between 1.5-0.2 (I feel awful when it’s below 1). I’ve tried going gluten free, I’m on low dose methimazole, propranolol, etc…it helps a little but the flares are brutal. No Graves antibodies. Have you seen this?
Hi KP,
Yes, and you can probably impact it with further aggressive dietary changes such as AIP or a strict elimination diet (no bad oils, etc.). You’d also want to try anti inflammatory supplements, fish oils, probiotics, and so on. I would try something like this along with your dietary changes which includes D, magnesium, fish oil, probiotics, and more: https://www.restartmed.com/product/thyroid-daily-essentials-thyroid-multivitamin/
Hi KP, I know this post is really old. I am hoping to hear what helped you get through the hyperthyroid symptoms of postpartum thyroiditis? I am 9.5 month postpartum and suffering horrible hyperthyroid symptoms – insomnia, anxiety, dizziness, brain fog, etc.
How are you doing now?
Thank you,
Nat
Such great information! I was recently diagnosed with Postpartum Thyroiditis. I’m very frustrated because my condition has been pretty painful. I am 18 months postpartum and the doctors at the VA seemed to use Postpartum Thyroiditis at first and then said Hashimoto Thyroiditis. So, I’m confused! He encouraged me that it should get better soon. However, I am not very hopeful. The endo has a wait and see approach with me following up in 6 months. My antibody test was elevated to about 100-which doesn’t seem that high or concerning to him. The only reasonable thing my doctor said was to continue with my diet changes. I already avoid dairy, since I am sensitive to it. I’ve also restricted my diet to eliminate gluten and soy. Is it common for this condition to last 18 months postpartum? I’m hoping for relief soon. Thank you for the helpful tips.
Hi Starr,
Unfortunately, some postpartum thyroiditis turns into long-term Hashimoto’s and does not go away. You may be one of the unlucky 20% of people in whom it simply stays and doesn’t go away. Most of the time it fades within 6-12 months after pregnancy.
Thank you so much for this article! I had a miscarriage /D&C in January and I l started hyperthyroid symptoms a month later. My TSH came back low and I have an ultrasound next week. Is it common to have swollen lymph nodes and what feels like a swollen thyroid for months on and off? It seem like it flares up a little more at times and I have a slight sore throat. I have never been one to take daily allergy meds but I take Zyrtec now. I suffer from anxiety and big lack of appetite for over a month now. I’m so nervous to get pregnant again if this goes away. These hyperthyroid symptoms are a nightmare.
Good day Dr W Childs
My wife had a totalthyroidectomy in 1995 and she is now 65 years old
In 2018 my wife had palpitation and was said to have hyperthyroidism and was hospitalizes.
Dr. do you have any information on totalthyroidectomy and high thyroglobulin
Thanks in advance
Dennis
Hope to contact via phone number.
After a 2.5 year journey of seeing doctor after doctor, By a fluke I discovered I was hyper. I experienced the same same symptoms with my first child throughout the pregnancy and afterward, which never really seemed to go away. Then got pregnant again and started to develop strong symptoms once more in the pregnancy. I am 12 month pp and my endo says pp thyroiditis. My symptoms have decreased by eliminating triggers such as sugar and caffeine, but they are still there, particularly during my cycle and if I eat improperly. The symptoms are strong and they are many. My concern is this disease not completely gone by now and it have been lingering this long.
Hi Dr Westin child’s, I have been on your thyroid multivitamin and adrenal reset complex vitamins when I developed postpartum thyroiditis after my second daughter was born. I was only hyperthyroid though never went hypo. I didn’t so any medication just diet changes and your supplements. I’d Like your opinion though, I’m currently pregnant with my third baby. I stopped the thyroid multivitamin and am on a prenatal vitamin now is the thyroid multivitamin safe for pregnancy? Also I truly want to do everything possible to have a good postpartum period again and maybe avoid getting thyroiditis again. Is there any of your supplements you’d recommend I start once the baby is born? I was thinking the hyperthyroid bundle you sell especially since that was the only issues I had postpartum etc. Anyway I’m looking forward to hearing your response thank you!
Hi Casey,
For general health, you’d want to use the thyroid daily essentials, omega soothe SR, Functional fuel DETOX, and Vitamin d3 liquid. This will give you the best shot to hopefully avoid post partum thyroiditis.
If you do find out that you are hyperthyroid or become hyperthyroid then you could swap to the hyperthyroid bundle at that time.
In regards to thyroid daily essentials during pregnancy, there’s nothing in it that would be harmful by itself but I always recommend touching base with your ob/gyn to make sure you aren’t getting too much one of nutrient or another just to be on the safe side.
Hello Dr Westin, I was diagnosed with postpartum thyroiditis after having my first child last year, came across your site and worked on my diet which helped in swollen gland reduction. I am 6 weeks pregnant now and my thyroid is swollen. What should I do ? Will my thyroid protrudes as my pregnancy advances? What should I do to make it go away forever ?
Thank you for this information. I have been fighting the battle with doctors for 40 years now, with them either not believing me and saying I was fine, or wanting to treat me only with synthetic drugs and not wanting to even try something else. It took me about 30 years to find someone who would even listen. Still even on medication the systems persisted. My GP has just gotten my endocrinologist to consider adding cytomel. I have only been on it about 2 months but am starting to see some subtle changes.
I always have said that I thought this happened after I had my son (41 years ago), but no one gave any credence to me. Thanks for letting us know there really is such a thing as postpartum thyroiditis.
Hi Kat,
My pleasure! And I would also highly recommend getting out of the conventional medical system. You will probably find a lot more success in finding a competent thyroid doctor with this resource: https://www.restartmed.com/how-to-find-a-doctor-to-treat-your-thyroid/
I went hyperthyroid after pregnancy with my twins – luckily my doctor tested my thyroid as a standard of care. He referred me to another doctor (probably an endocrinologist, but it was so long ago I don’t recall) and by the time I got more tests done, my thyroid had apparently burned out, and I was so hypo that she called me in a panic to see how I was. I never had any symptoms, or maybe just didn’t realize, because it all happened quickly. That was 27 years ago and I have been on thyroid meds ever since. Have had slightly elevated antibodies over the years, but my last test they were at a 1 and 2. Have had to adjust my meds over the years, and most of the time when I know something is “off” I have hyperthyroid symptoms. I’ve luckily never had weight issues, but I exercise regularly and eat well. I believe though that I was fortunate that my thyroid issues were caught at the beginning. I have done the AIP diet due to numerous food sensitivities. I take several supplements and started LDN about a year ago after developing eczema on my torso. I’ve been gluten free for over 20 years. Finding a functional or integrative medicine doctor is key to helping you properly treat your thyroid.
Hi Mary Beth,
Thanks for sharing and I wholeheartedly agree! Finding a competent thyroid doctor is key.
I was had hypothyroidism and Hassimottos before pregnancy and now 4 months post partum I have turned hyper! Will my thyroid be more damaged after this dies down or could I possibly go back to my previous levels of levothyroxine?
Hi Miranda,
It’s always possible that it could calm down and go back to previous levels, the opposite is also possible. If you wanted to give yourself the best chance of going back to whatever your previous normal was then you would want to be aggressive with lifestyle changes like diet, exercise, stress, and so on.
I was diagnosed with postpartum thyroiditis at 4 months postpartum (June 2023) after a bout of vomiting and becoming extremely weak and faint that landed me in the ER. At this point my thyroid was hyperactive. My tsh at that time was >0.005 and my T4 was 3.26. I began taking several supplements and felt so much better for about a month and a half. I went last week for labs and my tsh is now 30 and t4 is 0.66. But other than having an afternoon slump I feel fine. My dr said he thinks I have hashimotos and gave me NP thyroid 30mg. I feel like that was a little rash of a diagnosis since it’s normal to go from hyper to hypo in PPT and my baby is not even 6 months yet. My mama had hashimotos. And my grandma Has thyroid disease so I am high risk for it becoming permanent however I am holding out hope that I can reverse this. I haven’t started the thyroid medication because I really don’t feel like I need it at this point. I wondered what you thought about my labs? I was positive for the antibodies but that’s normal with PPT. I really don’t like prescription drugs and would love to avoid if possible. What do you think about NP thyroid? Is it really a safe and natural option? I am only 30. I don’t want to mess with my bodies ability to create the thyroid hormones. I wondered if I should skip the prescription drugs and take your hashimotos bundle for the next 3 months and see how my blood work comes out then? I would really appreciate your thoughts!! I feel so unsettled about taking that NP Thyroid.
Hi Macy,
It’s not always necessary to take thyroid medications right away, but you should proceed with caution if you are breastfeeding. It may make the most sense to use a combination of natural therapies as well as thyroid medication and then wean off of the thyroid medication after a few months.