Does thyroid disease cause depression?
Should taking thyroid medication, if you have thyroid disease, eliminate your depression?
What should you do if you are taking thyroid medication but still experiencing depressive symptoms?
In this post, we will discuss the connection between hypothyroidism and depression including how to approach treatment, which thyroid medications are best, and other causes of depression that result in confusion for patients and doctors alike.
Let’s jump in:
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Does Thyroid Disease Cause Depression?
It is well known and widely accepted that thyroid disease does indeed cause depression (at least this is taught in medical school).
But the problem is that this connection has never actually been proven.
Instead what we have are the following connections:
#1. The fact that hypothyroid patients and depressed patients exhibit similar symptoms.
#2. The fact that depressive symptoms may be eliminated in some patients with the use of thyroid hormones/medications.
#3. The fact that thyroid hormone can be given as a stand-alone depression medication and in place of anti-depressants.
#4. The fact that thyroid hormones influence serotonin production in brain tissue which is the same mechanism of action as prescription anti-depressants medications.
#5. The fact that TRH (which is part of the hypothalamic control of thyroid hormone) is sensitive to serotonin. Low serotonin may stimulate an increase in TRH and high serotonin may reduce TRH production. This may indicate a connection between serotonin, mood, and thyroid hormone production.
When you have this much smoke there is a tendency to scream fire, but why then do so many studies show conflicting results regarding the connection between thyroid disease and depression?
Much of this may have to do with the fact that we still don’t really fully understand depression.
Like many diseases, it’s probably best to consider depression as a side effect that can be caused by multiple different types of disease states or medical conditions.
Instead of thinking of depression as a primary condition, it may be best to consider it as a side effect of some other problem or a manifestation of some other disease.
Why think of it in this way?
Because multiple conditions have been shown to cause depression.
Conditions such as hormone imbalance (menopause, low testosterone, thyroid disease, and so on), nutrient deficiencies (B12 deficiency), inflammatory states, and gut dysfunction have all been shown to cause depression.
These other causes of depression may be sufficient to “wash out” a connection between thyroid disease and depression in general population studies simply because thyroid dysfunction is only ONE potential cause of depression.
Does this mean that there is no connection between thyroid disease and depression?
No, not by a long shot.
But it does mean that thyroid patients should be approached differently if they have depression compared to the general population.
Treating Depression if you have Thyroid Disease
It is clear that thyroid disease is associated with depressive symptoms.
One of the most concerning aspects of depression and thyroid disease is that studies clearly show that patients already taking thyroid hormone (1) (meaning those who have been diagnosed with thyroid disease) have a much higher rate of depression when compared to healthy adults.
This connection extends beyond depression and also includes anxiety.
Studies have shown that women who take T4 thyroid medication (to treat thyroid disease) show a higher risk of developing anxiety and depression compared to euthyroid patients (2).
So what can we take from this?
Well, if we know that low thyroid hormone (states of hypothyroidism) result in depression and anxiety, but we also know that women taking thyroid hormone to treat this problem still exhibit these symptoms, then the logical assumption is that perhaps they are not being treated adequately or that their depression is multi-factorial.
If their depression is the result of mistreatment or undertreatment with thyroid medication then it should go away once they are treated adequately but only if their depressive symptoms are not caused by something else.
With this in mind, let me ask you a question:
Is it more likely that most thyroid patients are walking around under-treated or that they have multiple conditions causing their depression?
The answer to this question is very complicated but it probably isn’t as important as you might think.
What’s more important is how to approach the treatment of women with thyroid disease who also present with depression.
It may be that there are a large number of women (thyroid patients) who remain depressed and anxious, despite taking thyroid medication because they are not on the appropriate thyroid medication or dose.
The standard approach to thyroid hormone management is to use T4 thyroid medications such as Levothyroxine and Synthroid and base dosing off of the TSH.
But the problem with this approach is that it does not take into account peripheral thyroid conversion or T3 levels.
If you are one of the 15% of patients who have genetic polymorphisms to the deiodinase enzyme, then using T4 thyroid medication may not be optimal for your body.
It’s possible that issues relating to thyroid conversion may be part of the reason (perhaps the primary reason) that so many thyroid patients remain depressed and anxious despite using thyroid medication.
So what are you supposed to do about it?
One of the easiest ways to approach this problem is to bypass the peripheral thyroid conversion step by adding T3 therapy to your existing dose of T4 medication.
Studies have shown that adding T3 to T4 medication is sufficient to reduce symptoms of depression and improve well-being in many patients (3).
T3 is the active and most powerful thyroid hormone and it can be given as a prescription medication that can be used either by itself or in conjunction with other thyroid medications like levothyroxine.
Other studies have shown that up to 12% of the population contains a genetic change to a specific enzyme (DIO2 polymorphism) which can limit the amount of T3 that the brain receives, which would make less effective T4 only thyroid medication (4).
Even adding as little as 5-10mcg per day of Cytomel or liothyronine may be sufficient to dramatically reduce depression symptoms in thyroid patients.
But what if you’ve tried it and it hasn’t worked or what if your physician isn’t willing to prescribe this medication?
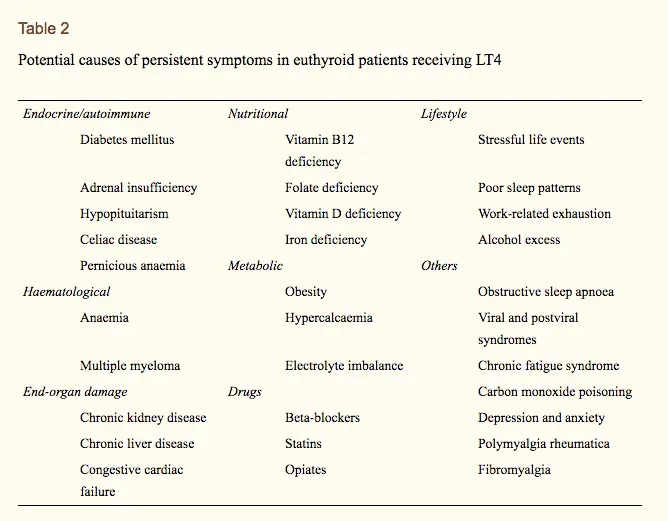
There are MANY other reasons that you may be suffering from depression if you have thyroid disease that may not be related to your thyroid.
Conditions such as vitamin B12 deficiency, iron deficiency, folate deficiency, the stress in your work life, reduced sleep or insomnia, alcohol consumption, and so on can all contribute to depressive symptoms.
For this reason, make sure that you ALSO assess these factors in addition to your existing medication.
In many cases simply altering the medication you are taking (by either adding T3 to your existing T4 dose or by switching to NDT) will likely result in a reduction in depressive symptoms (but it may not eliminate them).
Once you’ve altered your medication you can then look into other causes and treat those issues.
Hashimoto’s & Depression (& Other mood disorders)
Another subset of patients that we need to discuss is those with Hashimoto’s thyroiditis.
As you probably know, Hashimoto’s thyroiditis is an autoimmune disease that results in the slow and chronic destruction of the thyroid gland over time.
Patients with this condition may eventually go on to develop hypothyroidism due to this chronic inflammatory destruction of the gland.
The problem with this condition is that many patients with Hashimoto’s tend to experience hypothyroid-like symptoms (such as fatigue, depression, constipation, cold intolerance, and so on) despite having a so-called “normal” TSH.
Traditionally, patients who have Hashimoto’s disease and have a normal TSH are not treated with thyroid hormone medication, even if they have symptoms.
Studies have shown that patients with Hashimoto’s disease, even with a normal TSH, have an increased risk of developing both depressive symptoms and anxiety.
So what do you do if you have depression and Hashimoto’s but a normal TSH?
The first step is to closely evaluate your thyroid lab tests to determine if they are indeed actually normal.
Despite having a “normal” TSH it is still very possible to exhibit low free thyroid hormones which may be sufficient to warrant treatment with thyroid medication.
Some studies have shown a benefit to treating Hashimoto’s patients, even though they have a normal TSH (5).
It is also possible that the thyroid antibodies in Hashimoto’s may be causing depressive symptoms irrespective of their impact on thyroid function.
What does that mean?
It means that the thyroid antibodies THEMSELVES may actually be causing depression or other problems (6).
This leads us to the second step…
The second step is to look into other therapies that may help reduce total antibodies in your body.
This makes treating depression in Hashimoto’s patients more difficult because they have 2 reasons for these types of symptoms.
One is from damage to the thyroid gland and hypothyroidism and the second is from the antibodies themselves.
If you have Hashimoto’s thyroiditis and depression, then make sure you look at other therapies which may be able to calm down your immune system and help reduce the total amount of antibodies in your serum.
Therapies such as Vitamin D supplementation, the use of LDN, certain supplements, and the use of thyroid medication may help reduce antibodies and therefore treat depression.
You can learn more about these therapies here.
Using T3 Thyroid Hormone for Depression (If you don’t have thyroid disease)
Another interesting point worth mentioning here is that several studies have shown that the use of thyroid hormone, in addition to standard SSRI (selective serotonin reuptake inhibitors (7)), helps improve outcomes in patients with depression.
Let’s break this down:
Some studies have shown that patients who don’t respond to standard depression medications, such as Zoloft or Paxil, show an improved response when thyroid hormone is added to the mix (8).
Other studies have also shown that thyroid hormones, such as T3, can be used both as a stand-alone depression medication or used in combination with SSRIs as well.
So what exactly does this mean?
There isn’t enough information to draw a clear picture just based on the studies, but at the very least it indicates that there is some connection, perhaps outside of our current understanding, between your mood and thyroid hormone.
Another explanation for this connection is that there may be a large group or subset of patients walking around with the label of depression when in reality they might actually have sub-clinical hypothyroidism or hypothyroidism.
If you are a patient who has failed multiple different types of depression medications, someone who has failed medication cocktails, and so on, then it might be worth evaluating your thyroid lab tests and considering a trial run of thyroid hormone.
The thyroid medication which seems to work the best is Cytomel or Liothyronine.
This medication contains pure T3, which is the strongest thyroid hormone.
Even using small doses of T3 by itself, or in combination with SSRIs, has been shown to reduce the symptoms of depression and improve quality of life markers.
This can be done safely to minimize any negative side effects of using thyroid medication (even in those without thyroid disease) by following a series of guidelines listed below (9):
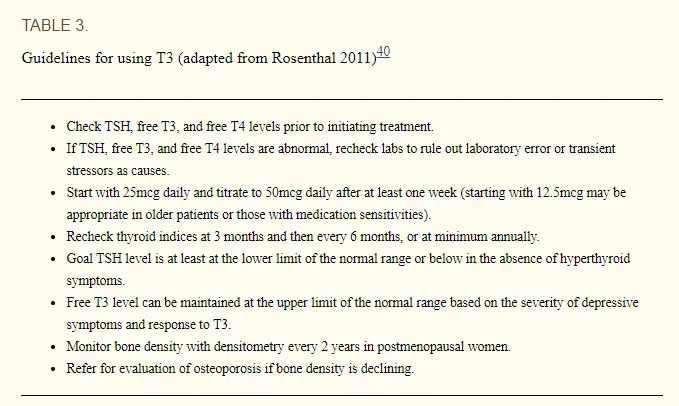
- Close monitoring of thyroid lab tests INCLUDING TSH, Free T3, and Free T4
- Slow titration of T3 starting at 25mcg and increasing based on tolerance and over a period of weeks
- Set the goal TSH at the lower limit of normal
- Maintaining Free T3 in the upper limit of the reference range
- Close monitoring of bone density with DEXA scanning in patients who are post-menopausal
- *Note: Observational studies have shown that using 50mcg to 150mcg of T3 per day does not result in negative effects on cardiac (heart) or skeletal (bone) tissues, but these studies are limited to 2 years in length.
*Note: These are similar steps that can also be used to help with weight loss in thyroid patients as well.
Another interesting point is that T3 has been shown to be effective in treating mood disorders such as bipolar disorder, even in patients who have failed multiple different types of mood-stabilizing medications (10).
This indicates that there is likely a connection between brain function, mood, and the amount of T3 in circulation in the body.
It is possible that polymorphisms in deiodinase enzymes (such as DIO2) may be responsible for reducing the total amount of T3 which enters the brain which may then trigger these symptoms (11).
This pathway can be bypassed with the use of medication such as T3 which may be superior to T4 forms of medication (for those with the polymorphism).
The science isn’t settled, but some of the work is promising, especially if depression is severely impacting your quality of life and ability to function.
In these situations, it may be worth a trial run of thyroid hormone.
What to do if you Are Clinically Depressed
We’ve gone over a lot of information in this post so let’s condense it down to your next steps:
- Check your thyroid lab panel including free thyroid hormones (Free T3 & Free T4)
- Consider adding T3 therapy to your regimen (Cytomel, liothyronine, or NDT) – Even small doses of 5-10mcg per day may help
- Treat nutrient deficiencies such as B12, folate, and iron deficiency
- Focus on reducing circulating thyroid antibodies if you have Hashimoto’s
- Treat Hashimoto’s with thyroid medication (if necessary)
- Ensure that you are sleeping 8 hours per night
- Practice stress reduction techniques (meditation)
Following these guidelines should help you get on the right track to treating any depressive symptoms you may be experiencing.
Just realize that this is not a complete list, but it can serve as a starting point for many of you.
Final Thoughts
The bottom line?
If you are suffering from depression AND you have thyroid disease AND you are on thyroid medication then you know something is not right.
If you fall into this category then you need to look at different thyroid medication alternatives, the use of supplements and nutritional vitamins, and other factors that can influence your mood.
If you don’t have thyroid disease but you do suffer from depression, then it may be time to look into alternative depression medication such as Cytomel or liothyronine.
The connection between depression and thyroid hormone is not well understood, but it seems that this connection is strong.
Now I want to hear from you:
Do you have thyroid disease? Do you also suffer from depression?
Do you still have depression despite taking T4 thyroid medication?
Have you tried T3 medications to treat your depression?
What has worked for you? What hasn’t?
Leave your comments below!