Thyroid hormone resistance gets a lot of attention from thyroid patients for one very important reason:
Because it has the potential to explain why so many thyroid patients continue to feel poorly despite taking thyroid medication and despite having thyroid lab tests in the normal range.
While this is true, the assertion that thyroid hormone resistance exists gets a lot of pushback from the conventional medical community.
The reason for this has to do with the fact that most doctors are only familiar with one type of thyroid resistance that is very rare:
The genetic type.
If you are only looking at the genetic version of thyroid resistance then, sure, it’s easy to make the case that it’s not very common and those people stating they have it, are most likely incorrect.
But if we use a broader definition or even the most correct definition, then those patients who believe they have it suddenly start to make a lot more sense.
Let’s jump in:
Is Thyroid Hormone Resistance Real?
Let’s start with the basics:
Is thyroid hormone resistance real?
Absolutely.
There are plenty of studies that show this to the be case (1).
If you look at the evolution of thyroid hormone resistance, you will see something interesting.
In the past, thyroid hormone resistance was felt to be quite common and was said to be present in patients who had a decreased metabolism despite taking thyroid medication.
Back in the old days, thyroid patients were treated based on their metabolism and not on blood tests (this was prior to the widespread availability of TSH testing).
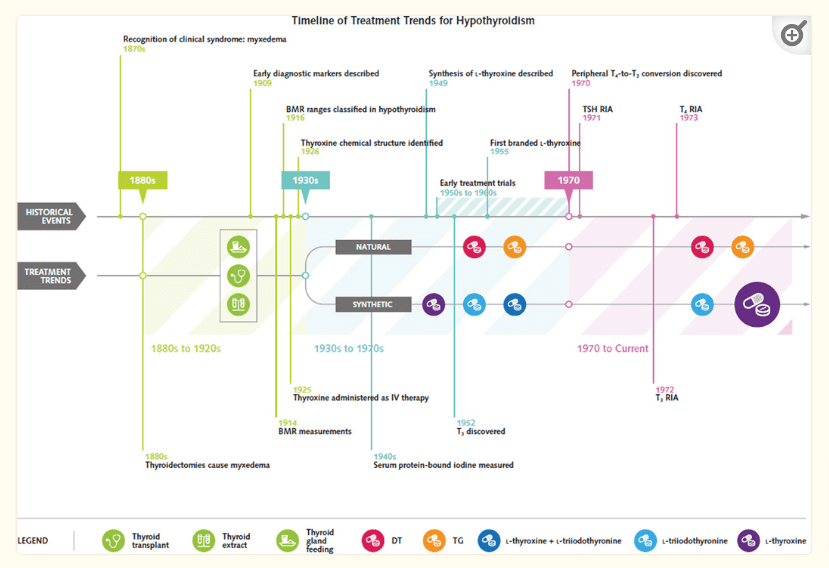
Back then, doctors would provide various doses to thyroid patients in an effort to increase their metabolism and they were said to be “treated” when their metabolisms were normalized (2).
As a practicing doctor, you could look at people and determine who would have thyroid resistance based on how much thyroid hormone they needed.
If one person needed 2 grains of NDT to normalize their metabolism and another needed 4 grains of NDT to normalize their metabolism, then you could make the assumption that the person needing a higher dose may be more resistant to thyroid hormone.
This isn’t a perfect way to assess thyroid function or thyroid resistance, by any means, but there’s still value in looking back at how things used to be.
You can compare that philosophy with how doctors think about thyroid resistance today:
And right now it’s considered a very rare condition with around 1,000 cases reported in total, most of which, are genetic in origin.
Is it really the case that thyroid resistance syndromes dropped off the face of the earth or is this a case of changing definitions?
Probably a little bit of both.
It seems like the pendulum swung from an overdiagnosing of thyroid resistance (due to the inability to accurately test for it) to an underdiagnosing (due to an overly restrictive definition).
We can probably safely assume that we are now in a period of underdiagnosing for a couple of reasons:
#1. In virtually all other hormone systems in the body, acquired hormone resistance syndromes are far more common than genetic hormone resistance.
Current experts would have you believe that this is the exact opposite of what happens for thyroid resistance (I will explain this in more detail later).
And #2. The current plight of thyroid patients suggests that something is wrong with the diagnosis and management of hypothyroidism.
You wouldn’t expect hundreds of thousands (maybe millions) of thyroid patients to be unhappy (3) if you have your treatment “figured” out.
Between these two points alone, I think we have a good argument for thyroid resistance but we don’t have to stop there.
We can just take a look at the standard definition used in medicine to diagnose hypothyroidism…
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
The Difference Between Hypothyroidism and Thyroid Hormone Resistance Syndromes
We know that thyroid hormone resistance exists, but how does it compare to hypothyroidism?
In a sense, they are actually very similar.
To better understand what I mean, let’s look at exactly how the body regulates your thyroid.
This part can get a little confusing but hang in there as it’s very important to understand:
Here’s how it works:
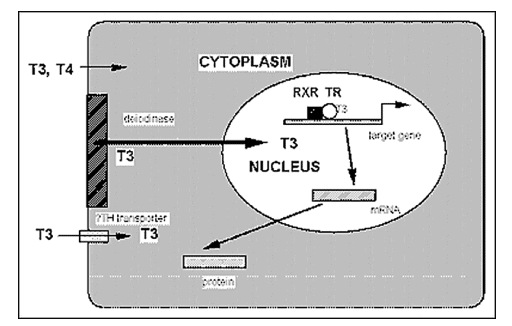
- It all starts in your brain with your hypothalamus where thyroid hormone in the bloodstream is first sensed. Depending on the amount of hormone in your blood, your hypothalamus then sends a signal to your pituitary gland in the form of TRH (a hormone).
- The pituitary gland senses the amount of TRH and releases TSH in response.
- TSH then travels through your blood to your thyroid gland (located in your neck) and responds to this stimulus by producing T4 and T3 thyroid hormones.
- T4 and T3 thyroid hormones then travel throughout your body to target cells. They could be transported from your neck all the way to your toe or to your brain or to your gut.
- Thyroid hormones must then gather around their target cells, be transported across the cell membrane, and touch specific thyroid hormone receptors.
- After doing its job in your cells, thyroid hormone then travels back to your brain via the bloodstream where it is sensed by the hypothalamus and the process continues over and over.
If you’re a little bit confused after reading this, don’t worry.
It’s not necessary for you to have this completely memorized, but to just have a basic understanding of how it works.
What you need to know is that if any of these steps are not working properly, then the end result will be a reduction in thyroid function and the symptoms of hypothyroidism.
This could happen in your brain, it could happen in your thyroid gland, or it could happen in your cells.
When it happens in your brain, we call it central hypothyroidism (4).
When it happens in your thyroid gland, we call it primary hypothyroidism (5).
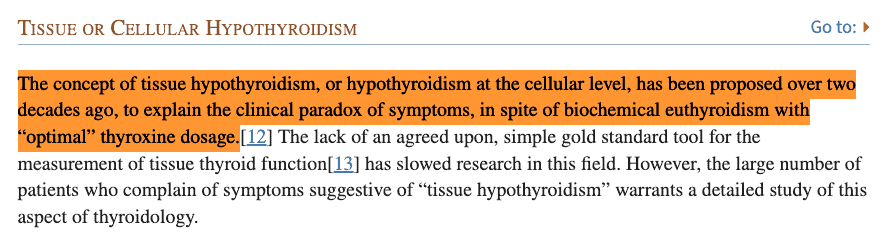
When it happens in your cells, we call it thyroid resistance or tissue-level hypothyroidism (6).
While every single case results in decreased thyroid function and, technically, hypothyroidism, each problem manifests a little bit differently and will impact your lab tests in a slightly different way.
You may have had a thyroid condition for many years and have never been made aware of these distinctions, and that’s actually not that uncommon.
The reason for this is that the most common causes of hypothyroidism result from problems with the thyroid gland directly.
The most common of these is Hashimoto’s thyroiditis which results in the destruction of the thyroid gland.
For this reason, most doctors don’t spend a lot of time testing for problems in your pituitary gland, your hypothalamus, or your cells to see if the problem is there instead.
They just tend to automatically assume if you have hypothyroidism that you must have a problem with your thyroid gland.
And this probably explains why most doctors aren’t familiar with thyroid resistance as a cause of hypothyroidism and why if you mention this condition, they will most likely give you a strange look.
But that doesn’t make it any less real or any less of a problem.
For all intents and purposes, you can think of thyroid hormone resistance as a type of hypothyroidism because it results in decreased thyroid function at the cellular level.
This means it’s just as important of a cause as something like Hashimoto’s, even though it’s different in terms of what causes it and how it manifests.
The Two Most Common Types of Thyroid Hormone Resistance:
Now that we know that thyroid hormone resistance is real and how to define it, let’s look at the two causes.
As I mentioned above, the cause that doctors think about when they think of thyroid resistance is the genetic version but I think that the acquired version is much more important and relevant for the average thyroid patient.
I think you will understand why as we go through these causes.
#1. Genetic Thyroid Hormone Resistance
Genetic thyroid hormone resistance syndromes are very rare.
This subgroup of thyroid resistance is not as interesting as the acquired version (which we will soon talk about below) simply because it’s so uncommon.
The exact prevalence is not really known probably because there are several different genetic variants of the disease and each presents in a different way.
The most common figure I’ve seen reported is that genetic thyroid resistance syndromes may be seen in as high as 1 in 40,000 live births (7).
All of these conditions have one thing in common:
Genetic mutations result in varying degrees of cellular resistance to thyroid hormone.
In many cases, this results in very high levels of free thyroid hormones that the body produces to try and push through some thyroid function.
You would expect the presence of high levels of free T4 and free T3, but what’s unexpected is that these levels are often accompanied by normal or high TSH levels (8).
These patients also tend to be very unresponsive to normal doses of thyroid hormone (not very surprising if you understand thyroid function).
There’s probably a fair amount of these patients who run through life without having any issues and their problems are only known if their thyroid function is accidentally tested for some reason.

In those people who have true genetic thyroid resistance, the effects are hard to miss if thyroid problems arise.
These patients may need doses of T4 as high as 500mcg to 1,000mcg per day (9)!
For reference, most hypothyroid patients do well on doses of levothyroxine and Synthroid in the range of 50 to 150 mcg per day.
This means genetic thyroid resistance creates an environment in which you need doses of about 5-10x that of normal to obtain normal thyroid function.
But I would say that this type of thyroid resistance is an anomaly and most of you reading this are more likely to have what I refer to as acquired thyroid resistance.
#2. Acquired Thyroid Hormone Resistance
Understanding that genetic thyroid resistance exists is important because it can help us better understand acquired thyroid resistance which is probably far more common than most people think.
I say that because, in general, acquired hormone resistance syndromes are always more common than their genetic counterparts.
Take for instance insulin resistance.
Acquired insulin resistance is incredibly common and is seen in some form or fashion in up to 40% of the population in the United States.
Acquired insulin resistance stems from the overconsumption of carbohydrates and sugars.
Genetic insulin resistance syndromes, by comparison, are far less common.
The same logic applies to other hormone resistance syndromes such as progesterone resistance from estrogen dominance disorders (10), leptin resistance from weight gain (11) and repeat dieting, and cortisol resistance from chronic stress (12).
Physiologically speaking, doctors accept that the acquired versions of hormone-resistance syndromes are always more common than the genetic versions except in the case of the thyroid.
My personal opinion is that this probably has more to do with our lack of understanding of thyroid resistance than the reality that it doesn’t exist or that it’s rare.
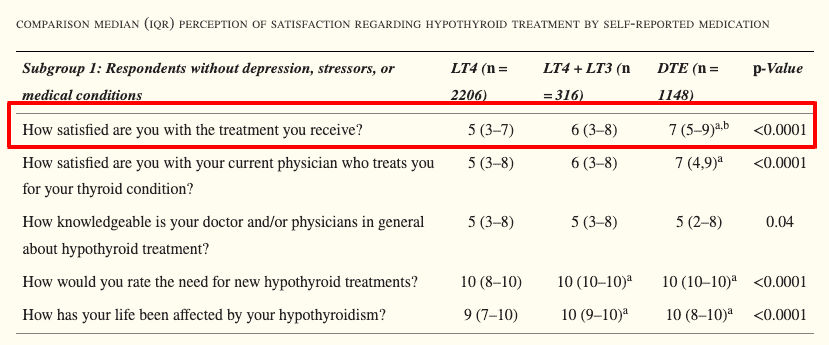
I say that because there’s a lot of real-world evidence to suggest that many thyroid patients are suffering from what looks like acquired thyroid resistance (13).
This is reflected in how thyroid patients perceive their thyroid treatment which is not very well.
Whenever thyroid patients are polled, they continually express concern about thyroid management, lingering symptoms despite having normal thyroid lab tests, and so on.
In other words, it doesn’t look like we have the whole thyroid dilemma solved simply by looking at the current state of thyroid patients.
If acquired thyroid resistance exists, and I believe that it does, then how would it manifest?
It would be very similar to genetic thyroid resistance but would vary in intensity and severity.
In other words, we would see thyroid patients walking around with the following attributes:
- Some thyroid patients would do well on thyroid medications like levothyroxine and Synthroid but we would not expect standard doses to work for everyone. Some thyroid patients would need very high doses of these medications, probably in the range of 150 to 300mcg (less than genetic thyroid resistance but higher than normal).
- Some thyroid patients would require higher doses of T3-containing medications such as natural desiccated thyroid or compounded thyroid medication.
- Even more extreme, some thyroid patients would require T3-only thyroid medications like Cytomel and liothyronine. And they may even require higher doses than what would be considered “normal” physiologic doses.
- Some thyroid patients would have thyroid lab tests that look normal but still remain symptomatic because even though there is a sufficient amount of thyroid hormone in circulation, the cells are not responsive to it. This would create a scenario in which labs look normal but thyroid patients would still feel hypothyroid.
- We would expect lifestyle changes to improve thyroid hormone function which would then reduce the need for thyroid medication. For example, if you lost weight, reduced stress, replaced nutrient deficiencies, and cleaned up your diet, then your need for thyroid hormone might fall.
Does this sound like the current situation that thyroid patients find themselves in? I think it does.
And it’s not that farfetched of an idea to think that the majority of the problems thyroid patients currently face might be caused by acquired thyroid resistance syndromes.
Obviously, we need a lot more research and testing to determine if that’s the case, but discussing it like this is a good start.
How to Tell If You Have Thyroid Resistance
What should you do if you believe you have thyroid resistance? Are there any tests that you can use to help you determine if that’s the case?
Sort of, but not exactly.
Right now we don’t have any solid tools that can be used to diagnose thyroid resistance but there are some things you can test for to make an educated guess if it’s present.
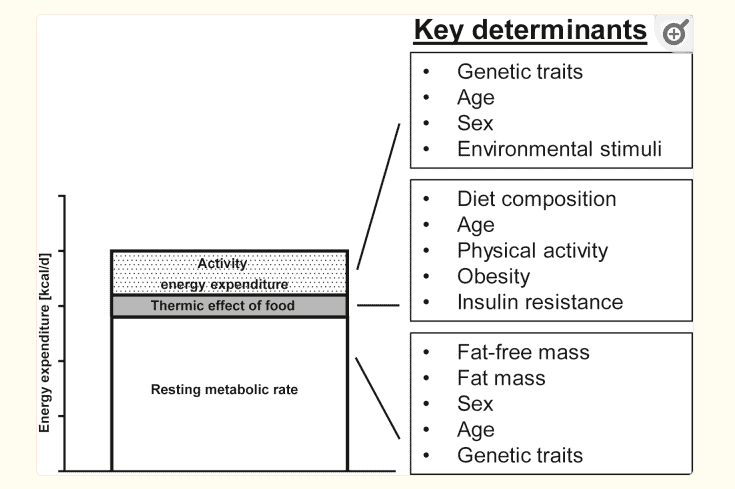
One of those tools is the assessment of your basal metabolic rate or metabolism.
The idea behind assessing your metabolism is simple:
If you can compare your basal metabolic rate to someone that is the same age as you but with normal thyroid function, then you should get a fairly good idea of where you would need to be if your thyroid was normal.
Imagine you are a 45-year-old woman taking levothyroxine who burns 1,600 calories per day.
If you knew that women your age without thyroid problems burn 1,900 calories per day then you could take thyroid hormone until you approached that number.
This method would be used in place of using thyroid lab tests to determine when you are “normal”.
The degree of thyroid hormone resistance would be made manifest depending on how much thyroid hormone you needed to get there.
I just used a 45-year-old woman as an example here but you could replace gender and age with whatever suits your personal situation.
This theory originates on the basis that thyroid hormone is the primary regulator of your metabolism (14).
While this is true, it’s not the only regulator of your metabolism which leaves some room for errors when using this method.
I happen to think this is a great option, though, if you have a way to measure your metabolism easily.
Another option would be to look at your thyroid lab tests in conjunction with your thyroid symptoms.
The standard approach to thyroid management places the primary emphasis on your lab tests, specifically your TSH.
If your TSH is normal, then you are considered to be normal, regardless of how you feel.
An opposite approach would be to focus solely on your symptoms and neglect your thyroid lab tests.
In other words, you would take thyroid medication until you felt normal.
Neither option is ideal as they both are on the extreme.
A better approach is to use a combination of both your thyroid symptoms and your thyroid lab tests.
Ordering tests like your free t3, free t4, and reverse T3 will allow you to better understand how well your body is converting thyroid hormone, how much T3 is available for your cells to use, and whether or not your body is using that T3.
Using the combination method of lab tests and symptoms allows you to feel better while avoiding the need to suppress your TSH to produce supraphysiologic thyroid levels.
These are the levels you want to avoid because they do come with some minor risks.
Practically speaking, this may mean thyroid medication pushes your TSH to be flagged as low but not as suppressed (there is a big difference between these two states and what it means for your body!).
Again, much like the metabolism testing method, this isn’t perfect, but it can definitely work.
Your goal should be to find a balance between how you are feeling (complete symptomatic control) and the risks that getting there may impose on your overall health.
You may be willing to accept a small risk of bone loss from lowering your TSH, for instance, if it means you have the energy you need to live your life, obtain a more normal weight, and regrow your hair.
I’m not here to make that decision for you, just to help better understand how you should think about the situation.
Final Thoughts
We are learning more and more about thyroid hormone resistance syndromes every year.
My suspicion is that as research continues, we will find out that acquired thyroid hormone resistance is much more common than doctors originally believed!
I think that eventually it will be recognized as perhaps one of the major reasons that thyroid patients have been struggling for the last several decades and may explain the unresponsiveness of some patients to medications like levothyroxine and Synthroid.
Right now we don’t have any solid ways for testing for thyroid resistance, but there are a handful of methods that can work.
If you don’t feel like waiting for the research to catch up, then you can try testing your metabolism or treatment based on thyroid medication that takes into account both your thyroid symptoms and thyroid lab tests like free t3, free t4, and reverse T3.
Now I want to hear from you:
Were you aware of thyroid resistance as a condition? Is this the first time you’ve heard of it?
Do you believe that you currently have thyroid resistance? If so, what makes you think so?
Do you have other hormone resistance syndromes like leptin resistance, insulin resistance, or cortisol resistance?
Are you planning on making any changes to your thyroid medication to try and compensate for these issues?
Keep the conversation going by leaving your questions or comments below!
Scientific References
#1. pubmed.ncbi.nlm.nih.gov/18940949/
#2. ncbi.nlm.nih.gov/pmc/articles/PMC4980994/
#3. ncbi.nlm.nih.gov/pmc/articles/PMC6916129/
#4. ncbi.nlm.nih.gov/pmc/articles/PMC3169862/
#5. ncbi.nlm.nih.gov/pmc/articles/PMC3931439/
#6. ncbi.nlm.nih.gov/pmc/articles/PMC3169863/
#7. ncbi.nlm.nih.gov/pmc/articles/PMC4790576/
#8. ncbi.nlm.nih.gov/pmc/articles/PMC2928892/
#9. ncbi.nlm.nih.gov/pmc/articles/PMC2928892/
#10. pubmed.ncbi.nlm.nih.gov/28423456/
#11. ncbi.nlm.nih.gov/pmc/articles/PMC6354688/
#12. ncbi.nlm.nih.gov/pmc/articles/PMC3341031/
#13. pubmed.ncbi.nlm.nih.gov/17383828/
#14. ncbi.nlm.nih.gov/pmc/articles/PMC4044302/