The standard of care is to place all pregnant women on T4-only medications such as levothyroxine or Synthroid.
But what happens to women who are taking thyroid medications which contain T3 when they become pregnant?
What about women who are already doing well on medications that contain T3 and want to become pregnant?
We are going to explore the topic of using T3 during pregnancy and talk about safety, the preferences of most doctors, why using T3 probably poses little threat to your baby and more.
How Doctors Look at Pregnancy and Thyroid Medication
We are going to talk specifically about using T3 if you are pregnant but first, we need to talk about some of the basics.
Is it safe to use thyroid hormone if you are pregnant?
The answer to that is yes, it is definitely safe to take thyroid medication during pregnancy.
In fact, if you don’t take thyroid medication (and you are hypothyroid) then you are putting your baby at an increased risk of birth defects (1), pregnancy complications (2), and a decreased IQ after birth (3).
The good news is that virtually all of these consequences can be avoided by simply restoring your thyroid to normal function with the use of thyroid medications that contain thyroid hormones.
Thyroid hormone is incredibly important to the development of your child which is why all pregnant women should have their thyroid checked.
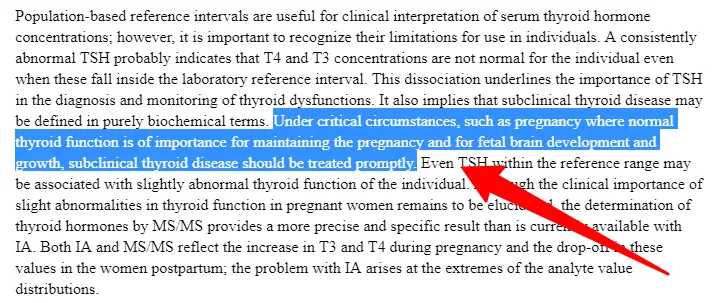
This is also why there are very strict guidelines (4) when it comes to managing thyroid lab tests during pregnancy.
The guidelines used by doctors (yes, even endocrinologists) are much more strict compared to the guidelines that are used for non-pregnant women.
For instance, a TSH greater than 2.5 mU/L would be considered bad in a pregnant woman (5) and a reason to start thyroid medication (some studies even recommend that this occurs in women who have no symptoms of hypothyroidism).
A TSH between 2.5 and 5.0 mU/L in a non-pregnant woman (6), on the other hand, would most likely be dismissed away by the same doctor.
So, yes, managing your thyroid is incredibly important during pregnancy and may require the use of thyroid medication.
And this is where our story starts.
What thyroid medications can you use? Are all types of thyroid medications safe during pregnancy? What kind of lab tests do you want to look for if you are pregnant and taking medication?
When conventional doctors (think about your ob/GYN, your endocrinologists, or your PCP) treat pregnant women who are also hypothyroid, they are really only looking at a few things:
#1. What medication you are taking and your dose.
Conventional wisdom is to place ALL patients on T4-only thyroid medications when they are pregnant and dose this medication based on the TSH.
This means that if you are not taking any thyroid medication, but your TSH is higher than the 2.5 mU/L I mentioned previously, your doctor will most likely recommend that you start taking levothyroxine or Synthroid.
And, if you are already taking some thyroid medication that contains T3 (such as Nature-throid or NP thyroid), your doctor will make the recommendation that you switch to T4 instead of T3.
This is the standard. To be on T4-only thyroid medication if you are pregnant.
#2. Your TSH and what level it is.
Your doctor will also want to regularly check your TSH (which stands for thyroid-stimulating hormone) to ensure that your TSH does not rise above 2.5 mU/L (or below 0.1 mU/L).
Your medication will be adjusted based on this level.
This is considered the standard or conventional care (7) and, while you should be aware of it, you should also be aware that there may be other potential options (including my own view of treating hypothyroidism).
Which is what we are going to talk about next.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Can T3 Be Used During Pregnancy?
And this is where our story continues.
What if you are someone who is already taking medication that contains T3 prior to pregnancy?
What if you are doing well on that medication and you don’t want to change?
Will staying on your medication actually cause harm to your baby?
These are very important questions so let’s tackle them one by one and use scientific studies to back up our conversation.
First off:
Is it possible to use T3 during pregnancy?
Yes, it is possible to use T3 medications if you are pregnant.
The question is not whether or not they can be used but how safe they are when used during pregnancy.
And in regards to that question, we don’t have much in the way of scientific data to help us out.
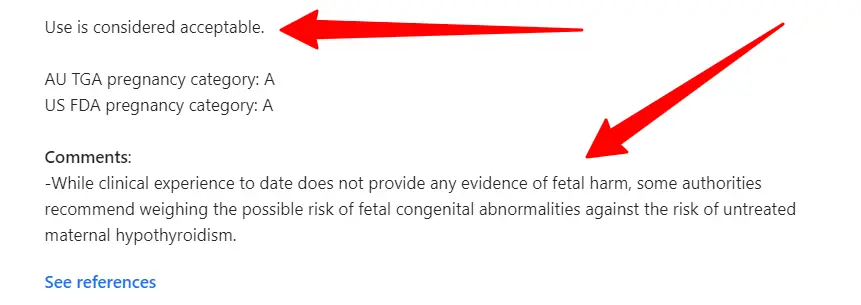
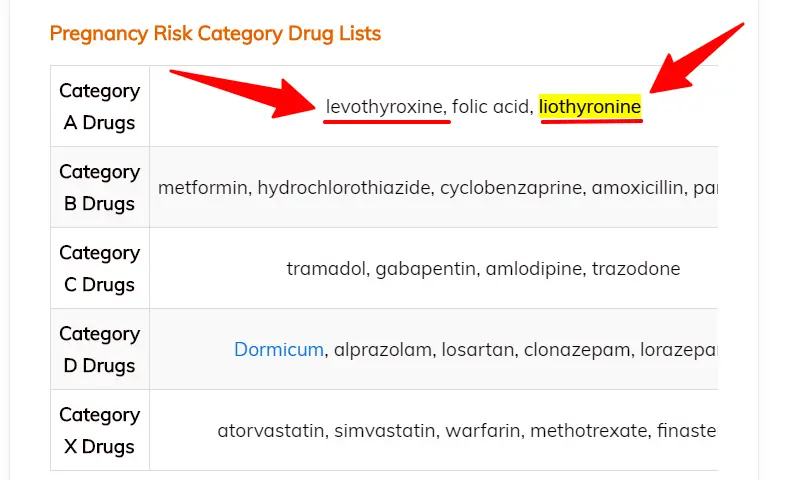
All we know is that liothyronine (which can be used as a proxy for all T3 medications) doesn’t seem to cause any harm to the fetus (and would be classified in the same category as levothyroxine in terms of safety).
And, at this point, all we have are theoretical dangers (8) that have not been substantiated by real-world clinical studies.
I have included a variety of studies below which discuss this topic in more detail so feel free to jump there if you want more information.
What if you are currently taking thyroid medication and then you become pregnant?
In most cases, and as long as you are not overmedicating yourself, it’s probably best to stay on whatever medication you are using prior to becoming pregnant.
Changing just opens you up to new problems and with thyroid management being so important in early pregnancy, it’s probably not wise to make big changes to the type of medication you are using.
We do know, however, that most women need to up their dose of thyroid medication once they find out that they are pregnant.
This stems from the fact that you must start providing thyroid hormone to both the growing baby and yourself.
So the general rule is to increase how much thyroid hormone you are taking once you find out you are pregnant.

I do find, however, that this is typically not an issue for patients under my care.
Most likely because they are already optimized prior to pregnancy (or perhaps taking slightly more than necessary) which means they don’t need much in the way of dose adjustments.
Will staying on your medication harm your baby?
The medication itself is not likely to cause any harm to your baby directly.
In fact, we have information directly from the FDA (9) stating that “Cytomel should not be discontinued during pregnancy” to imply that if you are using it prior to pregnancy there’s probably no benefit in discontinuing your medication.
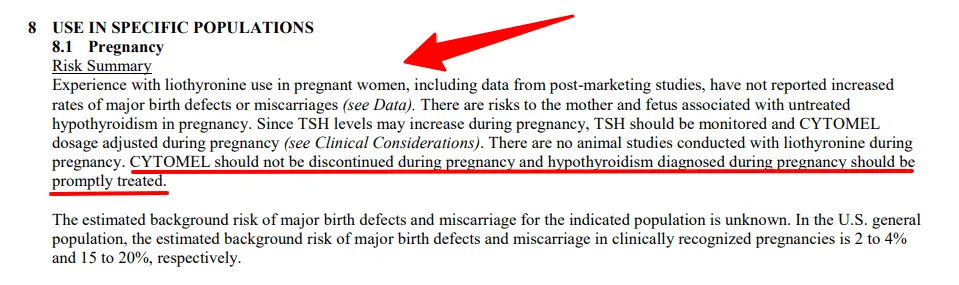
Instead, if there is to be any harm, it’s going to stem from your dose of thyroid medication.
The same information from the FDA states that “There are risks to the mother and fetus associated with untreated hypothyroidism”.
The point here is that it matters less what type of medication you are taking and more that you are actually treating the condition.
If you take too much Synthroid (enough to cause hyperthyroidism) then that will cause a problem.
Just like taking too much of T3 can cause similar issues.
But the problems stem from the hyperthyroid state (10) and not the medication itself.
As long as you follow your labs (more information below) you shouldn’t have any major issues in this area.
What are the differences between T4 and T3 medications?
The reason that most doctors prefer to use T4 over T3 is that T4 is considered to be more ‘stable’ in the bloodstream.
T4 has a much longer half-life compared to T3 (11) which means that it stays in your system longer.
This makes sense given that T3 is the active form of thyroid hormone and is also the most powerful.
But just because it is used rapidly by the body and because it has a shorter half-life means that it needs to be avoided.
A combination of T4 + T3 (such as levothyroxine + liothyronine) can be used to get the best of both worlds.
You can maintain a steady level of T4 supply in the bloodstream and still gain some of the more rapid benefits of smaller T3 doses as well.
Which thyroid medications contain T3?
There are many thyroid medications that contain T3 but most doctors shy away from using them.
Medications that contain T3 include:
- Liothyronine
- Cytomel
- SR T3
- NP Thyroid
- Armour thyroid
- WP thyroid
- Nature-Throid
An Example of Using T3 During Pregnancy
If you’ve read some of my other articles you know that I will occasionally share lab results from patients that I am treating.
I want to do the same here, but these lab results are from my wife who has been taking T3-only thyroid medication (Cytomel) for her last 2 pregnancies.
But a word of warning:
Just because this treatment has worked for her doesn’t automatically or necessarily mean that it is right for you.
She has been taking T3-only thyroid medication for several years in order to treat hypothyroidism in addition to metabolic damage from an eating disorder early in her life as well as treatment-resistant depression (resistant to anti-depressants but responsive to T3).
Her liothyronine dose has ranged from 12.5mcg up to 50mcg per day (depending on a number of factors), but for pregnancy, we tend to keep the dose between 12.5mcg per day and 25 mcg per day.
She is currently in her third trimester and we recently checked her labs which you can see below:
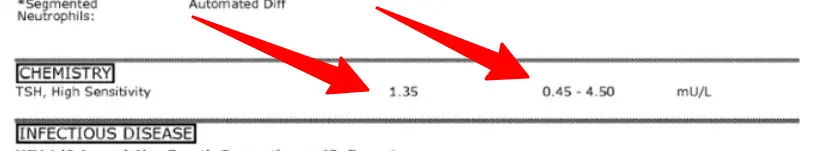
Her TSH is currently reading at 1.35 mU/L and you can see the reference range at 0.45 – 4.50 mU/L.
The normal range should really read between 0.2 and 2.5 mU/L based on studies, but lab companies don’t always differentiate between pregnant and non-pregnant women making it important for you to know about this on your own.
Her labs are perfectly within the normal range for pregnancy using a T3-only medication.
I feel comfortable using this medication on her because it has worked for her for many years, both before she was pregnant and during her last two pregnancies, and she hasn’t experienced any negative side effects thus far.
A couple of things to note about her labs and case:
- Advanced thyroid lab tests are not always helpful during pregnancy – If you notice, I didn’t order free thyroid hormone levels. These aren’t always required (but I almost always order them in non-pregnant patients) due to how pregnancy influences blood volume and free thyroid levels. If you have an abnormal TSH, or if you are experiencing hypothyroid symptoms with a normal TSH then it would be a good idea to get these.
- Your TSH is much more important when you aren’t pregnant than when you are – Following your TSH during pregnancy is much more helpful compared to when you are not. Again, this has to do with the fact that pregnancy impacts both blood volume and thyroid lab tests making them less reliable compared to the non-pregnant state.
- Her TSH is not suppressed while taking T3 – It’s a common misconception that TSH must be suppressed when taking T3-containing medications. This doesn’t automatically occur and doesn’t always have to occur.
As I said, this example doesn’t mean that you should use T3, but I did want to provide you with a study of someone who has used T3 for two pregnancies without any issues.
I also have many other experiences in treating patients with NDT formulations (such as WP thyroid and Nature-throid) who have used these medications during pregnancy without any issues.
These are all anecdotal experiences, however, and not scientific in nature so keep that in mind.
I definitely wouldn’t give my own wife T3 if I thought that it was dangerous, however, which is why I shared this example.
Is T3 Safe to use if you are pregnant and have Hypothyroidism or Hashimoto’s?
When deciding whether or not to use T3 you should be aware that there are no studies available that definitely show that T3 is harmful to your baby.
On the other hand, there are also no studies that show that T3 is beneficial or can replace T4 during pregnancy either.
This puts you, as a pregnant woman, in a bit of a pickle when deciding what route you should go.
I don’t think it makes sense to automatically think that you need to take T4 medication if you are pregnant, however.
One of the main reasons that we don’t have a lot of studies on medications in pregnant women is that it’s very difficult, and sometimes dangerous, to do these studies.
But just because they don’t exist doesn’t mean that we can’t make assumptions or assertions about how you might do if you were to use T3 medication.
We know, for instance, that many patients around the world do better on a combination of both T4 and T3 (12), especially in the setting of DIO2 genetic defects.
Right away this tells us that there are some people, estimated between 10 and 20% of the population (13), who are not able to utilize T4 as well as others.
This would be encouraging for pregnant women who fall into this category and may need to consider using T3.
In addition, we also know that your own thyroid gland produces a combination of both T4 and T3 when it is healthy and functioning properly.
That production is approximately 80% T4 and 20% T3 (both from direct production and peripheral conversion).
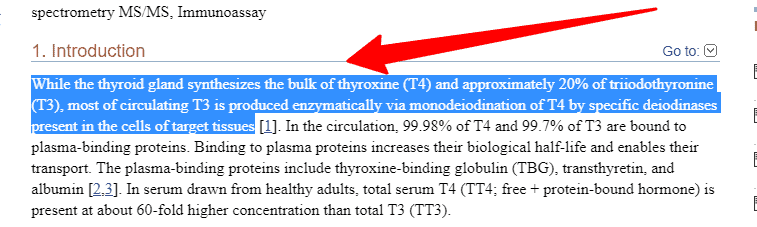
The assumption could be made that if the healthy thyroid gland produces T3 on its own, even during pregnancy, using an exact replica of that hormone as a medication replacement might also be safe.
Lastly, we know that thyroid lab tests can be assessed and evaluated during pregnancy to ensure that enough thyroid hormone is entering the cells and is sufficient for the fetus.
We can look at factors such as TSH and free thyroid hormone levels to ensure that this is the case.
It’s also possible to evaluate your thyroid tests using isotope dilution tandem mass spectrometry (14) over the standard immunoassay.
This method of lab testing provides a more accurate view of free thyroid hormone levels compared to the immunoassay which can miss cases of biochemical hypothyroidism.
In my opinion, and based on this information, there is a place for the use of T3 medications in pregnant women.
Thyroid Lab Testing when using T3
Pregnancy causes physiologic changes in women and these changes alter how you should look at your lab tests.
The image below illustrates some of these changes:
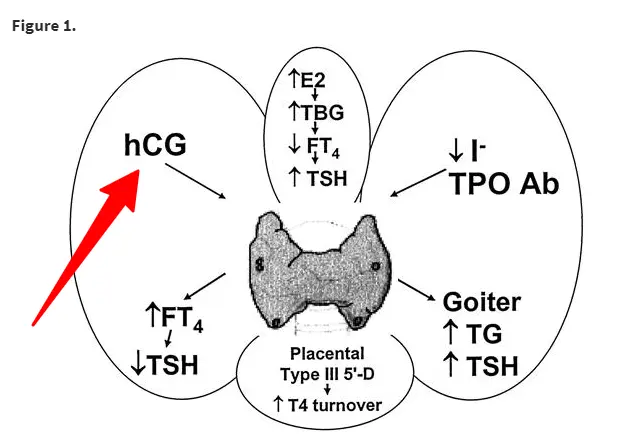
- Iodine consumption increases (your body needs more iodine).
- Thyroid hormone production increases (to compensate for you AND your baby).
- Serum thyroxine and serum triiodothyronine (T4 and T4) increase
- Blood volume increases by 50% (15) (which can lower blood pressure and dilute the concentration of certain factors).
- Thyroid hormone-binding globulin increases.
- Free thyroid hormone levels remain unchanged.
- The fetal thyroid produces T4 but converts that T4 into reverse T3.
- An increase in hCG which may have thyroid stimulatory effects (hCG comes from the placenta).
- *Despite changes to T4, T3, and binding globulins, free thyroid hormone levels remain unchanged.
What’s important here is that these are all things that change once you are pregnant and they all have an impact on how you want to look at your labs.
These changes may be one of the reasons why many doctors prefer to look only at TSH but it should be noted that your free T3 and free T4 levels should not be dramatically altered even with the changes in blood volume and thyroid binding globulins.
If you elect to use T3 then you should be evaluating free T3 and free T4 in addition to your TSH.
I recommend following the TSH guidelines set forth by the USPSTF (16):
- First trimester TSH: 0.1 – 2.5 mIU/L
- Second trimester TSH: 0.2 – 3.0 mIU/L
- Third trimester TSH: 0.3 – 3.0 mIU/L
If you’ve read any of my other blog posts then you probably know that I have my own set of guidelines that I follow but I really believe that these guidelines are decent.
The guidelines outside of pregnancy are another story entirely, but these guidelines do allow for optimization toward the lower end of the reference range in regard to TSH.
You could easily dose your medication (whatever you elect to take) to optimize your TSH in the bottom area of that reference range.
Most TSH lab tests will flag a TSH under 0.45 mIU/L as “low” but these lower levels would be accepted as “normal” under the guidelines listed above.
In fact, you could optimize your TSH between 0.1 and 0.44 mIU/L in the first trimester of pregnancy (read more about this idea here) which would technically be low outside of pregnancy but which would be perfectly normal during pregnancy.
This distinction is very important for you to understand, especially if you have a more advanced understanding of thyroid lab tests compared to most people.
I see a number of women who wrongly believe they need to push their lab tests to non-pregnant levels which may put them at more risk than any minor benefit they may be received by doing so.
In addition to testing for TSH, you will also want to look at both free T3 and free T4.
The reference ranges provided for these should be somewhere in the middle of the reference range (this will vary based on labs).
Outside of pregnancy I typically like to see these a little bit higher, but it’s safer in the pregnant state to keep them in the middle to avoid accidental overdosing or underdosing which can have negative consequences on the fetus.
Yes, you might experience slightly more fatigue than if your lab tests were more optimized but those small gains are probably not worth any increased risk.
Final Thoughts
There are situations where it may be a good idea to consider using thyroid medications that contain T3 if you are pregnant.
You should be aware, however, that this idea currently runs against conventional medical care.
But as we break down the logic behind the current treatment paradigm, it’s clear that these guidelines err more on the side of being conservative as opposed to erring on the side of safety.
There are many women who have successfully
Perhaps more important than what type of medication you are using is the DOSE that you are using.
It would be possible to overdose, or take too much thyroid medication when using ANY type of thyroid medication.
It is possible that due to how powerful T3 is compared to T4 that T3 may be more likely to cause side effects of excess thyroid hormone.
Now I want to hear from you:
Are you pregnant or thinking about getting pregnant and wondering what you should do with your thyroid medication?
If so, which way are you leaning? Which medication are you currently using?
If you have successfully gone through pregnancy using a T3 medication please share your experience below!
If you have any other questions or comments please leave them below as well.