Are you a thyroidectomy patient struggling to feel better after your thyroid removal?
If so, then this article may help to explain why you are feeling the way that you do.
Article highlights:
- Those without a thyroid are in a unique situation which is different from other thyroid patients.
- Up to 20% of those without a thyroid do not achieve normal free thyroid hormone levels on standard medications such as levothyroxine.
- This reduction in free thyroid hormones can be tested for by looking at the free T3 and free T4 levels.
- Using other thyroid medications, such as Cytomel and liothyronine, may improve this problem.
The Unique Situation of Thyroidectomy Patients
Today I want to focus on a special group of thyroid patients, namely those without a thyroid.
If you fit into this category then you know that even though you are technically still hypothyroid you are still in a ‘class’ of your own.
Those people who don’t have a thyroid find it more difficult to lose weight, find it harder to normalize their symptoms, and overall struggle with a more intense version of hypothyroidism.
And, by the way, the information in this article is relevant to ALL people who do not have a thyroid.
This includes people who have had their thyroid removed through surgical means, it includes those born without a thyroid, it includes those who have had their thyroid ablated from RAI, and it includes those with end-stage Hashimoto’s thyroiditis.
But, back to the question at hand, why are these thyroid patients so much different from those who have a sub-optimal but still functional thyroid gland?
It has to do with the combination of hormones that the thyroid gland produces in a healthy state.
Under healthy and normal conditions, your thyroid produces a combination of both T4 and T3 thyroid hormones.
Even patients who have a sluggish thyroid are still able to produce at least SOME of both of these hormones which are then supplemented by thyroid medication.
But people without a thyroid are not able to produce EITHER of these hormones. And these patients often only receive T4 only thyroid medication.
So, in effect, they are losing two thyroid hormones and only replacing those lost hormones with one.
And, it turns out, this is a big problem for up to 20% of patients who do not have a thyroid gland.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
T4 Therapy Does Not Always Normalize Free Thyroid Hormone Levels
The study I want to focus on for this article can be found here (1).
Among the many important points illustrated by this study is the fact that it showed a certain sub-group of patients without a thyroid are not able to maintain normal free thyroid hormone concentrations with T4-only thyroid medication.
If this sounds confusing to you, don’t worry because we are going to break it down into simple understandable terms.
As a patient without a thyroid, you are probably aware that you need to be on thyroid medication for the rest of your life.
The medication you are probably taking is either levothyroxine or Synthroid as these are the most commonly prescribed medications to treat this condition.
Both levothyroxine and Synthroid contain thyroid hormone but they only contain T4 which is considered the inactive thyroid hormone.
This study showed that up to 20% of patients without a thyroid who are taking these medications are not able to reach the normal healthy levels of thyroid hormone seen in normal controls.
And this promotes a big problem, especially for the 20% of people who fit into this category.
It means that this sub-group of patients will likely experience persistent symptoms of hypothyroidism despite being treated “adequately”.
Understanding the Connection Between TSH and Your Symptoms
As a thyroid patient, you are probably well aware of the thyroid lab test known as the TSH.
You’ve probably been told that this is the most sensitive and best marker for assessing thyroid function.
And while this may be true for some people, it’s not true for all people.
While TSH can be a helpful marker of thyroid sensitivity in the body, it’s certainly not a perfect test.
And relying upon your TSH as the only marker of thyroid function may lead to inappropriate treatment.
In fact, the study that I mentioned previously helps to break down and compare how your free thyroid hormone levels fluctuate based on your TSH level if you don’t have a thyroid.
It also compares these values to those of “normal” healthy adults with a functioning thyroid gland.
This information really helps to visualize the difference in thyroid conditions and highlights the importance of measuring other thyroid hormones such as free T3 and free T4.
Let’s take a look at this image from the study first:
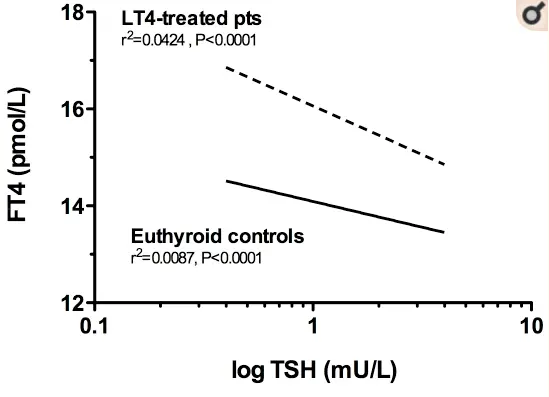
Here you can see the TSH on the X-axis and the FT4 on the Y-axis.
The dotted line represents patients who are being treated with LT4 (which is another name for levothyroxine or Synthroid) and the solid line represents healthy adults.
As you might suspect, as you take more thyroid medication by mouth you would expect your free T4 level to increase and your TSH to decrease.
This is perfectly normal and that is exactly what we see here.
In fact, we see that patients who take T4 medication by mouth actually have a higher free T4 level than those who do not take thyroid medication.
This might seem surprising to you, and you may even think that it’s a good thing, but it isn’t once you understand the function of T4 in your body.
T4 only has potential and hardly has any activity by itself (2).
In order for all of that free T4 in your body to be utilized, it MUST be converted into the active thyroid hormone known as T3.
In order for this to happen your body must take and convert it in a process known as peripheral thyroid conversion.
It’s okay for your free T4 to be high, but only if your free T3 level is also high.
If that were the case then we would be happy and we would expect that you would probably feel well and good.
But that isn’t what we see at all:
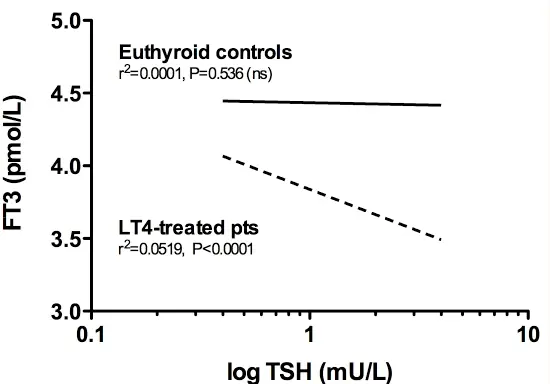
This graph is similar to the other one except on the Y-axis is FT3 or free T3.
In addition, we also see a much different pattern here compared to the free T4 graph.
Here we see that as TSH drops (meaning the more medication you take) the free T3 level increases but it never actually approximates the healthy levels seen in controls.
What does this mean?
It means that a large percentage of patients without a thyroid is not able to adequately utilize the thyroid medication that they are taking by mouth.
The thyroid hormone that they are taking is being absorbed in their intestinal tract, it’s being taken through the blood to the pituitary gland, and it’s even helping to reduce the TSH but it is NOT being converted into the active T3 thyroid hormone.
And T3 is really the only thyroid hormone that we care about because it has all of the biological activity (3).
Put another way:
There seems to be a blockage or something preventing the body from taking the T4 that you are ingesting by mouth and activating it by the body.
And, if you think about it, this makes perfect sense.
After all, why does your body produce both T4 and T3?
There must be an important reason and it probably has to do with the fact that not everyone can function well on one type of thyroid hormone.
The good news is that this appears (so far) to only be a problem for roughly about 20% of patients without a thyroid but it is a big problem for those people.
Symptoms Indicating Your Medication May Be Insufficient
How do you tell if you are among that 20% (or so) of patients without a thyroid who are not doing well on the “standard” treatment?
It’s actually fairly easy and that’s exactly what we are going to discuss now.
For starters, perhaps the easiest way to identify whether you fit into this category has to do with your thyroid lab tests.
If you are someone who doesn’t have a thyroid (because it has been removed or because you were born without one or because it has been destroyed with radioactive iodine) then you should be paying close attention to your lab tests.

But not just the standard lab tests such as TSH as this will not give you the information you are looking for.
At a minimum, you should be looking at TSH in conjunction with both free T3 and free T4.
Remember:
These free thyroid hormones may be the only sign that your body is having trouble converting T4 into T3 so you must check for this.
If you find that your TSH is “normal” (this will typically be defined in various ways by your physician but most physicians agree that a TSH between 1.0 and 2.0 is “normal”) and if you find that your free T3 and free T4 are low then you likely fit into this situation.
But how do we define a low free T3/free t4?
The study listed above helps to define this range but basically, you should be looking for these values to match those found in healthy adults with a functioning thyroid.
If you find that your free t3/free t4 are in the bottom 30% of the reference range or even off the charts low, then this is a problem.
Let’s use an example to help drive this point home:
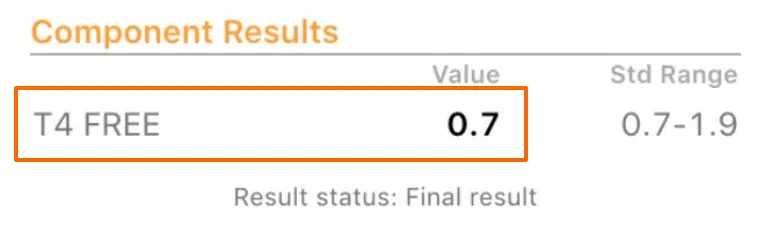
The image above is an example of a free T4 level from a patient of mine.
You can see here that her result is 0.7 while the actual range is 0.7 to 1.9.
Her 0.7 value does fall within the “normal” range but you can clearly see that she is at the very bottom of this range.
Using the reference range of 0.7 to 1.9 and the 30% optimal range I gave you above, you can see that any free T4 value that falls within 0.7 and 1.06 would be considered suboptimal and is probably an indication that T4-only thyroid medication is not sufficient for you.
The 0.7 to 1.06 range was calculated by taking the difference between 0.7 and 1.9 (which is 1.2) and then calculating 30% of the 1.2 value which is 0.36 and then adding 0.36 to the low end of the range 0.7.
This gives you the bottom 30% of the reference range that I previously mentioned.
You can apply this same calculation to your free T3 level.
If you find that one (or both) of your free T3 and free T4 levels are suboptimal AND you are feeling persistent symptoms of hypothyroidism then you are someone who doesn’t fit this standard mold.
While testing is very important (and it is something you should be doing), it’s not the only way to find out if your medication is working for you.
The second way you can tell is by assessing your clinical symptoms.
If you have hypothyroidism and you are receiving treatment for this condition then you should not expect to have continued symptoms with your treatment, assuming your treatment is appropriate for you.
The studies are clear on the matter. They show that the classical symptoms of hypothyroidism track well with thyroid status and thyroid lab tests (4).
This means that you should NOT be experiencing the following hypothyroid symptoms with your treatment:
- Fatigue
- Weight gain
- Constipation
- Musculoskeletal pain
- Cold intolerance
- Weakness
- Depression
- Brain fog
- Memory loss
The presence of these symptoms indicates that your body is not getting sufficient thyroid hormone.
If you have any of these symptoms then your next step should be to evaluate your TSH, free T3, and free T4 as outlined above.
The more difficult part is not identifying that you need further therapy but instead trying to convince your doctor that you don’t fit into the “standard” mold and require different therapy.
Understanding Thyroid Treatment Beyond T4 Medications (What to do next)
If levothyroxine (or Synthroid) isn’t working for you then what are you supposed to do?
This might seem like a big problem, especially if you are inundated with the conventional medical model, but I’m here to tell you that there are MANY thyroid medications that exist beyond levothyroxine.
In fact, I’ve written extensively about these medications in various blog posts throughout the years.
The key to improving your situation is to use medications that contain a combination of BOTH T4 and T3.
T3 is an FDA-approved thyroid medication, just like levothyroxine, to treat those people with hypothyroidism and those without a thyroid.
And T3 can be safely added to your existing dose of levothyroxine or Synthroid (5) to help brute force your free thyroid hormone up to higher levels.
The only problem?
Despite the fact that this is an FDA-approved medication (6) to treat your condition, your doctor may be hesitant (or just downright resistant) to use it.
If this happens to you, then it may be time to seek out a second opinion or look for a physician who is more willing to work with you.
Dosing T3 in the setting of not having a thyroid can be tricky but it is only slightly more difficult when compared to using T4.
T3 has the same effects (although they are more pronounced) on your TSH levels.
Because of this, you really only need a small amount when compared to T4.
While using T3 be sure to keep an eye on your TSH, free T3, and free T4 levels as we discussed in the previous section.
You should aim to get your free thyroid hormone levels up to higher levels. As they increase you should start to feel your symptoms improve.
Conclusion
What I want you to take away from this article is that not all thyroid patients are alike and that you, as a patient without a thyroid, may need different treatment compared to other people even in your same situation.
If you aren’t feeling well, make sure that you test and look into more than just your TSH. By testing and evaluating your free t3 and free T4 you can find out if you are someone who has trouble with peripheral thyroid conversion.
If you do fit into that category then you will likely need a combination of both T4 and T3 thyroid hormones.
It’s also possible that you may be able to brute force your way into a higher T3 level by using increasingly high doses of T4-only medication such as levothyroxine or Synthroid.
This option, while it may work, is not preferable as it will also cause TSH lowering (or even TSH suppression).
If possible, try to keep your TSH within a normal to low range as opposed to suppressing it unless indicated by something like thyroid cancer.
Now I want to hear from you:
Are you a thyroidectomy patient struggling to feel better with thyroid medication?
Have you had this discussion with your doctor?
Have you tested other thyroid lab tests as described in this article?
If so, did you find that your levels were low?
Leave your questions or comments below! It’s helpful to get as much information as possible to share with other thyroid patients.