If you are new to the world of thyroid problems then something like reverse T3 may be a bit of a conundrum for you.
I know it may seem confusing but we can break it down into very simple terms which will help you understand why this metabolite is so important to your thyroid health (and, therefore, overall health)!
So what is reverse T3?
Reverse T3, sometimes referred to as rT3, is best thought of as an anti-thyroid metabolite.
Meaning that it is something your body creates which is designed to slow down thyroid function.
Why would your body need to slow down thyroid function?
There are actually many (good) reasons why your body might want to do this.
Think about the case of being seriously ill.
Does it make sense for your body to burn excess energy or does it make sense to put more energy into your immune system to help your body fight off infections and recover?
Obviously, it makes sense for your body to put energy into recovery as opposed to building muscle when you are sick.
By altering thyroid conversion as needed, your body can manipulate how much energy it is using (and where that energy is being utilized).
But this assumes that everything is functioning the way it was meant to.
In disordered states, it’s possible for this conversion process to be disrupted which causes serious consequences for thyroid function.
When this happens, you are said to be in a state of high reverse T3 which is exactly what we are going to talk about today.
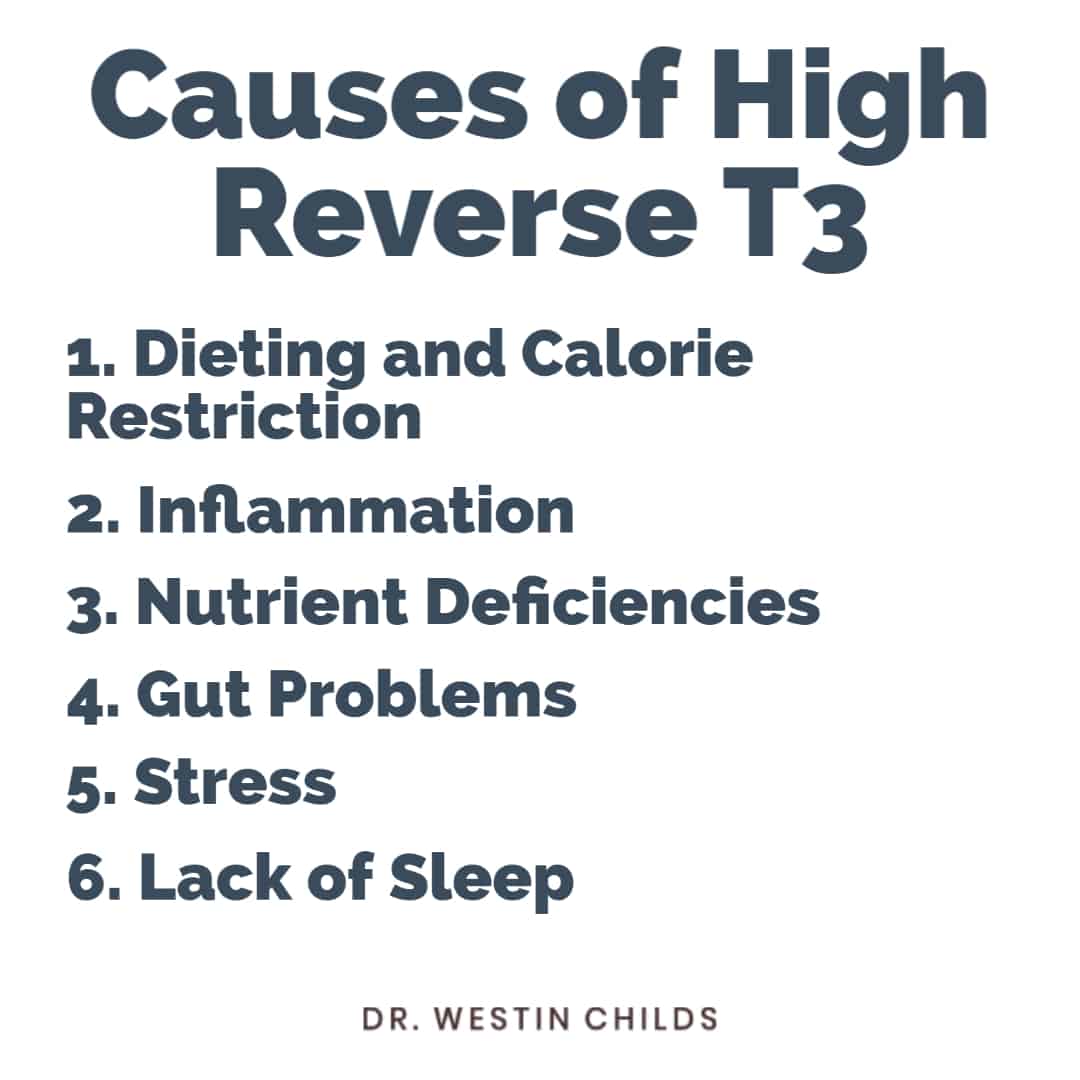
#1. Dieting and Calorie restriction.
The first, and perhaps the most common cause of high reverse T3, stems from calorie restriction and dieting.
This cause such a common cause because so many thyroid patients struggle with weight gain!
Having a sluggish thyroid (known as hypothyroidism) reduces your metabolism which leads to weight gain.
When this happens, most thyroid patients then try to do what everyone does when they want to lose weight which is cut back on how much food they are eating.
Cutting back on calories may cause a temporary benefit to your weight, but it comes at a big cost:
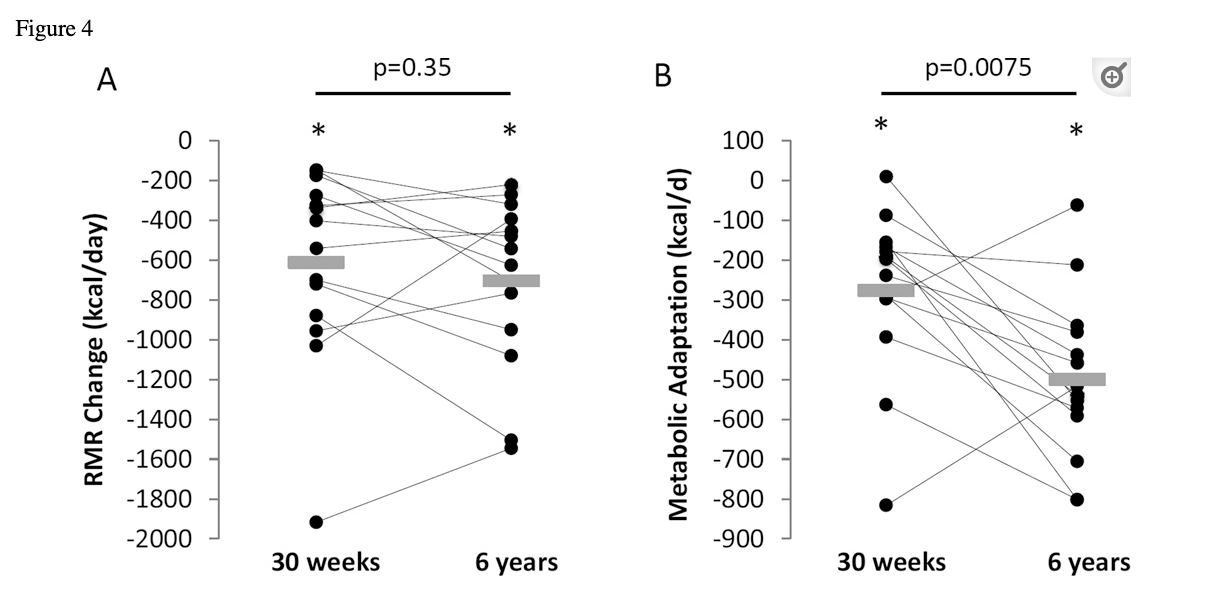
Decreased thyroid function from metabolic adaption (1).
Metabolic adaptation is used to describe the cost incurred by the body from weight loss efforts.
It’s hotly debated right now how big a role metabolic adaptation plays in post-weight loss weight gain, but it seems clear based on my own experience that it is certainly a problem for thyroid patients.
Ignoring the metabolic adaptation controversy for a second, we know that dieting causes several changes in thyroid function including an increase in reverse T3 and a decrease in free T3.
As a thyroid patient, the more you cut your calories the slower your metabolism will become and the more likely you will be to gain weight once you resume eating a normal amount.
And this entire process seems to be primarily mediated through reverse T3 levels.
I’ve had the opportunity to test thyroid patients and thyroid function at many different times including immediately after intensive weight loss programs.
And I’ve seen the massive spikes in reverse T3 that come as a result of this adaptation process.
The argument can be made that the adaptation process is only temporary and that your thyroid and hormones will return to normal after a set period of time.
And while this is true, it doesn’t happen nearly as fast as you might think.
How long it takes for the body and thyroid to recover from weight loss efforts varies, but some studies suggest it can take several years (2).
The good news is that all hope is not lost even if you’ve damaged your thyroid and your metabolism with the use of aggressive weight loss treatments.
The first step to losing weight is restoring thyroid function.
This can be done in a number of ways but one of the easiest ways is with the use of thyroid medication.
Simply getting on the right type and dose of thyroid medication is enough to help many thyroid patients lose weight with minimal effort.
This weight loss will most likely not be complete (complete in the sense that you will get back to normal weight), but it should be enough to help you lose 5-20 pounds without changing your diet.
Once you get to this point you can focus on your other hormones, cleaning up your diet (not restricting calories), exercising, managing stress, taking supplements, and so on.
You can learn more about how I help thyroid patients lose weight by balancing their hormones in my weight loss guide.
The bottom line?
Make sure that you avoid all diets that require you to restrict your calories for a prolonged period of time (3 weeks seems to be the cut-off).
And by restriction, I am talking about anything less than around 1,500 calories or so.
If you eat, say, 1,200 calories per day for 4 weeks straight then there is a good chance that you will see a spike in your reverse T3 levels.
Fasting, when done correctly, does not appear to trigger this same response which makes it an ideal alternative to prolonged calorie restriction for thyroid patients.
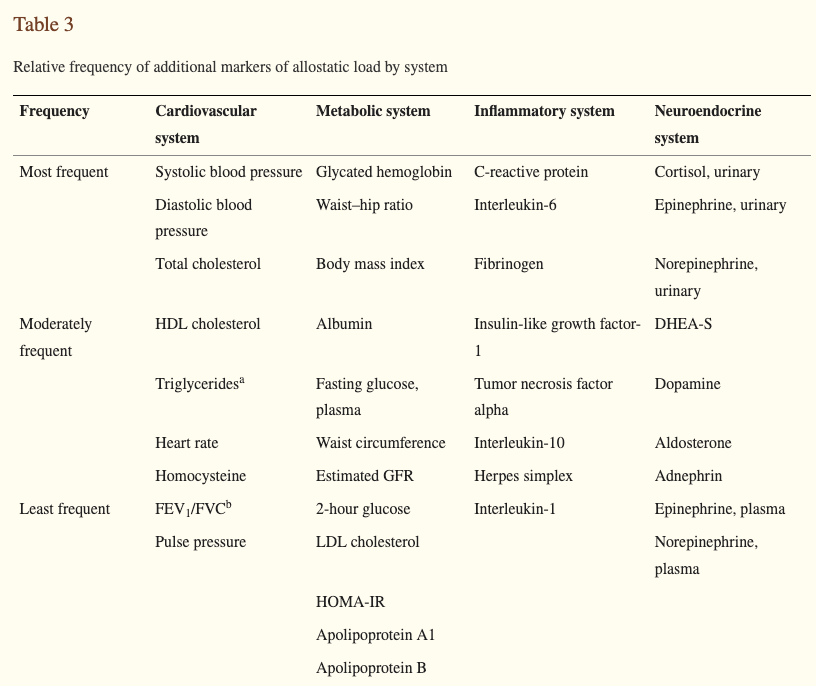
#2. Inflammation.
Next on the list is inflammation.
Inflammation causes a spike in reverse T3 because it forces your body down the T4 to rT3 pathway (3).
Both systemic (meaning all over your body) and cellular (meaning low-grade inflammation which is harder to test for) can cause this problem.
Most people with inflammation know that they have inflammation because of how they are feeling.
People with inflammation tend to feel fatigued, sore, and achy, have joint pain and suffer from headaches, rashes, and so on.
These non-specific symptoms often indicate that inflammation is present but they don’t necessarily tell you where it is coming from.
Symptoms can go a long way to helping you identify if inflammation is present but it’s also a good idea to get lab tests to confirm.
Two easy tests that can help identify inflammation include the ESR and CRP.
These tests don’t pick up all forms of inflammation but they are a great starting point.

In my experience, one very common cause of inflammation in thyroid patients is food intolerance.
Foods high in sugar, processed foods, and foods made with industrial seed oils are often the culprit.
By cleaning up your diet you should be able to see a reduction in inflammation fairly rapidly if that is the primary cause.
Other treatments can also be considered including the use of anti-inflammatory supplements like fish oil, black seed oil, turmeric, alpha lipoic acid, and so on.
Cooling down inflammation is a quick way to help lower reverse T3 levels and improve thyroid function overall.
#3. Nutrient Deficiencies.
You probably intuitively know that nutrients such as vitamins and minerals are important for your body but maybe you don’t understand exactly why.
These nutrients are used as co-factors to help certain enzymes function in your body.
Remember when I talked about converting T4 into T3?
That conversion process is mediated by certain enzymes called deiodinases (4) and specific vitamins play an important role in helping that process function optimally.
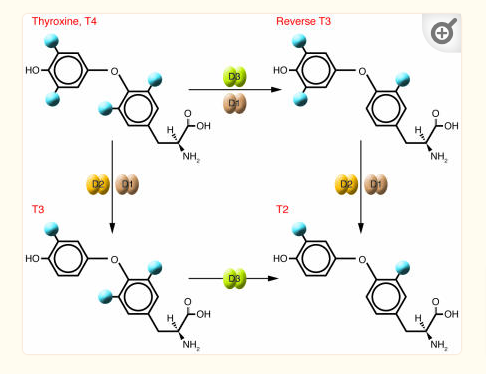
The conversion process will still occur even in the absence of these co-factors, but their absence will slow down its activity considerably.
As deiodinase enzyme activity slows, your body will start to build up reverse T3 levels because it can’t produce T3 efficiently.
The good news is that this provides you with the opportunity to use certain supplements to help augment this process and sort of brute force thyroid conversion in your favor.
The only potentially bad news is that this process really only works if you are deficient in these nutrients, to begin with.
But because most thyroid patients suffer from sub-optimal levels of many nutrients, there’s a good chance that taking them will provide some benefit though that benefit will vary from person to person.
The nutrients and vitamins most important for supporting thyroid conversion include zinc, selenium, vitamin E, and vitamin A.
A deficiency in any of these nutrients may diminish how well your body can convert T4 into T3 and increase T4 to rT3 conversion.
This is actually great news.
Why?
Because taking supplements is something that you have control over.
You can make the decision on your own to purchase and use a supplement without the need to get a prescription from your doctor.
We know from studies that taking these nutrients actually helps as well.
For instance, this study (5) showed that taking zinc improves thyroid function in people who are zinc deficient.
And with factors like soil depletion of nutrients and the impact of thyroid function on stomach acid, these nutrient deficiencies are actually quite common among thyroid patients.
This is one of the reasons why I am so passionate about using thyroid support supplements.
I find they are a great way to naturally improve thyroid function and you can learn so much about them by doing your own research.
If you are ready to start using supplements to improve your thyroid you can find some of my recommended products and doses for each below:
- Zinc – 5-10 mg per day
- Selenium – 50 to 150mcg per day
- Vitamin E – 4 capsules per day
- Vitamin A – 12 drops per day
Zinc and selenium tend to help more with T4 to T3 conversion while vitamin A and vitamin E tend to help more with thyroid cellular activity (and sensitivity).
I’ve written about these vitamins (and many others) and why they are so critical to thyroid function here, so if you want a more in-depth look at how supplements can help your thyroid, check out that article.
#4. Intestinal Dysfunction.
Next, we have intestinal dysfunction.
Don’t let the name confuse you.
Intestinal dysfunction refers to any problem with your gut in general.
Usually, this occurs in the context of an imbalance in healthy and unhealthy bacteria in your gut known as intestinal dysbiosis (6).
But it can also occur secondary to inflammation or damage to your gut lining (such as that seen in increased intestinal permeability or leaky gut (7)).
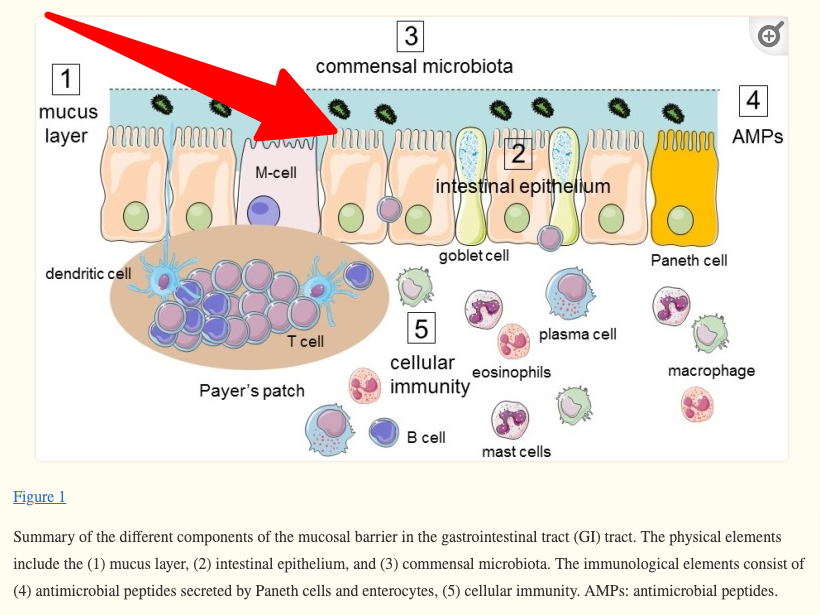
Both conditions result in the same thing:
Increased reverse T3 levels.
How or why does this occur?
Because approximately 20% of all thyroid conversion in your body occurs in your gut (8).
Remember:
Your gut is a huge source of hormones, neurotransmitters, immune activity, and thyroid conversion for the entire body.
Any inflammatory problem (or dysfunction) in this area can compromise any of the previously listed functions including thyroid conversion.
For our discussion, we will focus mostly on thyroid function.
You can imagine that if up to 20% of T4 to T3 conversion occurs in the gut, certain gut problems may limit that percentage and lead to higher reverse T3 levels.
What you may not realize is that pretty much any issue in the gut can cause this problem.
Irritable bowel syndrome, small intestinal bacterial overgrowth, acid reflux, yeast overgrowth (fungal overgrowth), gas, bloating, constipation, diarrhea, and so on.
These are all ‘canaries in the coal mine’ so to speak and their presence may be a reflection of an unhealthy gut.
What’s more, is that these gut problems are much more common among thyroid patients by virtue of how the thyroid influences gut function.
So if you already have thyroid dysfunction (no thyroid, Hashimoto’s, or hypothyroidism) then there is a good chance you are suffering from these gut issues as well.
Treating or addressing these gut issues is paramount if you want to normalize reverse T3 levels.
#5. Stress.
Next up is stress.
And here, I am really talking about stress from any cause.
I probably don’t have to convince you that stress is a bad thing.
We already know that stress can lead to weight gain (9), increase insulin resistance (10), lower testosterone levels (11), cause premature aging (12), etc., etc.
These are obviously things you don’t want to happen in your body.
But we can also add to this list that stress increases your reverse T3 levels and negatively impacts your thyroid (13).
It does this, at least in part, because it impacts cortisol.
Remember:
Cortisol is your stress hormone and it is secreted in times of stress as a compensatory mechanism.
The more stress you are under the higher your cortisol will be and the more it will impact your thyroid function.
For this reason, it is imperative that you do your best to avoid excessive exposure to stress in your day-to-day life.
Some stress is okay and even beneficial, but it can become pathologic when it reaches a certain point (14).
If you can’t eliminate sources of stress then you will need to take steps to improve how resilient your body is to this stress.
You can do this by taking certain supplements such as adrenal adaptogens, using meditation (15) or prayer, eating a healthy diet, supplementing with activated B vitamins, and so on.
If you want to know if stress is impacting your life then make sure you learn more about cortisol testing.
Testing for cortisol is somewhat controversial but it can be helpful in certain situations.
#6. Lack of Sleep.
Last on the list is a lack of sleep!
If you are not sleeping enough then this will drive up your reverse T3 levels (16).
What’s the magic number here?
You should be looking at getting at least 8 hours of quality sleep each night.
Some of you may actually need more than this (I fit into that category) and while some of you may feel ‘fine’ with less that doesn’t mean that your body can actually handle fewer than 8 hours of sleep (17).
So even if you feel ‘fine’ it doesn’t mean that it isn’t negatively affecting you in some way.
If you have an elevated reverse T3 level and you are only sleeping 6 hours per night, for instance, then this might be the sole cause of your high reverse T3 (even if you are otherwise feeling normal).
The number of hours you sleep is important but so is the quality (18).
Make sure you are taking steps to sleep in a cool, quiet, dark environment each night that is free of interruption so that you can sleep soundly each night.
This is very important as well.
Do your best to avoid sleeping aids and sleeping supplements, as well, as these do not necessarily force your body into a restful sleep and in some instances may actually make sleep more difficult long-term.
You can find a list of tips and tricks to naturally improve the quality of your sleep here.
I’ve created this list because I personally struggle with sleeping issues and so it’s always something I’m trying to optimize for myself.
Your Next Steps
The bottom line?
If you are someone who is struggling with thyroid-related issues, then one of the first places you should look is at your reverse T3.
High reverse T3 may explain why some people feel sluggish or hypothyroid despite taking thyroid medication and despite having otherwise ‘normal’ thyroid lab tests.
It’s generally a good idea to get a reverse T3 lab test as part of a complete thyroid lab panel.
Getting this complete panel will help you put all of your labs into context and will help you understand what is happening with T4 to T3 conversion in your body.
If you have a high reverse T3 level your next step is to try and determine the cause.
Use this list above to help you hone down on that issue and then address the problem with the therapies I’ve listed above.
Now I want to hear from you:
Do you have a high reverse T3?
Have you had your reverse T3 level tested before?
If not, are you planning on getting it tested after reading this?
If you do have a high reverse T3 level, what therapies have you tried?
Leave your questions or comments below to keep the conversation going!
Scientific References
#1. pubmed.ncbi.nlm.nih.gov/32386226/
#2. pubmed.ncbi.nlm.nih.gov/27136388/
#3. ncbi.nlm.nih.gov/pmc/articles/PMC3978663/
#4. ncbi.nlm.nih.gov/pmc/articles/PMC1578599/
#5. ncbi.nlm.nih.gov/pubmed/8157857
#6. ncbi.nlm.nih.gov/pmc/articles/PMC4315779/
#7. ncbi.nlm.nih.gov/pmc/articles/PMC7231157/
#8. ncbi.nlm.nih.gov/pubmed/20351569
#9. ncbi.nlm.nih.gov/pmc/articles/PMC2727271/
#10. ncbi.nlm.nih.gov/pmc/articles/PMC9561544/
#11. ncbi.nlm.nih.gov/pmc/articles/PMC6182538/
#12. ncbi.nlm.nih.gov/pmc/articles/PMC7400286/
#13. ncbi.nlm.nih.gov/pmc/articles/PMC3148770/
#14. ncbi.nlm.nih.gov/pmc/articles/PMC6430278/
#15. ncbi.nlm.nih.gov/pmc/articles/PMC4895748/
#16. ncbi.nlm.nih.gov/pmc/articles/PMC8848531/
#17. ncbi.nlm.nih.gov/pmc/articles/PMC4434546/
#18. pubmed.ncbi.nlm.nih.gov/34610163/




What is the pharmaceutical remedy for high reverse T3 when you are already on T4/T3 meds? Change the T4 or T3?
Hello Dr. Westin, Thank you for providing a platform to discuss concerns on Thyroid issues. I am a 70 year old male, who just in early January this year was diagnosed with multiple PE’s in both lungs and DVT in my right leg. In the course of seeing multiple doctors to determine cause and best care practices, It was found in the course of a carotid ultrasound, I had a 1.3 x 1.0 x 1.1 cm thyroid nodule that came back at Ti-Rads 4. I also have family history in both my Mother and brother of Thyroid issues, Goiter and enlarged thyroid. I also have multiple symptoms from both Hypo and HyperThyroidism. I also know from your discussions both can’t be happening simultaneously, so please see below my thyroid panel results. I am scheduled for a FNA biopsy next Tuesday, hoping for some answers to my multiple and simultaneous health issues going on in just the first six months of this year, as I have been fairly healthy my entire life. I am currently taking Metoprolol for SVT, Protonix for Acid Reflux, and have been prescribed as well to take Cholesterol lowering drug as my levels just jumped from 195 to 230 in just the last four months, and have been diagnosed with severe obstructive sleep apnea, all just in these past six months starting with the PE/DVT discovery. Thank you in advance for any commentary you may be able to provide.
Larry
T4 Free .83 ng/dl
Thyroid Peroxidase <0.30
TSH 2.40 uIU/ml
Thyroglobulin Antibody <0.9
T3 Free 3.29 pg/mL
T3 Reverse 25.3 ng/dL
Vitamin 25 Hydroxy 40.00 ng/mL
Dr Childs,
You are the only physician in the content creation world that truly addresses RT3 and actually give actionable tools. Thanks to implementing two of your suggestions – #1 Candida treatment and #2 Adding Curcumin, my up and down RT3 has stabilized to low normal ranges.
I have a request, my latest insulin test revealed low insulin 1.6, normal blood glucose 85. Would you do a post on LOW INSULIN and its impact and treatment?
Dear Dr. Childs,
I have been following your blog with great interest for quite some time and want to thank you for all the interesting and useful information and guidelines you post here!
Unfortunately, there don’t seem to be many doctors like you in Europe where I live. Some do prescribe NDT, but not T3, and I don’t know of a single one willing to test and treat rT3. Fortunately, there are few labs where you can order these tests yourself, which is why I find your blog so helpful.
One thing I have noticed is that you rarely (if ever) refer to progesterone and estrogen treatment. I know that you have prescribed testosterone to female patients, but you don’t mention E or P. I have been to so called functional or alternative practitioners who all told me women over 40 need to be on E and P. However, from articles I’ve read, it seems even menopausal women can produce enough estrogen from other sources than the ovaries, especially overweight women since E is produced by fat tissue as well. So, lately, I have been wondering if taking estrogen routinely once you’re 40+is really a good idea…especially if you have been diagnosed with insulin resistance and struggle to lose weight…?
Is there a reason you don’t routinely prescribe estrogen and progesterone to your female patients?
Hi Anna,
I prescribe both estrogen (bi-est typically) and progesterone to women all the time 🙂 I have several articles on the topic, in fact. I do not believe, however, that all women over 40 should be on both as that just wouldn’t make sense and would cause more harm than good for many women.
Hi Anna,
I feel the same way – I am from Germany and I am also very interested in the information here 🙂 rT3 is particularly important to me and I am very disappointed that there is so little scientific data on it. I am therefore very pleased about practical experience. I can therefore tell you that thanks to E and especially Cortison, I was able to adjust my thyroid (with alternating strong rt3 formation) significantly better – yes, I really need to take hydrocortison (adrenal rebuilder alone e.g. was not enought) and there are also data available that not even too much but also to low Cortisol stimulates rT3 formation. Although E is often made responsible for weight gain, one should Keep in mind that E is the main anabolic hormone in women and is thus important for building muscle, creating Energy, good Ventilation/breathing. Not without a reason femal athletes need more Estrogen or one should better say use up more E (and less progesterone) to achiev Performance and thus have performance Problems which are due to excesiv consuption of E. Of Course it might not that simple and especially Hormons are very complex due to their interactions (and You don’t learn this complexity during your medical studies, but unfortunately rather best when you are affected) …. I would just like to note this briefly and hope that is fine at this Point – if not, Sorry for my comment
Hi Nicole,
Thanks for sharing! I agree that the connection is probably more complex than mentioned but you are heading in the right direction.
I have Hashimotos and have had it for about 20 years. Struggling with my Thyroid levels. They are very low. I don’t have enough T4 to even convert to T3 I do not know why I am not making T4. I also do not have glutathione. My other hormones estrogen, progesterone and testosterone are all low. My natural pathic Dr. currently has me taking Nature Thyroid at 1.5 gr. I take 2 a day and progesterone pills and creams for the other two; which i am not comfortable with because of the problems they can cause. I am tired, fatigued, and gaining weight.
Hi Michelle,
You could be in end-stage Hashimoto’s which would explain your low T4 levels. You can read more here: https://www.restartmed.com/end-state-hashimotos/
Dr Childs, my TSH is .020, T4 is .8, reverse T3 is 18.9 T3total 136. I am on 100mc of Armour. Feel pretty good with some symptoms, my doctor wants to lower meds due to suppressed TSH. Already have problems controlling weight. Use to be on Cytomel and felt fantastic, but current doctor changed me to Synthroid and felt terrible on it. Finally got her to try Armour. Also, my blood test never did show thyroid problem, but uptake test proved was a problem. What needs to be done?
I was on Synthroid/cytomel/hydrocortisone for 14 years. Every 6 months or so, I would start to feel sluggish, and start to gain weight, and would increase my Synthroid. After I retired from teaching, which had been very stressful as a job, I began to have strange reactions to foods and supplements that never gave me problems in the past. I knew that I was in de-stressing mode, and thought that could be one of the reasons. A doctor I see periodically, suggested WP. My life changed so dramatically… I felt like before I ever had Hashimotos. I didn’t even need to try, I lost 30 lbs in a year…slow but steady. Energy levels were back, sciatica was resolved, acid reflux was resolved, no fibromyalgia and other small things, all resolved. Then, 18 months later, the company halted production. I had to switch to NatureThyroid…. and within 10 days I was huffing and puffing, and experiencing serious breathing issues. Went on pumps, with little help, or they gave me what I now know were adrenal reactions-awful! After 3 months, I went one day without meds, and experienced none of the breathing issues! Despite me telling the doctor what was happening to me after the switch in meds he refused to believe there was a connection. Anyway, I went back to Synthroid, had no breathing issues, but gained weight immediately…7 lbs in a week! 2 months later my doctor told me he again had WP… I was so happy! But to my great disappointment, just 2 grains gave me the same breathing issues within 24 hours. I had originally tritated to 4.5 grains, and. Ow I could not even handle 2 grains! The more I took the worse the breathing issues. Strangely, all the other issues went away again, but the breathing issues were very scary as it affected my heart as well. I stayed on 2 grains for another 6 months, and stopped 2 months ago.
I am on Synthroid .137/T3 25mg/ – very careful about food (trying to follow a paleo diet, except for dairy) – just in the last month I gave up gluten completely. Yet I gained 5 lbs a month since I’m back on Synthroid… what other meds would you suggest? Obviously I do better on natural thryoid , but is there another make you would suggest?
I hope this helps some of you.. Find a doctor who will test Free T3/Free T4 and prescribe Armour or NP Thyroid – something natural. The TSH test does not work for all patients, and Synthroid does not work for all patients!!! That’s just what is being forced on us as patients, and it’s keeping millions of us sick. Period. I’ve had Hashimoto’s for 20 years. The TSH test and Synthroid/Cytomel worked for 1o years, then stopped for no apparent reason. I eat gluten & dairy free, exercise 5 days a week, and am diligent. And still had Vanderbilt doctors trying to reduce my dosages to a point where I almost couldn’t get out of bed. NO. Put your foot down people!! Enough is enough. I kept searching until I found a good doctor who listened and knew his stuff.
Today if you test me, I have ZERO TSH, but my Free T3 is exactly in range. Free T4 and T3 measure how much thyroid hormone is actually available at the cellular level to exert its metabolic effects. Surprisingly, cells need energy to run on. Not TSH. Request the Free T3/Free T4 test, keep your results, track your own progress, and ask to be prescribed based on those results – if the TSH test doesn’t seem to be a good indicator for you. Best of luck everyone!
Hi Kswen,
I would be cautious of prolonged TSH suppression if you are post-menopausal. It’s always ideal to optimize your thyroid without suppressing the TSH if possible. You can learn more here: https://www.restartmed.com/suppressed-tsh/
I am trying to figure out why I have *both* a high Free T3 (5.2) and a high rT3. (30.7)
T3 is good and Free T4 is good. TSH is low.
Could it simply have been timing of the labs? Too soon after taking cytomel?
I’m in the process of lowering my T4 (synthroid) and raising my T3 (cytomel).
I had been stable for years, with good numbers but gaining weight with high rT3. It’s so true, dieting raises my rT3, then I get stuck and gain more weight.
Hi Cyndy,
Yes, it could be something as simple as timing. If you test your free T3 sooner than 24 hours after your last dose of T3 your free T3 will be high.
Thanks! I will recheck soon.
So grateful to you for being a true physician… teacher. You are helping so many patients that are truly in need of information, and empowering them, so they can take the steps to start to feel better. Thank you!!!
Hi Angela,
Glad you find it helpful! And I’m happy to help.
Two years ago I ended up with C-diff due to several rounds of antibiotics for an infection I didn’t really have (long story-I’m very angry about it). Due to the illness and the treatment, Flagyl, I lost weight. I weighed 197lbs to start, and dropped down to 158lbs in a matter of a couple months.
I had been taking 50 mcg of L-thyroxine for many years before that with no problems.
After the hell I went through losing that weight, I was going to do my best to keep it off. About six months after everything, I started to eat normal again. (I had many food restrictions due to my gut issues and my post infectious IBS). I had gained 10 lbs back. I figured that would be normal since I was eating more than 1,000 calories per day.
From that point forward though, my thyroid was testing all over the place, but it was in “normal” range according to my doctor so I kept taking my pill as usual.
Fast forward, I’ve been slowly and continuously gaining weight. No matter that I eat clean, take my Synthroid, vitamins and supplements, and being more active than I have in years. I now weight 210 lbs. It’s the heaviest I’ve ever been – even when I was pregnant many years ago.
I spoke to my ENT about the fatigue that has been plaguing me for years that my primary doc isn’t concerned with, and she ordered 13 tubes of blood to be tested. One was my Free T3. My regular doc never tested it because my thyroid was always in the “normal” range.
It came back slightly over the normal range, she told me to show my doctor. But we sold our house and moved and I had to wait to get a new doctor then it took me 3 months to get in to see the new doctor due to insurance issues (hubby is retired military), and she retested me. This time taking 18 tubes of blood. According to the blood work other than my thyroid testing high-normal everything was excellent, but she did NOT test my Free T3 again even knowing it was high previously!
Recent blood work show’s I’m super healthy (even my cholesterol which surprised my new nutritionist – that my new doctor sent me to, he said it shows I’m eating well and exercising, but I knew that already). His conclusion is that I’m not eating enough, my thyroid results weren’t back at the time – he didn’t get to see the numbers. So, now he’s got me eating so much food I want to barf.
At my follow up, one month after my blood was taken, my doc told me last week we’re going to switch up my Synthroid to jump start my thyroid. So, now I’m taking 50 mcg 3x per week, and 75 mcg’s 4x per week. This makes me nervous, why aren’t we doing anything about my Free T3? No response from her concerning that matter.
My main complaints going it to see her, was; 1) fatigue – I could sleep anywhere from 4-12 hours and still feel the same regardless. I used to be fine on 7 hours. Not anymore. 2) weight gain – I started to panic when I hit 200 lbs and saw it wasn’t stopping any time soon. 3) energy/weakness – my body doesn’t want to do anything. I just feel weak.
Her first response to me was; “There are three weight loss drugs you can try, however I prefer the lap band surgery.”
Say what??? Shouldn’t her concern have been to figure out why I was gaining weight despite my efforts, and that the weight gain wasn’t stopping? I wanted to run out of there, but after waiting for three months to get in to see her, I felt trapped. She wasn’t even concerned with my thyroid, until it came back high normal again. She’s trying to get me in the middle of the normal range to see how I feel then. So, I’m to get my blood work redone at six weeks from starting the new Synthroid regime. I’m one week in, the side effects weren’t kind at first, but I can tell I’m adjusting.
I know this isn’t going to be an overnight fix, and I’m willing to do what I need to do to feel like me again, it’s been ages. I miss me! What do you recommend I do?
Hi Natalie,
You have to understand that doctors pretty much solely believe that weight gain is due to eating too much and exercising too little. They will pay lip service to the idea that weight gain can be caused by hormones but they don’t understand it nor do they actually believe it. I know this because your doctor gave you the option of 3 weight loss medications (which suppress appetite) or lap band which is the surgical intervention for weight gain. You should start with a complete hormone panel including your thyroid, leptin, insulin, cortisol, and sex hormones. That will help you figure out what you need for treatment.
Thank you! I’m going to request a new doctor because this one has lost her mind. And I’ll request the suggested hormone panel!
No problem!
Hi,
I believe my issue is with my Conversion. So I was hoping to try you T3 conversion Booster….
Reverse T3- 14.1 (9.2-24.1 range)
T3 (free) 2.5 (2.0-4.4)
TPO 14 (0-34)
Sex Horm Binding Glob 147.3 (24.6-122)High
Magnesium 1.8 (1.6-2.3)
T4 .85 (.82-1.77)
TSH 1.7 (.45-4.5)
I also have a SIBO, Raynauds diagnosis and EBV and Endo.
My health took a major dip about a year ago and I’ve been trying to come back ever since. So my albumin levels are finally ok. I’ve been trying to heal the SIBO as I know the hormone/thyroid go through the gut and if I can get that moving I have a much better chance to get the thyroid/adrenals working better.
I had a complete adrenal crash a few months back but my Cortisol tests (I’ve done 3) are a bit off, but not enough to concern the drs of course:).
Currently taking a host of supplements, but most significantly Ashwaganda and Liothyronine(5 Mcg), natural Progesterone cream. IDK if the Thyroid med is helping honestly.
Im currently 110lbs 5’6”, so (while I’ve manage to put a few lbs back on since the major dip), I’m still skinnier than I normally am, but I seem to be gaining, even though I still don’t eat a normal amount (which is hard to do with sibo). Altho I have a feeling the thyroid issue will eventually make weight gain a prob.
I’ve lost about 1/2 my hair (either the health, stress or thyroid) and have extreme fatigue.
I KNOW you’re not taking patients so I’m really just looking for advice on supplements. I honestly feel like with the SIBO, I’m a bit nervous to add any additional supplements. BUT IF you had time to glance over anything I’ve written, I’d really appreciate it!
I’ve seen every dr in my area (but since most of my labs are “normal” so am I), I’m currently seeing a NP but have only gained traction at my own behest.
Thank you
I was on synthroid for 30 years. For the last several years- 75 mg. TSH above 5 so doc wanted to increase to 88. Had my own blood work done and high reverse t3, low T3,mid T4 Switched Drs and trying Armour 60mg. Felt pretty good, brain fog gone, more energy, sleeping better but around 4 th week getting chest pain and heart palps. Blood work on 60 Rt3 droped and near bottom range, TSH 3.6, Ft3 up a bit, FT4 on the bottom of range.I am now on 30 Armour which is more bearable but still not great. I can feel my blood pumping under my rib, chest discomfort. Blood work soon. Did I start too high? Have you heard anything about Armour being reformulated or pig source changed. Seems lots of people are struggling that didn’t struggle before. Doc says give it a week and see. I am about ready to give up even tho the rest of me feels pretty good!
Thank you for the reverse 3 info. I asked my GP doctor to include a blood draw to test it. So far she’s not willing. She is usually fairly forward thinking. Studied some course on nutrition at Scripts, for what that’s worth. Any suggestion for the 1 thing I can say to her to spark her interest?
Hi Lois,
Not really, it’s better to just find a doctor who is forward thinking. Even if you convince her to order the test she still won’t know what to do with the results.
Hi,
I have high TPO and high rT3. My other thyroid number all fall in the very low end of the normal range. My doctor allowed me to experiment with trying both NDT and Synthetic. All had side effects for me including heart palpitations except for Tirosint. However, once on Tirosint my T4 increase and my rT3 increased as well. Didn’t help to solve the issue. I’m not sure where to look next. I have inflammation and gut issues, but conventional wisdom ins’t helping me to get to the root cause of the inflammation. Any suggestions on a process to figure out the culprits?
Thanks,
Megan
My reverse T3 was 24, after five weeks on 60 armor my reverse T3 was 11. However after three weeks on armour I started with palpitations. Week seven I couldn’t take it anymore and the doctor dropped me down to 45. I am down to 30 now and do not feel good at all. I felt good the first two weeks, brain fog lifted more energy better sleep. I have heard that NP thyroid is no longer any good and people are having a lot of problems on it. It smells bad and their labs are no longer optimal.Apparently the company has changed their pigs source. Have you heard if there’s a problem with Armour? Why am I not feeling good?
Hi Shelley,
It sounds like your issue is just a dosing issue. In regards to NP, Nah, it still works fine for many people. Many people try to blame their medication but I almost always find that some other big problem is left unattended which is accounting for their symptoms. Most people also forget that dosing thyroid medication is not an exact science and that your dose will change many times throughout your life.
I so appreciate all you are doing with your blog. For a detail oriented person like myself I have this need to understand the details. You have provided, thank you. Soon after reading all your RT3 blogs I had an appointment with my doctor. She does not resist my request but she is not very knowledgeable. I requested a RT3 test, she had never heard of it. She searched on her computer and found the code to order it. Guess what…it just did not happen. Either the lab did not know what it was or something. It is frustrating out here in the US, trying to navigated the medical systems. I have lost faith in what I once believed in. To few medical providers to go around and too expensive to keep trying new ones. I was confused by a few things in your blog. It implies that a person can elevate their RT3 fairly quickly with dieting and then it can take a year to get it back down. Is this long amount of time to get it back down the norm? Once elevate, am I correct in the thinking that T3 medication would still be absorbed and help with balancing? Once elevated would taking selenium help get the RT3 levels back to normal without T3?
I have high rT3 and TSH, with normal ranges of T3 and T4 and without antibodies (I have a controled autoinmune disease, but not on the thyroid). I have no hypothyroid symptoms except fatigue. I take care of my nutrition, exercise and stress management. I supplement with active B vitamins, Omega 3 and probiotics. I take no other medications. But my T3 and TSH go higher and higher. I read many blogs and books an I feel that my case isn’t like the majority. This is the first text I read about how to manage a high rT3, but I’m a little bit lost… If you can help me, I’ll appreciate so much. Thank you in advance!
Hi Alex,
If you have any questions feel free to post them below and I can try to answer them!
Thank you so much for your great blog..I was at my obs office today, and I discussed with him the more I diet the more I gain..I did the endoscopic sleeve..and didn’t lose a lb. I had periods where I was bulimic from frustration. My doctor suggested that I read up about your program.. what would you suggest I go from here? Can your program be of help. My thyroid levels are all in good range. Thanks In advance!
Hi Nancy,
If you are talking about the weight loss program then you don’t have to have thyroid problems in order for it to work. But you should be aware that weight loss will be very slow given your history of bulimia. Bulimia and anorexia cause severe metabolic damage which can take years to recover from so you need to understand that your weight loss will be very slow. But the therapies found in that guide would be ideal given your situation.
I need some help with figuring out my labs so I can ask my doctor to help me properly address my situation, and whether or not the high reverse T3 is causing recurring miscarriages. Labs were done 22 hours after the last dose of medicine was taken.
Current medicine is 325mg WP Thyroid (65 mg, 3 in AM and 2 in PM)
RT3 – 25 (8-25)
TSH 0.1
Free T3 – 4.7 (2.3-4.2)
Free T4 – 1.4 (0.1-1.8)
Thyroglobulin antibodies – <1
Thyroid peroxidase antibodies – 3
Platelet – 283 (140-1400)
Vitamin D – 33 (30-100)
Red Blood Cell – 5.19 (3.80-5.10)
Ferritin 15 (16-154)
Progesterone 5.9 ( approx 5 weeks pregnant, jumped to 15.5 within 5 days, and dropped to 6.9 one week from the first lab, resulting in miscarriage)
I was on 50 mcg of Tirsoint my doctor added t3 I began To feel pretty good my brain was working good then she went up to 75 mcg + t3 mcg I felt great had the most energy and no anxiety and depression. Had to get a Cortisone shot in back everything went bad thyroid went hyper Not sure if shot did this or not had to come back down to 50 mcg again but no t3 I am depressed again and anxiety. I know I have digestive issues IBS have been on special diet. They do not know what causes it or how to cure it. I am assuming my Rt3 was high so that is why I went hyper. So I am assuming I have a conversion problem. Since there is no cure for IBS is there anything I can do to to help the conversion I am only on t4 med now. If I added t3 again would it go hyper again. I feel hopeless because I am going to have to go on an antidepressent which is not going solve the problem. Help
I’m not exactly sure what’s going on. I have Graves Disease/Hyperthyroidism and was treated with RAI in 2011. My TSH and Free T4 are normal but my T3 are elevated. I have put in 30lbs in 2 years. I’ve looked over a lot of my test results and I’ve never had my Reverse T3 tested. I’m starting to think that maybe my Reverse T3 is the culprit of my weight gain? I can find too much info on individuals dealing with Graves Disease and weight gain. Any advice would be greatly appreciated!
Thanks!
Hi Brittney,
You won’t find any information on what you are looking for because you are looking in the wrong place 🙂 Once your thyroid has been ablated with RAI you are no longer hyperthyroid, you are now hypothyroid. So if you are searching for how to treat weight gain with hyperthyroidism you won’t find what you are looking for. Anything related to weight gain and HYPOTHYROIDISM is what you need to be looking at and I have tons of information on that: https://www.restartmed.com/thyroid-weight-gain/
Dr. Child’s,
I have had excessive hair shedding for three years(after removal of my right thyroid) Nothing has helped with this problem. My endocrinologist prescribed Tirosint (75) but always have high levels of RT3 (26) so assume I am not converting T4 to T3. My doctor does not believe in T3 meds so I went to a functional doctor who took me off of Tirosint and prescribed time release T3 only(5 mcg twice daily). My hair shedding has not improved, in fact it is worse. I just do not know what to do anymore. I have been fighting this battle for three years. Any suggestions would be greatly appreciated. Thank you
Hi Sher,
T3 (especially Cytomel) can exacerbate hair loss but it is usually only temporary.
Hi Dr. Childs,
Last year July 2020 I was diagnosed first with EBV and 3 weeks later Hashimoto’s. I had the flu that February and although I felt better I started to develop exercise intolerance (blamed it on the lockdown stress) and would wake up a lot with flu like feelings in my leg, which would subside after an hours.
Anyway, no issues before that flu.
In October 2020 I had my reverse T3 checked and it was sky high, 63 ….yikes. Also retested EBV and the titers were of the charts high. I was at my worst from EBV then, completely bedridden. Husband later said he was always in start mode to pick me up and take me to the ER.
Worked on getting EBV back dormant (haven’t retested that one yet) and am finally feeling better. Still have ways to go, but retested reverse T3 and is now 18, which is a huge drop compared to 4 months earlier. T4 is 1.4 and T3 is 2.8 (too low).
My question, should I make sure this EBV is dormant again before looking in to thyroid medication or start thyroid medication now?
I looked at your supplements but it contains black cohosh which I can’t take.
Thank you for your time.
Hi Maggie,
There’s no reason to wait to start thyroid medication/supplements with EBV. They can be used regardless of your EBV status.
Hi Dr Child’s
I actually feel as if the thyroid meds themselves cause acid reflux . Increasing histamine lowering dao and causing leaky gut or just making the condition worse. This then increase reverse t3 from the inflammation involved . Viscous cycle. I’ve tried them all even tirosint but gelatin is high histamine as well. Any thoughts on this ? Also having issues at menopause ….. I’ve read that estrogen. Dominance can cause high reverse t3 . It’s never ending. Then I understand you actually need estrogen and progesterone for optimal for thyroid function. Oh and estrogen depletes dao and progesterone increases it …. so how r we as women suppose to break down histamine in the gut that’s contributing to ibs ect…
thank u
Lori
Hi Lori,
Some thyroid medications can be hard on the stomach. The good news is that simply switching to another brand of thyroid medication will solve the problem 🙂
Thank you so much for this information. I’ve had hypothyroidism for years. I found a doctor that helps me manage it better, and since I was feeling better tried to start a diet and exercise program to lose weight. 3 weeks into it, I crashed hard and had my thyroid labs checked. My reverse T3 is high. Same thing happened last year. After reading your article I now understand why this isn’t working for me. Thank you!!
Hi Audrey,
Happy to help!
Hello! In need of help. I just got my labs back and I don’t think I’m getting the right help. I had RAI in 2017 so my labs are a bit funky. My primary dr is keeping me at 125mcg (Tirosint) and 10 mcg (Liothyronine) even though my TSH is at .02. I have no “hyper” symptoms and my T4 and T3 are in the normal range. Also just had my reverse T3 tested since I haven’t been feeling well and that’s at 26 – abnormal and high. My primary dr didn’t comment on it but I know this is why I cannot lose weight and I’m exhausted. Especially after I run. My Naturopathic Dr wants me to decrease my T4 to 112mcg since she said it’s the T4 that is the issue. I read your list of issues that cause high RT3 and I’ve been very stressed but also deep into peri-menopause and have not had a period since 1/28/22 so I’m wondering if this is related and what to do! Also, I was advised to stop the zinc and selenium so this isn’t making sense. Hoping you see this as the article is old. Thank you!
Hi Erika,
I would recommend checking out this article which explains more about your situation: https://www.restartmed.com/weight-loss-after-thyroid-removal/
That article is about thyroid removal but the information still applies to you since you are post RAI.
Hi there,
First of all, thank you for this article! I love your holistic approach and thyroid knowledge and appreciate this reliable source.
I began taking thyroid medication (Amour) a while back due to a mold toxicity issue that lead to CIRS and threw my hormones out of whack.
As of the past six months I’ve had trouble with rising RT3, and my dr has slowly been scaling back my dosage, which seems to be working well.
My body seems to be healing as I come out of this illness, and I’m wondering if it will be eventually possible to scale off the thyroid meds, very slowly, but altogether.
My question is basically this: Do you ever see people with rising RT3 simply because they are on too high of a dose of thyroid meds?
And have you ever seen anyone successful scale off of their thyroid meds completely? (Not with hashimotos obviously, but just a sluggish thyroid due to other health issues.)
I would love your thoughts on this!
Hi Audry,
Yes, absolutely. The body will attempt to block excess thyroid hormone by increasing reverse T3 (if it can). And, yes, you can learn more about getting off of thyroid medication here: https://www.restartmed.com/how-to-get-off-of-thyroid-medication/
Hello,
My blood work shows my rt3 is high at 24. My doctor has suggested lowering my t3 dosage. I currently take compounded t4 at 57 mcg and 13 mcg twice daily. It’ll be lowered to 9 mcg and t4 stays the same. Wanted to check if this was the best option.
Tsh 0.01
+ T3 REVERSE, LC/..
(ng/dL)
24
Jun 2022
Range: 8-25
† T3, FREE
(pg/mL)
4.1
Jun 2022
Range: 2.3-4.2
+ T4, FREE
(ng/dL)
1.3
Jun 2022 Range: 0.8-1.8
† THYROGLOBULIN
(IU/mL)
>1000
Jun 2022
Range: < OR = 1
+ THYROID PEROXI..
(IU/mL)
111
Jun 2022
Range: <9
Thank you!
Hi Char,
Unfortunately, I’m not able to provide medical advice regarding what you should do with your thyroid medication. I can point you to this article, though, which may be helpful: https://www.restartmed.com/normal-thyroid-levels/
just wanted to ask you a question just for my understanding how often should you get you thyroid levels cheeked
Hi Kelsey,
It depends! If you are trying to figure out your dose then you might want to get it checked every 2-3 months. If you are just keeping an eye on your levels then 2-4 times per year usually works.
Hi Dr Child’s
I’m in Australia and it’s very hard to find a dr who will test reverse T3.
I begged my dr to test it for months as my thyroid felt inflamed. He finally did but in the meantime I suddenly started reacting to all foods that I eat My RT3 was 1212! And it should be below 170. I finally found an integrative dr to help but it looks like now I have suspected MCAS to deal with, huge weight loss and react to any meds they prescribe too. I’m taking T3 to reduce my RT3 but at a loss what to do with the rest. I’m surviving on 2 foods and react to all proteins as well so no meat for 2 months just small amounts of rice and potato.
Will my RT3 correct itself even eating such small amounts of food?
I also have high testosterone and DHEA?? A kinesiologist says it’s the CRH hormone causing it and high cortisol levels. It’s all so hard to navigate when drs just don’t have a clue Do you have any help or advice on my situation please?
I’m so lost and feel like I’m wasting away to nothing. I’m honestly desperate now.
Hello Westin,
What a fantastic video. I do have a slightly higher level of RT3. T4, T3 and TSH are all in optimal range.
I could have all six of your causes for high RT3. Where do I start.
I’m working with a functional med doc in holland but she does not have in-depth knowledge on this.
And can a very high level of THYROGLOBULIN Ab indicate an autoimmune conditions when all other markers other than he RT3 are normal?
I look forward to hearing from you
Daphne
Hi Daphne,
Yes, it could be an early indication of Hashimoto’s or some other condition. You can learn more here: https://www.restartmed.com/thyroglobulin-antibody/
I came across your articles on RT3 maybe being a cause of weight gain while on desiccated NP thyroid. I have a functional medicine doc but haven’t discussed this with her yet. recently my sleep has been terrible, the anxiety is very high, so high I can physically feel it in the middle of my chest and have, in the past 6 weeks, have ballooned in my upper belly (like I did in the beginning of menopause) I thought it was due to my hormone pellets running out but having them inserted 3 weeks ago hasn’t brought relief. I quite taking my thyroid to see if that helped and my sleep has already improved. my last thyroid test results were great but did not include a reverse T3. I also take biote iodine + selinium. I am thinking this may be my problem! I could not find anything that would explain why I would gain weight while on thyroid medication.
Hi Teressa,
It could be and it’s pretty easy to test for.
Hello I’m Carla , and on my last lab test my reverse t3 was on the high level , all my other level which is t4 , t3 , and other hormones were fine , I was take 150 mcg Synthroid Dr lower to 137. I’m still having hypo symptoms but I can sleep better ,I’ve gain like 40lbs , muscle weakness, inflammation I really need your advice Dr Child it’s been like 6 years I’m struggling up and down with this issue please help.
My RT3 several weeks ago was 82! I assumed it had to be a lab error. I went down in my t4 meds and up in my t3 meds. Just tested again and I’m still at 28 for RT3. Am I dying???
I take t3 which causes less t4 that results in less reverse t3. I was in very bad shape 4 years ago with 3.0 t3 and 30 reverse t3. I am now 3.2 t3 and 16 reverse t3. I could not remain upright more tha 2 hours, now very active. Hair loss scalp, outer eye brows, underarms. Symmetrical sores on ears. Lesions on wrists, infected toe nails, loss of heel pad tissue per podiatrist. All symptoms improved rapidly with taking t3.
What could cause rt3 to jump from 11.5 to 21 with just a small 15mg increase of np thyroid? Both my ft4 and ft3 were in bottom of range. Doctor thought a small increase might be beneficial. Obviously not. Tsh below range as well. What might need addressed?
Hi Lou,
Every dose of NDT contains more than 3x the dose of T4 than T3 so even small doses of NDT can increase reverse T3. Just be careful not to practice reference range endocrinology, that is to say, a primary focus on lab test values over other more important factors like your symptoms.
I am experiencing breast tenderness and soreness. I even stopped my bioidentical estrogen and testosterone to make sure that wasnt the cause. my rt3 was a 28 on last lab work. All other hormone levels were within normal range. The PA could not find how to order Free t3. there was no code for it.
Anyway, other symptoms include significant muscle tightness and achiness, brian fog and significant sore breast. Can an elevated a Rt3 cause these symptoms?.
Thank you!
Tracy
Hi Tracy,
An elevated reverse T3 is just a warning that there is a problem, it doesn’t necessarily cause problems on its own. You’d want to find what is causing your reverse T3 to be elevated as that is probably contributing to your current set of symptoms.