It may surprise you to know that around 1% of the population suffers from this condition (1).
And it’s especially important if you consider that a small percentage of patients with this disease may go on to develop thyroid storm.
But what exactly is thyrotoxicosis? Is it a problem if you have it? Is it different from hyperthyroidism?
In this article I’m going to walk you through this condition, we are going to discuss what it is, how it affects your body, the consequences of this condition, how to treat it, and more.
What is Thyrotoxicosis?
When it comes to your thyroid there are many different problems that can arise.
The most common thyroid condition is known as hypothyroidism which is a condition of too little thyroid hormone.
Another common condition (although not quite as common as hypothyroidism) is hyperthyroidism which is a condition of too much thyroid hormone.
Thyroid hormone plays a very important role in regulating many processes in your body.
But, like other hormones, the goal is to have the right balance of thyroid hormones at any given time.
If this balance shifts to too much or to too little then symptoms may arise and problems may start to occur.
Thyrotoxicosis is the name we give to a series of symptoms that arise from excessive thyroid hormone stimulation (2) on your cells and in your body.
Normal amounts of thyroid hormone help to create energy, manage your metabolism, regulate other hormones, promote hair growth, promote regular bowel movements, and help your heart beat regularly.
If your cells start to become overstimulated by thyroid hormone (from various conditions which we will explore below) then you are said to be in a state of thyrotoxicosis.
And this condition, if not treated, can directly lead to damage or death of your cells (which is why it must be taken seriously).
And this state is very harmful to the body!
In fact, untreated thyrotoxicosis can lead to serious consequences such as bone loss and heart problems if not treated relatively quickly.
In addition, it can also lead to a more serious and potentially life-threatening condition known as a thyroid storm (3).
The Difference Between Thyrotoxicosis and Hyperthyroidism
The terms thyrotoxicosis and hyperthyroidism are often used interchangeably, but it’s important to realize that they are not the same condition.
Distinguishing between these two conditions is actually very important because it may impact your treatment and your prognosis going forward.
So, how are they different?
Hyperthyroidism is the name of several different diseases and conditions which ultimately lead to excessive amounts of circulating thyroid hormone in the body.
Thyrotoxicosis, on the other hand, is the name given to the symptoms that arise from the excess thyroid hormone.
This state often is associated with very characteristic symptoms which we will go over below.
But, just because you have hyperthyroidism doesn’t mean that you are in a state of thyrotoxicosis (4).
In fact, the entire goal of treating hyperthyroidism is to help reduce thyroid hormone, reduce the impact of thyroid hormone on your cells, and normalize thyroid levels.
For instance:
Taking hyperthyroid medications such as methimazole helps to reduce thyroid hormone production and conversion thus reducing the impact of thyroid hormone on your cells.

Undergoing a thyroidectomy or RAI reduces the total amount of thyroid hormone produced by destroying or removing the gland that produces thyroid hormone.
All of the treatments for hyperthyroidism focus on this goal!
If you have hyperthyroidism and you are still in a state of thyrotoxicosis then that is an indication that your treatment is insufficient or needs to be adjusted.
Because, in a perfect world, all therapies designed to treat hyperthyroidism should help normalize thyroid levels.
This means that the symptoms of thyrotoxicosis can be used as a marker to determine if you are getting adequate treatment for your hyperthyroidism.
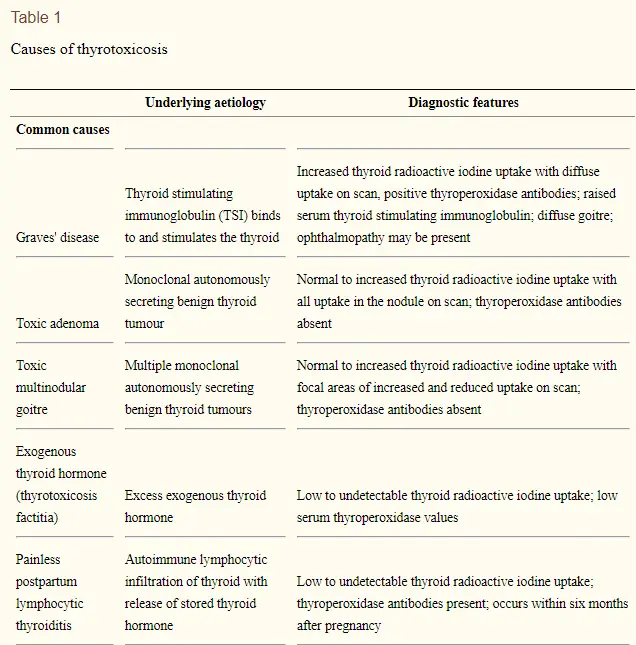
Causes of Thyrotoxicosis
Now that you understand what thyrotoxicosis is, it’s relatively easy to talk about the conditions that may cause this problem.
It can be the result of any condition which results in hyperthyroidism and which isn’t treated accurately.
Remember, the entire goal of treating hyperthyroidism is to reduce the impact of thyroid hormone on your body.
You can find a list of the most common causes of thyrotoxicosis below:
- Graves’ disease (5): The most common cause of thyrotoxicosis is Graves’ disease. This autoimmune condition of the thyroid gland results in excess production of thyroid hormone due to antibody stimulation.
- Toxic multinodular goiter (6): Rarely, some goiters can autonomously produce thyroid hormone. If this happens they are referred to as toxic nodules. This condition is uncommon as most thyroid nodules do not produce thyroid hormone and are completely benign.
- Thyroiditis: Thyroiditis literally means inflammation of the thyroid gland and this condition can result in excessive production of thyroid hormone. Any condition which causes inflammation also causes damage and this damage may cause the ‘leakage’ of thyroid hormone into the bloodstream. Conditions such as Hashimoto’s thyroiditis, subacute thyroiditis, postpartum thyroiditis, and so on can all cause thyrotoxicosis. The good news is that many of these conditions resolve on their own without treatment (with the exception of Hashimoto’s thyroiditis).
- Thyroid medication (7): Your body can produce too much thyroid hormone on its own but you can also take too much thyroid medication by mouth. This condition tends to arise from people who take too much thyroid medication or the wrong type of thyroid medication. The good news is that simply dropping your dose of thyroid medication is usually enough to resolve the issue. You can prevent thyrotoxicosis from occurring in this setting by regularly checking your thyroid lab tests.
- Prescription medications (8): Certain prescription medications (such as Amiodarone and amphetamines) can stimulate thyroid hormone production or damage the thyroid gland. Damage to the gland, much like damage from inflammation, may cause the excessive release of thyroid hormone into your bloodstream. This is rare, but should be considered with certain medications!
Symptoms Associated with Excess Thyroid Hormone
Believe it or not, it’s actually hard to miss the diagnosis of thyrotoxicosis because the symptoms are almost impossible to miss!
This is both a good and a bad thing.
Good in the sense that you should be able to identify the problem and know if your treatment is working.
And bad in the sense that you may feel poorly while you are undergoing treatment and diagnosis.
The symptoms associated with thyrotoxicosis include:
- Weight loss (due to stimulation of metabolism)
- Heart palpitations (due to stimulation of heart tissue)
- Heat intolerance (due to excessive heat production by your body)
- Fatigue
- Hair loss
- Anxiety
- Tremors
All of these symptoms occur from overstimulation of your cells by thyroid hormone.
They should completely resolve as you undergo treatment!
If your symptoms persist despite starting treatment then this may be an early indication that your treatment is not enough.
How is Thyrotoxicosis Diagnosed?
You can easily diagnose thyrotoxicosis with an evaluation of clinical signs and symptoms and with the use of specific laboratory tests.
If you have this condition then you will definitely experience some or all of the side effects that I’ve mentioned above.
In addition, the effect of excess thyroid hormone in the body causes specific changes that can be picked up through routine laboratory testing.
As thyroid hormone levels increase your TSH will start to decline. In addition, your free thyroid hormone levels will start to rise.

This pattern is observed in almost all cases of hyperthyroidism and thyrotoxicosis and can be a very helpful tool for identifying the condition.
Ask your doctor to order these tests if you suspect thyrotoxicosis or hyperthyroidism:
- TSH (thyroid stimulating hormone): Your TSH will most likely be very low or close to zero.
- Free T3 (triiodothyronine, free): Free T3 will likely be elevated or high-normal.
- Free T4 (thyroxine, free): Your free T4 may be normal or low.
- TSI (thyroid stimulating immunoglobulin): If you have Graves’ disease then your TSI may be elevated. You should always check for this antibody if you suspect you have hyperthyroidism because it is the most common cause of that condition.
There is one other condition worth mentioning here which can confound your interpretation of thyroid lab tests and that is the condition of subclinical hyperthyroidism.
This condition results in a slightly lower than normal TSH but your free thyroid hormones (free T3 and free T4) are normally within the normal reference range.
If you have this condition you may also experience minor symptoms of thyrotoxicosis but these symptoms are often not extreme enough to bring you to the Doctor.
Symptoms such as minor fatigue, minor hair loss, minor changes in bowel movements, and so on can be confused with other conditions.
There is a lot of conflicting information regarding whether or not this condition should be treated, but I wanted you to be aware of it in case your lab tests don’t fit this ‘typical’ pattern.
Treatment Options
The entire goal when treating this condition is to focus on reducing the impact thyroid hormone has on your cells while also attempting to reduce the total amount of circulating thyroid hormone.
This can be accomplished in several ways and you may need one or more of the therapies listed below:
- Thyroid blocking medications (9): Usually the first line of treatment for excess thyroid hormone is to attempt to prevent your thyroid from creating more thyroid hormone and to block its metabolism or conversion in the cells. This can be done with the use of anti-thyroid medications such as methimazole, PTU, and beta blockers. These should always be the first step in treatment because they are not permanent solutions and you can always be more aggressive over time if necessary.
- Thyroid surgery: If anti-thyroid medication fails then you may need to have your thyroid gland completely removed. This procedure is known as thyroidectomy and it can be used to treat hyperthyroidism. One downside to this procedure is that you will be required to take thyroid medication by mouth for the rest of your life afterward, but this may be preferable to suffering from the side effects of thyrotoxicosis.
- Radioactive iodine ablation: Another option if thyroid medication fails is to undergo radioactive iodine ablation. This procedure results in the destruction of your thyroid gland through the use of radioactive iodine. After this procedure, you will also be required to take thyroid medication by mouth because your thyroid gland will no longer be functioning.
- No treatment at all: In some cases, especially in certain cases of thyroiditis (10), you may not need treatment at all for your symptoms. These conditions may result in a reversible cause of thyrotoxicosis that will completely go away over time. This is the best-case scenario and it doesn’t happen often, but you should be aware of it.
Side Effects and Consequences of Thyrotoxicosis
What happens if you don’t get treatment or what happens if you don’t get enough treatment?
It’s helpful to think of thyrotoxicosis as a toxic condition for your cells that may lead to serious long-lasting conditions if not treated appropriately.
It is dangerous for this condition to be left unchecked because it can result in permanent damage to certain tissues in the body.
The most concerning include your bones and your heart tissue.
- Bone Loss and Osteoporosis – Untreated thyrotoxicosis can lead to osteoporosis. This condition is serious because it can potentially lead to early fractures, hospitalizations, chronic pain, and an increased risk of infections. Excess thyroid hormone increases bone cell turnover (11) which reduces the stability and strength of your bones. This risk seems to only be prevalent in women who have gone through menopause. Some studies show that women who are menstruating may be protected from this consequence (12).
- Cardiac Enlargement – Another serious problem is that excessive thyroid hormone can stimulate your cardiac (heart) tissue and result in an enlarged heart as well as changes in blood pressure (13). As your heart enlarges it may increase your risk of heart disease, the development of arrhythmia, heart failure, and lead to premature death.
Don’t let these side effects scare you! They can both be prevented with early diagnosis and treatment.
Thyroid Storm vs Thyrotoxicosis
Lastly, it’s important to differentiate between the condition of thyroid storm and thyrotoxicosis.
These conditions are related in that thyrotoxicosis can lead to thyroid storm, but they are different entities entirely.
Thyroid storm is a life-threatening medical emergency that can result from excessive stimulation of your cells by thyroid hormone.
It occurs in about 1-2% of people who have thyrotoxicosis and has a fairly high mortality rate (14).
Thyroid storms can almost always be prevented as long as thyrotoxicosis is treated adequately with the therapies listed above.
Rarely, it can occur spontaneously by various factors that may be out of your control.
You can learn more about this condition here.
Conclusion
Thyrotoxicosis is a serious condition that results from the impact of thyroid hormone on the cells in your body.
This condition often arises from the same conditions that cause hyperthyroidism.
When treating thyrotoxicosis the goal should be to reduce the damage that thyroid hormone is causing your cells by reducing total thyroid hormone and cellular thyroid conversion.
By using this strategy you will be able to avoid long-term serious side effects and consequences of this disease.
You can prevent this condition by ensuring that your hyperthyroidism is well managed which can be done either naturally or with the use of thyroid medications.
Scientific References
#1. https://www.ncbi.nlm.nih.gov/books/NBK482216/
#2. https://www.ncbi.nlm.nih.gov/books/NBK482216/
#3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3475282/
#4. https://www.ncbi.nlm.nih.gov/pubmed/26926973
#5. https://www.ncbi.nlm.nih.gov/books/NBK285567/
#6. https://www.ncbi.nlm.nih.gov/pubmed/18357484
#7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4560848/
#8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5697581/
#9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5424485/
#10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996955/
#11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4314789/
#12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4309145/
#13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3832836/
#14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998648/


I had all my thyroid removed about 7 years ago. I’ve had my dosage adjusted a few times but I recently developed the awful symptoms again of hyperthyroidism. I have gone from .175 down to .137 and I felt I was getting back to normal but all the symptoms are still there. I even skipped a daily dose thinking I could get some relief from the palpitations, diarrhea, shakiness, being so out of breath and severe fatigue. It’s been a week and it hasn’t helped at all. My question is how long does it take, once you reduce a dosage. to get back to normal? Of course I mean if it’s the proper amount that was adjusted.
Hi Lori,
Usually within a few days but it could theoretically take up to 2 weeks in some cases.
I was initially diagnosed with hyperthyroidism with large thyroid nodule. Biopsy showed benign, consistent with benign follicular nodule. Within eight months thyrotoxicosis, unspecified without thyrotoxic crisis or storm was determined. Both PCP and endocrinologist, along with otolaryngologist suggested a total thyroidectomy. I am now trying to acquire the correct dose of Synthroid (125mcg) medication to reduce symptoms.
I am thankful that I found your web site with the wealth of information that you are supplying to patients. I will have my first appointment with the endocrinologist and will insist that he follow your Thyroid Lab Tests protocols listed on your site. I will also be ordering your Thyroid Supplements for a Total Thyroidectomy Support. Thanks for your help.
Hi John,
It sounds like you are on the right track!
I had TT in 2018 because of multinodulr goiter and had been pressing on my trachea. I was put on 100mcg of synthroid since and was doing ok until recently when i started to feel symptoms of palpitations, fatigue , chest pressure which prompted my endo to aso refer me to cardiologist. My blood work shown hypothyroid with low tsh im not sure how low..and my endo lowered my synthroid to 50mcg every sunday and keep the 100 on the other 6 days , i was also put on metoprolol for the tachy. But initially the tachy didnt go away even with the cardiologist doubled my dose for metoprolol. I talked to my endo again and felt im over medicated so he lowered my dose to 88mcg daily..it seemed to help with the palpitations and its my 3rd day now but i still feel other hypo symptoms like fatigue, cold intolerance, and anxiety as well! Im just hoping this is the right dose how many weeks will it start to normalize levels and feel better?
Hi MJ,
If you are on the right dose you should notice some improvement within 2-6 weeks, typically.
How do you know if you are on the right dose? Do i just endure the anxiety and other symptoms till my thyroid levels even out?
Hi MJ M.
If you are on the right dose then your symptoms should subside or fade away 🙂
thank you Dr Childs, 6th day now on the lower dose of synthroid ( from 100 mcg to 88 mcg ) I notice some improvements but the fatigue is too much. I am worried going back to work next week that I still feel worse and cant function. Is fatigue something the body go through with synthroid dose change? will this also improve within 1-2 weeks. I know im impatient.
Just recovering from a bout of … thyroiditis, I guess?
Had an episode 10 years ago after contracting a bad stomach bug in India (lost a stone in 4 days, had tachycardia for weeks and some neuropathic symptoms)
This time: end of January 2021:
out of the blue:
first few days: rash on left side of my nose/cheek, sudden need-to-run-to-the-bathroom diarrhoea, hardening of the lower abdomen, nausea, itchy all over and weak
Initial symptoms (first 2 weeks):
* 5Kg (9%) weight loss,
* body fat: 28% reduced to 12% (that is not a typo) (!)
* palpitations
* fast breathing rate (even during tai chi)
* breathlessness on usually small efforts (like going upstairs)
* weakness – had to walk slowly and unsteadily like a 90-year-old
* insomnia (hard to get to sleep at night, at times not until 6am)
* HR about 95bpm lying in bed (mornings); 140 doing tai chi /walking (!)
* HRV very low: 20s to 30, but even as low as 19! (it is usually around 60 – based on daily measurements for the last 8 years)
At 6 weeks:
* TSH < 0.5 TSH; (last summer it was: 2.2)
* FT3: normal-high (6.3; top of normal is 6.5),
* FT4: normal (bang-on-in-the-middle-of-the-range)
* Antibodies were not measured
* Total T3 also not measured
* ALT (liver panel) elevated: 85 (normal range: 2-53) – post-viral?
* HR 80 (improved, not yet normal)
* HRV 48-50 (improved, not yet normal)
* body fat back to 20% (on same machine as usual, fine with me)
* oxygen saturation: 98, perhaps also 93 at times
Feel better & stronger now but I wonder what caused this this time round – did I do the right thing waiting or should I have sought medical advice earlier…
Perhaps COVID? (thinking of the rash, red soles of feet, ALT value, digestive issues – none of the usual parasites like giardia were found)
Is an ECG warranted?
Does taking too much liothyroine cause weight gain or thyroid storm? Mine is around 6
Range is 2-5
Thanks
Hi Nikki,
Taking too much liothyronine can certainly lead to hyperthyroidism and hyperthyroid-like symptoms. It could trigger a thyroid storm in the right situation.
Rarely, I have also seen T3 lead to weight gain.
From your experience, is there any link between a toxic nodule and a Grave’s disease diagnosis? 8 years ago, I had a nodule (2.4cm x 1.6cm x 2.1) discovered & biopsied. It was benign. My labs were all normal. Fast forward to spring 2022, and I developed all the symptoms of thyrotoxicosis. Labs ultimately showed high TSI and non traceable TSH, T4, T3, T4 free & T3 free all high. Thyroid U/S showed the nodule had remained stable from previous images. Thyroid uptake scan revealed the nodule to be toxic. I am currently awaiting further advice regarding treatment from my NMD, along w an endocrinologist consult.
Is it possible that the toxic nodule is the cause of the Grave’s , and if a toxic nodule is removed, could the Grave’s potentially resolve? I am treating my conditions naturally at this time with gluten-free, dairy free, sugar free diet & supplements, and desire to NOT have RAI or thyroidectomy. What are potential treatment options in my case?
Hi Kristin,
Toxic nodules and Graves’ disease typically do not coexist. A toxic nodule is a piece of thyroid gland tissue that is not responsive to normal input whereas Graves’ disease is an autoimmune hyperthyroid state mediated by the immune system so the underlying cause of each is quite different. There have been cases where Graves’ disease occurs after treatment for toxic nodules but I’m unaware of a direct connection between the two.
I hope you can help me figure out my thyroid issue. My most recent blood work results shows my Thyroxine Free is 0.75,(L) my TSH w/FT4 Reflex is 10.61 (H),and TSH ( 3rd Generation) is 11.38 (H) which my doctor says is hypothyroidism.
My problem is in the past when I’ve taken that Levothyroxine it cause serious side effects of vertigo so bad I had to go the ER. Plus my heart would beat hard, terrible heartburn, and too I’d be a nervous wreck and that’s on the lowest dose. Even on a half a tablet I felt bad so I just quit taking it. This was back in September of 2022 and I felt back to normal until December. I noticed my heart would beat hard, was angry and irritable, just felt my nerves were on edge. I went to the ER on December 10th and my blood pressure and 165/100 and my heart rate was 110 or so. They said it was my thyroid and got nothing to for my blood pressure or to lower my heart rate. Got some results on December 26th from that ER visit that I had tachycardia with sinus arrhythmia. Had to go back to ER on New Years thinking I had pneumonia and again my blood pressure and heart rate were high but turned out to be viral upper respiratory infection. Still I asked about getting something for my heart rate blood pressure and the doctor said no because of side effects. After that I decided to get a blood pressure monitor. On January 12th after a series of upsetting incidents I took my blood pressure at 4:30 and and it was 165/103 with 117 heart rate. By 8:00 I called an ambulance because my heart rate was so bad and couldn’t breathe good had tightness across my back and numbness in my left hand.
So after all that and and getting CT for a possible pulmonary embolism (was negative) I stayed overnight in the hospital to be monitored because my heart rate was above 100 for 10 hours straight. 3 different doctors brought up my thyroid and I explained it to them and one said there’s a thyroid medication you can take that helps T3 and T4.They ended up giving me Metoprolol 25mg to help my blood pressure and heart rate stay low.So when I went to my primary care doctor on the 18th she put me on 30mg of NP Thyroid medication. I took it first thing in the morning but noticed after 45 minutes my heart rate was 104 when I’d take my blood pressure. This went on for 6 days. I decided to look at all my lab results and found on that CT scan I have a thyroid nodule on the right side of my thyroid. I researched it and found about how those can leak thyroxine in your bloodstream and cause hyperthyroid symptoms.
I checked and I have 9 hyperthyroid symptoms compared to 3 hyperthyroid symptoms. So my lab results I showed you at the the beginning of this message don’t match what’s going on with me physically. It’s really frustrating. I’m not taking the NP Thyroid medication and have done well on the Metoprolol.I see my cardiologist tomorrow in regards to what my results from wearing a GIO heart patch for 5 days are. What is your theory on all this? What do I have in regards to my thyroid? Please let me know. Look forward to hearing from you about this issue!Thx!