I can’t think of a more scary headline for a thyroid patient than to hear that the very thyroid medication they are taking may be associated with a heart attack.
This is especially important when you consider that heart attacks tend to impact older generations and that up to 25% of people over the age of 60 have a thyroid problem (1).
But is there really a connection between using thyroid medication and your risk of a heart attack?
Sort of, but it’s much more complicated than you might think.
There’s no question that there is a complex and intimate relationship between thyroid function and heart function and when there is an imbalance in your thyroid it will impact your heart.
But that doesn’t guarantee that you will get a heart attack and it certainly doesn’t guarantee that the medication you are taking will increase your risk.
Let’s talk more about the connection between your thyroid and your heart, how it impacts your risk of heart attack, which thyroid medications are considered to be safe, and much more.
Will Taking Thyroid Medication Give You A Heart Attack?
First off, let’s answer the question about whether or not taking thyroid medication can trigger or cause a heart attack.
The answer is yes, but only if you are grossly misusing your thyroid medication and only if you have underlying problems already present.
Here’s what I mean:
Thyroid hormone directly impacts the heart tissue which means that it has the potential to increase both heart rate and the force of contraction of your heart.
In other words, taking thyroid medication can increase how quickly your heart is beating and how strong each beat is.
But beyond this, there is a very important and complex relationship between thyroid function and your overall heart health (2).
To give you a better idea of what I’m talking about here are just a few ways that your thyroid helps to regulate heart tissue:
- By impacting the flow law which directly impacts multiple cardiac parameters (blood pressure and heart rate).
- By impacting the structure of the heart and its conduction system (remember your heart is a massive electrical conduction system).
- By impacting the autonomic nervous system (both the parasympathetic and sympathetic nervous systems).
- By impacting the renin-angiotensin-aldosterone (RAAS) system.
- By impacting vascular compliance.
- By impacting vasoreactivity.
- And by impacting renal (kidney) function.
You don’t need to understand what exactly each of these functions means but you should understand that your thyroid is required if you want to have a healthy heart.
You should also understand that if your thyroid is dysregulated either because your thyroid is too high or too low that will have a negative impact on your heart.
I think it’s best to think about it like this:
A healthy thyroid means a healthy heart.
Yes, other problems can arise with your heart from outside of your thyroid but as long as your thyroid is optimized then you know those problems aren’t coming from your thyroid.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Understanding Heart Attacks & What Causes Them
With that in mind, I want you to think about the average person and their risk of a heart attack.
Heart attacks, referred to as myocardial infarctions, occur when you have a blockage of arteries that supply blood to the heart tissue itself.
There are many different causes of heart disease but the #1 cause of heart attacks in developed countries stems from a build-up of cholesterol in the arteries (3) that supply blood to your heart.
This is referred to as coronary artery disease and is really the thing you should be worried about if you are worried about your risk of a heart attack.
Cholesterol buildup in the arteries of your heart takes a long time to develop and it isn’t until they reach complete occlusion (or blockage) that you finally get your heart attack.
The rate at which your arteries build up this cholesterol is dependent on your genetics, general lifestyle, the foods you are eating, how much stress you are under, and underlying hormone imbalances (men and women develop heart attacks as their sex hormones decline).
Are you following me so far?
If you’ll notice what I said, I mentioned that it’s the build-up and the blockage of these arteries from cholesterol that causes the heart attack.
So let’s put this into perspective:
When your doctor says that thyroid medication may give you a heart attack they aren’t saying that the thyroid hormone is the cause of that heart attack, they are saying that it may precipitate the heart attack.
But let’s be clear:
Taking thyroid medication is not going to cause the build-up of cholesterol which is the underlying cause of most heart attacks!
In fact, there’s good evidence to suggest that the use of thyroid medication may balance your cholesterol and protect your heart.
For this reason, it doesn’t make sense to blame a heart attack on thyroid medication because it’s just the thing uncovering the underlying problem which is the cholesterol build-up.
Make sense?
Thyroid Medication and Its Impact On The Heart
Let’s talk more about how thyroid medication influences your heart, though, because this topic is important.
All thyroid medications have the potential to put a strain on your heart (4), especially if they are used incorrectly.
And it is this unneeded and unnecessary stress which may unmask the presence of cholesterol buildup much in the same way that a cardiac stress test can.
But the way that thyroid medication impacts your heart is no different from the way that doctors intentionally stress out your heart with a cardiac stress test.
Doctors will frequently place patients who they think have a risk of heart disease on a treadmill (5) to intentionally put stress on the heart.
During a stress test, doctors can see if blockages are developing in the heart tissue and how well oxygen is making it to your heart cells.
And, believe it or not, there are patients who do end up having heart attacks during their stress test.
But you wouldn’t blame the stress test for the heart attack, it was just the thing that uncovered the problem that already existed.
Does this mean that thyroid hormone is dangerous because it has the potential to put stress on the heart?
Not at all!
Your body needs that thyroid hormone (otherwise you wouldn’t have been given it!) and excess stress from thyroid medication can be avoided when the medication is dosed appropriately.
It’s absolutely the case that excessively high doses of thyroid hormone may put unnecessary stress on your heart but, as long as you are being dosed appropriately, this is not a risk you have to worry about.
We know this because healthy people have thyroid hormone flowing through their veins all of the time and their thyroid is not the thing that causes their heart attack.

And when your doctor gives you thyroid medication, he or she is trying to bring you to a normal state, not give you more than you need or less than you need (though they can make mistakes from time to time).
The bottom line?
If you are taking a normal physiologic dose of thyroid hormone then you don’t have anything to worry about.
Thyroid medication, if used correctly, will not increase your risk of heart disease.
In fact, it is far more likely to protect your overall heart health.
It does have the potential to unmask underlying heart disease but really only if your dose is too high.
The Relationship Between Hypothyroidism, High Cholesterol, and Heart Attacks
If you are someone taking thyroid medication then you are doing so to treat a condition called hypothyroidism or low thyroid function.
And if that’s the case, there’s a lot of evidence to suggest that not treating your thyroid is far more likely to increase your risk of a heart attack than using thyroid medication.
Here’s what I mean:
Low thyroid states result in high cholesterol.
In other words, the lower your thyroid function is the higher your cholesterol will be (6).
Thyroid hormone is responsible for helping your body to break down and metabolize cholesterol.
When you don’t have enough thyroid hormone in your body, there will be a build-up of cholesterol which can then make its way to the places you don’t want it (such as your coronary arteries).
So, as you might suspect, treating low thyroid function should reduce your risk of heart attack and that’s exactly what we see in some studies.
Some studies suggest that early use of levothyroxine in conditions like subclinical hypothyroidism (7) may reduce the risk of a heart attack for some patients.
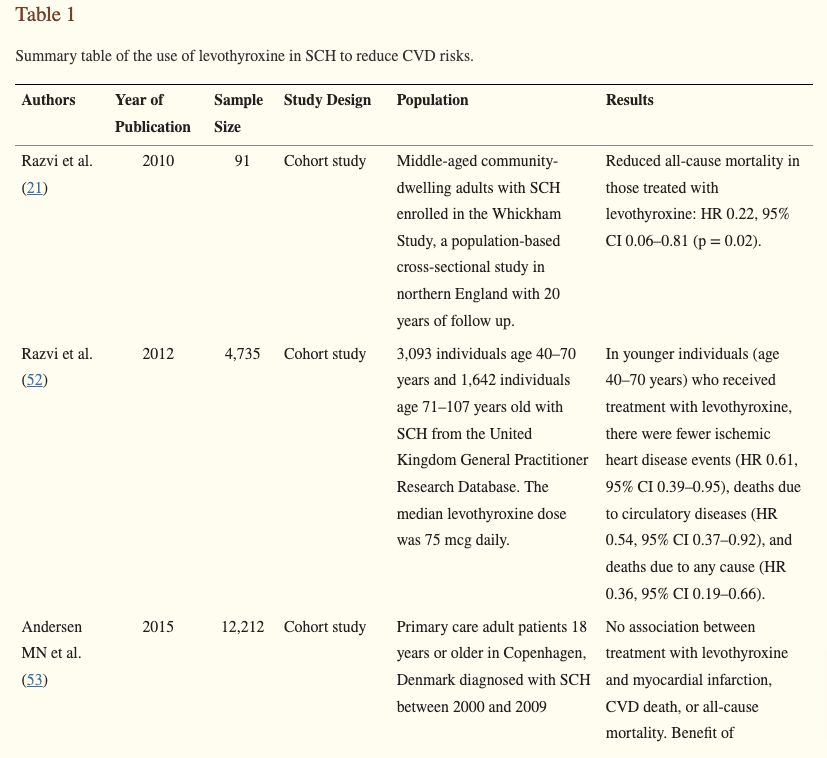
This suggests that even small changes in thyroid function are worth treating and their treatment prevents heart-related complications.
To be fair, there are some conflicting data as to whether or not it’s a good idea to treat subclinical hypothyroidism (8) to prevent heart disease, but the greater point still stands:
Treating patients with true hypothyroidism does provide a benefit to overall heart health.
The Difference Between T4, T3, and T2 On the Heart
What about different thyroid medications? How do they impact your heart?
This is a really important topic so let’s spend some time understanding it.
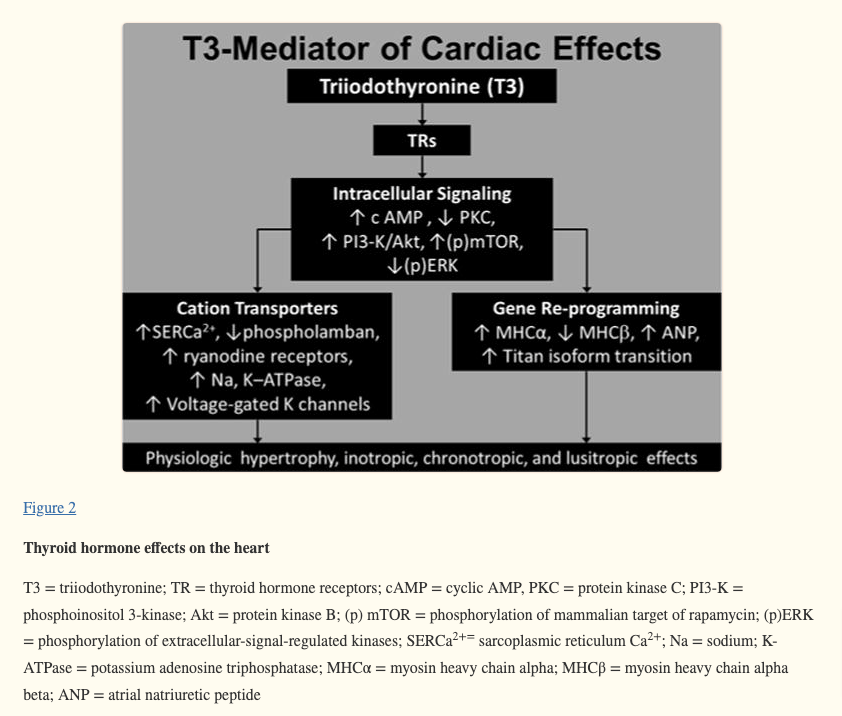
All of the major effects of thyroid hormones on the heart are mediated by T3 thyroid hormone (9).
This is very important because the majority of you reading this aren’t even taking medication that contains T3.
Most thyroid patients take T4-only thyroid medications like levothyroxine or Synthroid.
This means you aren’t even taking the type of thyroid hormone that has the potential to impact your heart directly!
In order for your levothyroxine to have any impact on your heart, your body must first convert it into T3 thyroid hormone through the thyroid conversion process.
This means that an extra step is required before your medication can impact your heart.
As far as thyroid medications go, T4-only thyroid medications like levothyroxine and Synthroid tend to have very little direct impact on the heart.
This is not true of medications that contain T3 thyroid hormone.
If you are taking a thyroid medication that contains T3 such as Armour thyroid, NP Thyroid, Cytomel, or liothyronine, just to name a few, then those medications can have a direct impact on the heart without the need for thyroid conversion.
This is why these types of medications tend to result in heart palpitations much more frequently than medications that only contain T4.
In addition, these medications also tend to have a more pronounced effect on heart rate which is why I recommend keeping track of your heart rate while using them.
This does not mean these medications are dangerous, though, it just means that they should be used with care.
Some doctors will tell thyroid patients that T3 medications should be avoided because they cause heart attacks but this isn’t true either.
Yes, they do have a slightly higher risk of unmasking existing heart problems compared to thyroid medications like levothyroxine but as long as you are not taking an excessively high dose or pushing yourself into a hyperthyroid state then the risk is essentially non-existent.
Remember:
The body naturally produces both T4 and T3 thyroid hormones so replacing both of these hormones if you don’t have enough is quite safe.
Similar to T3 thyroid hormone, T2 thyroid hormone does appear to have an impact on the heart tissue.
This effect is only seen with very high doses of T2 (10) (around 800 mcg per day) which is far higher than any thyroid patient would typically get.
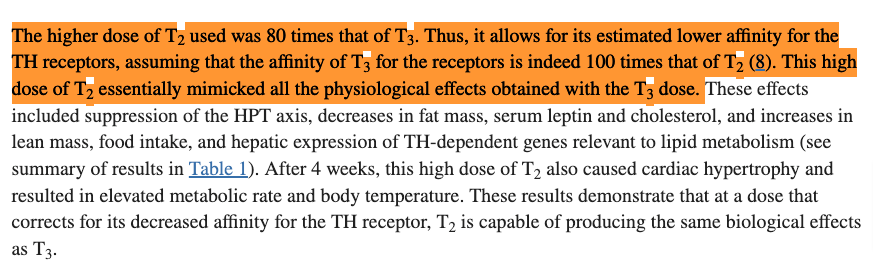
For reference, my T2 thyroid support supplement contains 100 mcg of T2 in each capsule which means you’d have to take 8 capsules each day for months on end before you’d even put yourself at risk.
This would be true of any thyroid hormone, though, as you can imagine that taking 8 times your dose of levothyroxine or liothyronine would have similar effects on your health.
Heart Palpitations Don’t Automatically Mean Your Dose is Too High
Many thyroid patients, perhaps even you reading this right now, have experienced heart palpitations after taking thyroid medication.
While they may feel scary and unpleasant, heart palpitations are almost always harmless (11).
A heart palpitation is just the sensation that your heart is beating in your chest.
Because thyroid medication can increase both the rate of contraction and the force of contraction of the heart, it’s not uncommon for thyroid patients to experience heart palpitations on occasion, especially after taking thyroid medications that contain T3.
But what you need to know is that having a heart palpitation is not the same as having chest pain or experiencing a heart attack and most heart palpitations are 100% harmless.
That doesn’t mean they are always harmless, though, which is why you should always get them checked out if you are experiencing them.
If your heart palpitation is related to your thyroid medication it will tend to fade within a few hours as your body uses and metabolizes the thyroid hormone that you just took.
Should You Worry? Not If Your Dose is Optimized
In summary, while thyroid medication does have the ability to impact your heart, this effect is almost always beneficial and not harmful.
There are rare situations in which pushing your body into a hyperthyroid state or taking too much thyroid medication may negatively impact your heart health, but this can be avoided by ensuring that your dose is adequate.
In rare situations, it’s also possible for the use of thyroid medication to unmask underlying heart disease but this is also very rare and is not something that thyroid patients really need to worry about.
Now I want to hear from you:
Are you concerned about the connection between thyroid medication and your heart health?
Do you have a personal history of heart disease?
Do you feel that your thyroid is playing a role in your cholesterol metabolism or cholesterol level?
Are you planning on making any changes to your thyroid routine after reading this?
Leave your questions or comments below!
Scientific References
#1. nature.com/articles/s41598-019-49540-z
#2. ncbi.nlm.nih.gov/pmc/articles/PMC6851449/
#3. ncbi.nlm.nih.gov/books/NBK537076/
#4. accessdata.fda.gov/drugsatfda_docs/label/2012/021924s006lbl.pdf
#5. cdc.gov/heartdisease/coronary_ad.htm
#6. pubmed.ncbi.nlm.nih.gov/35038435/
#7. jamanetwork.com/journals/jama/fullarticle/2768464/
#8. ncbi.nlm.nih.gov/pmc/articles/PMC7609906/
#9. ncbi.nlm.nih.gov/pmc/articles/PMC4318631/
#10. ncbi.nlm.nih.gov/pmc/articles/PMC4272398/
#11. pennmedicine.org/updates/blogs/heart-and-vascular-blog/2019/december/heart-palpitations