If you’ve been diagnosed with hypothyroidism or you suspect you have hypothyroidism then this is the post for you.
The world of hypothyroidism can be a confusing and conflicting place.
Learn all of the updated information relating to hypothyroidism treatment and management in this guide with references to the newest scientific research and studies.
This guide will walk you through everything important and relevant to thyroid function to help you become an advocate for your own health and help you discuss your thyroid with your physician.
Everything you Need to Know About Your Thyroid
Why do we even need a guide to help understand thyroid function?
If you have just been recently diagnosed you will notice that there is a lot of information about thyroid function on the internet.
Some of this information is good and some of it is not so good.
Separating the important and good information from the bad information becomes very important!
This guide contains information that is backed by scientific research with links to relevant clinical studies to the claims made.
This means you can be confident in knowing that this information is sound and helpful.
Much of the information contained in this guide also comes from my personal experience in treating hundreds and hundreds of patients.
The reason your thyroid is so important is that it influences almost every major hormone system in your entire body (1).
Small changes to thyroid hormone in the serum will, therefore, lead to huge changes in your quality of life.
These changes may be manifested as low energy, weight gain, inability to sleep well at night (and many more which we will discuss below) which all may influence your quality of life.
The problem?
While these symptoms may not ultimately kill you or lead to serious injury they impact your ability to live!
With that in mind let’s jump in:
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Hypothyroidism in a Nut Shell
Hypothyroidism refers to a condition in the body where an insufficient amount of thyroid hormone is produced naturally by your body (2).
This insufficiency can range from life-threatening levels (you need thyroid hormone to survive) to small deficiencies that lead to poor quality of life and everything in between.
The deficiency in your body depends on YOU and it will be different from individual to individual.
It’s helpful to think of thyroid function on a spectrum of 0 to 100:
On one end you have 0 thyroid function which results in death if not treated.
On the other end, you have 100 which means you are living happily with zero quality-of-life issues.
In the middle (let’s say around 50) you have a ‘living but not thriving situation’ where you may experience symptoms such as 20-30 pounds of weight gain, energy levels that lead you to rely upon caffeine to stay alert, brain fog that makes your work inefficient and various other symptoms such as intolerance to cold and even constipation.
Your goal in treating thyroid dysfunction should be to achieve a ‘thyroid level’ as close to 100 as possible!
This will leave you with an optimal quality of life.
Don’t worry – we will discuss how to achieve this level later in this post but for now, just realize what your goal of treatment should be.
Hypothyroidism can also be referred to as having a “sluggish thyroid” a “slow thyroid” or “low thyroid function” – but don’t be fooled, these are all names for the same condition.
This condition should be differentiated from HYPERthyroidism (3) which is the exact opposite condition.
Hyperthyroidism refers to TOO much thyroid hormone floating around in your body which presents with different but in some ways similar symptoms.
What Causes Hypothyroidism?
Finding out what is causing decreased thyroid function in your body may be one of the most important aspects of thyroid function.
Why?
Because some cases of hypothyroidism may actually be reversible and, therefore, treatable.
This isn’t true of all of the causes but it may be true for many, many patients.
Even if your condition isn’t completely reversible you still may be able to influence thyroid function and reduce your reliance on thyroid medication.
So what causes thyroid function?
It turns out that the most common causes of hypothyroidism in the United States stem from what is known as primary thyroid disorders (4).
Primary thyroid disorders mean that there is something wrong directly with your thyroid gland itself.
If your thyroid gland is damaged in any way then your ability to produce thyroid hormone may be compromised.
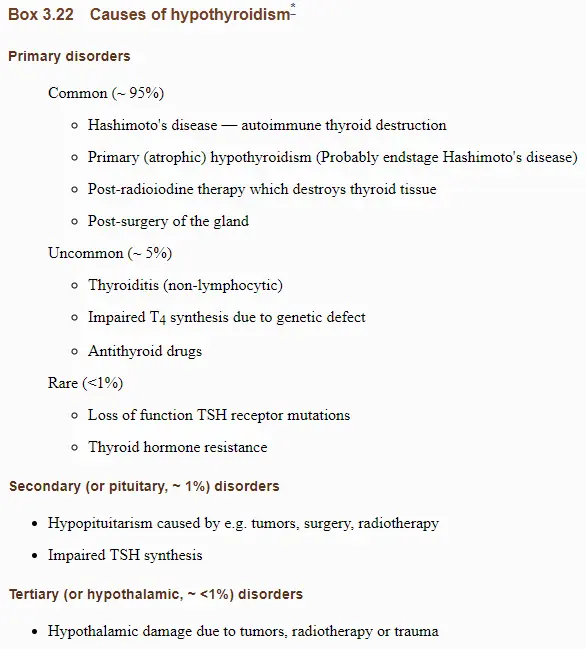
And these primary disorders account for 95% of hypothyroidism cases! (5) This means that there is a very high chance if you have thyroid issues it’s caused by one of these issues.
So what causes damage to your thyroid gland?
The most well-studied causes of hypothyroidism include:
- Hashimoto’s Thyroiditis (an autoimmune condition) – In this condition, the thyroid is destroyed by an autoimmune disease (6) where the body attacks your own thyroid gland and slowly causes damage over time.
- Primary Atrophic Hypothyroidism – This is felt to be caused by end-stage Hashimoto’s thyroiditis (more on this below). Basically, if Hashimoto’s disease progresses unchecked over time (7) then it will eventually destroy your thyroid gland.
- Post Radioactive Iodine Ablation – This is a therapy designed to treat hyperthyroidism but the goal of this treatment is to destroy the gland which leaves the patient hypothyroid.
- Post-Thyroidectomy – Thyroidectomy refers to the complete removal of the thyroid gland and is used to treat patients with hyperthyroidism and/or thyroid cancer. The removal of the thyroid gland results in hypothyroidism because the body is no longer able to produce thyroid hormone on its own.
This isn’t the complete list however because there are emerging causes of hypothyroidism that are less established but will probably become more important over time as we learn more about them.
These conditions tend to result in sub-optimal thyroid function which is difficult to diagnose and manage on standard lab tests:
- Obesity or Weight Gain – Obesity and weight gain may cause changes to hormones such as leptin and insulin which interfere with cellular thyroid hormone action. It is well known that thyroid disease leads to weight gain but less known that obesity leads to thyroid processing issues (8).
- Chronic illness – Chronic illness (9) such as diabetes, hypertension, cardiovascular disease, etc. may cause thyroid disease. This condition may mimic a condition known as euthyroid sick syndrome or low T3 syndrome.
- Certain Medications – Many medications are known to interfere with thyroid medication (10) including commonly prescribed medications such as beta blockers for the treatment of high blood pressure and anti-diabetic medications to treat high blood sugar. This is important to consider as a potential cause of thyroid dysfunction in a society that is taking more and more medications.
- Calorie Restriction – Patients who undergo yo-yo dieting or excessive calorie restriction show signs of thyroid damage (11) with low circulating T3 levels and high reverse T3 levels in the serum. This is particularly important to consider in a society that is constantly trying to lose weight through dieting and over-exercising!
- Under Treatment of Existing Thyroid Disease – Some patients, even if a small percentage, may need higher than normal thyroid medication when compared to standard controls. The reference ranges for thyroid function are meant to include up to 97% of the population but this leaves up to 1-3% of patients who don’t fit the “standard” ranges and may, therefore, need more medication.
- Micronutrient Deficiencies – It’s becoming more clear that certain nutrients such as zinc, selenium, and iodine are all required for optimal thyroid function and conversion (12). Our current society and standard American Diet may make it difficult to obtain adequate amounts of these micronutrients which, therefore, may lead to sub-optimal thyroid hormone in certain people.
- Genetics and Thyroid Conversion Issues – It is well known that each of us is genetically different. It has been shown that up to 67% of circulating thyroid hormone and TSH concentrations are genetically determined (13). Emerging genetic science is exploring variations in genetics at the individual level known as SNPs (single nucleotide polymorphisms). These changes to DNA may slightly alter how each of us processes thyroid hormone and how we convert thyroid hormone in peripheral tissues. It’s conceivable that through genetic testing we may be able to figure out the best dose and type of thyroid medication that a person needs. It’s also perfectly reasonable to assume that because of these SNPs, we cannot apply a one-size-fits-all treatment paradigm to every single patient.
It is well known that the most common cause of hypothyroidism is due to the autoimmune disease known as Hashimoto’s thyroiditis.
However, in many cases, thyroid function may also be slightly impaired because of the other less well-known causes listed above.
For instance:
You may be suffering from Hashimoto’s but your thyroid function may be further compromised by a history of recurrent yo-yo dieting, slight micronutrient deficiencies, and changes to your DNA which may make your body less likely to convert T4 into T3 in peripheral tissues.
Making sense?
So with all of this in mind, how likely is it that you have hypothyroidism or some thyroid problem?
How common is Hypothyroidism? (Incidence & Prevalence)
The number of new cases of patients with hypothyroidism is increasing over time.
This phenomenon can at least partly be explained by advancement in testing and diagnostic ability, but there appears to be some other issue at play here.
Studies from other nations outside of the United States also report similar findings (including in the United Kingdom (14) and India (15)).
So just how common is hypothyroidism?
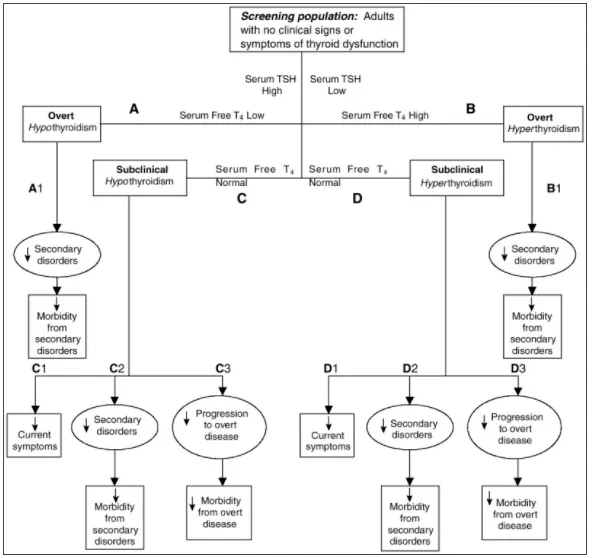
Well, it really depends on how you define hypothyroidism and which definitions you use.
If you use the diagnostic criteria of thyroid lab testing alone (known as biochemical hypothyroidism) then about 1 in 10 individuals (16) in the United States suffer from hypothyroidism.
By these standards, you have a higher risk of developing hypothyroidism if you are a woman and with increasing age.
If you include cases of subclinical hypothyroidism – meaning those patients who have abnormal lab tests but don’t meet the biochemical criteria for true hypothyroidism this number may jump up to around 20% of patients (10 percent from overt hypothyroidism and up to 10% of patients with subclinical hypothyroidism)(17).
So without including any other factors potentially up to 20% of the population may be suffering from some degree of thyroid dysfunction.
If you include patients who may have sub-optimal levels (let’s say from Obesity) but don’t meet the biochemical standard for diagnosis this number may be significantly higher.
The bottom line?
If you feel that you have the symptoms of hypothyroidism then serum testing is worth considering.
Do you have Hypothyroidism? Symptoms Guide
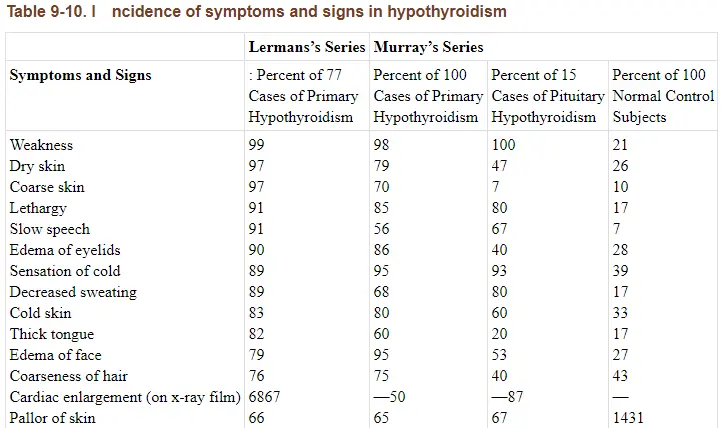
While there may be controversy surrounding the diagnosis and management of hypothyroidism there is very little controversy surrounding the symptoms.
And this is a good thing from the perspective of the patient.
Why?
Because symptom management may potentially allow a way for you to monitor your treatment and to determine if you are on the right treatment.
Let’s break this down:
If you suffer from hypothyroidism, and you have no known other medical conditions, and you are being treated with thyroid medication then the use of thyroid hormone should reduce or completely eliminate your symptoms.
This may seem very simple but it’s very powerful information…
If taking thyroid medication doesn’t result in an improvement in your hypothyroid symptoms then you can conclude 1 of 2 things:
#1. Your thyroid medication is insufficient (perhaps you are on the wrong type of medication or you are taking the wrong dose).
Or…
#2. Your symptoms are related to some other condition that is separate from thyroid function in your body.
In either event, your Doctor should be obligated to look further into your case and determine what issues may be contributing to your symptoms.
And this is why assessing your symptoms is so important.
It’s never normal for a person to have low energy, or to gain weight without changing their diet or to have cold hands or extremities or to suddenly develop constipation.
These are all potential symptoms of insufficient thyroid hormone in the body and they warrant further investigation.
If you suffer from these conditions and you KNOW (through lab testing) that you are hypothyroid then replacing that lost hormone should completely eliminate your symptoms.
If it does not then you need to go back up to #1 and #2 listed above to determine what the issue is.
So with that in mind let’s discuss the symptoms of hypothyroidism.
I’ve included a list of hypothyroid symptoms below for you to compare your symptoms against:
- Fatigue
- Lethargy
- Low endurance
- Slow speech
- Slow thinking
- Poor memory
- Poor concentration
- Depression
- Nervousness
- Anxiety
- Worrying
- Easy emotional upset
- Obsessive thinking
- Low motivation
- Dizziness
- Sensation of cold
- Cold Skin
- Decreased sweating
- Heat intolerance
- Non-restful sleep
- Insomnia
- Thick tongue
- Swelling of face
- Sparse eyebrows
- Low basal activity level
- Low basal temperature
- Slow resting pulse rate
- Long-normal intervals on ECG
- Swelling of eyelids
- Dry Skin
- Dry mucous membranes
- Constipation
- Weight gain unexplainably
- Paleness of lips
- Shortness of breath
- Swelling
- Hoarseness
- Loss of appetite
- Prolonged menstrual bleeding
- Heavy menstrual bleeding
- Painful menstruation
- Low sex drive
- Impotence
- Hearing loss
- Rapid heart rate
- Pounding heartbeat
- Slow pulse rate
- Pain in front of the chest
- Poor vision
- Weight loss
- Wasting of tongue
- Indistinct or faint heart tones
- Low QRS voltage on ECG
- Emotional instability
- Choking sensation
- Fineness of hair
- Hair loss
- Blueness of skin
- Dry, thick, scaling skin
- Dry, coarse, brittle hair
- Paleness of skin
- Puffy skin
- Puffy face or eyelids
- Swelling of ankles
- Coarse skin
- Brittle or thin nails
- Dry ridges down nails
- Difficulty in swallowing
- Weakness
- Vague body aches and pains
- Muscle pain
- Joint pain
- Numbness or tingling
- Protrusion of one or both eyeballs
- Brain fog
- Cardiac enlargement on x-ray
- Fluid around heart
It may surprise you that all of these symptoms may be associated with thyroid function in your body until you realize that almost every cell in your body has a thyroid receptor (18).
Because of this, the symptoms of hypothyroidism tend to be quite vast and vary from person to person making it potentially difficult to diagnose.
To make this information easier to digest I’ve also included the top 10 most common symptoms that patients tend to present with first and early in the disease process:
- Weight gain – Weight gain among hypothyroid patients is usually secondary to a reduction in metabolism and other hormone changes (19). This weight gain may be manifested by up to 10 pounds or as many as 50+ pounds depending on the severity of hypothyroidism.
- Depression or mood changes – Mood changes can also include anxiety or overall just not feeling like “yourself” (20). These mood changes tend to resolve with thyroid medication replacement.
- Changes to libido or sex drive – Low sex drive may be caused by changes to testosterone and other sex hormones as low thyroid hormone (21) may lead to low testosterone and/or changes to estrogen/progesterone. In addition, it appears that thyroid antibodies in Hashimoto’s may also impair sexual desire independently from their effect on thyroid function.
- Other hormone imbalances such as menstrual changes – Changes in the menstrual cycle include missed cycles, heavy flow, infertility, and even an increased risk for miscarriages.
- Fatigue or low energy – Thyroid hormone helps promote ATP production in the cells which are the energy currency in your body. Suboptimal ATP production may lead to the manifestation of fatigue.
- Intolerance to cold – Thyroid hormone helps promote energy production through a process known as thermogenesis (22). If thyroid hormone is low your total body temperature may drop (manifested as a low basal body temperature) which may increase your sensitivity to cold. Patients with this condition often wear sweaters in the winter or wear socks to bed because they are “always cold”.
- Muscle pain or joint pain – Hypothyroid patients may also experience muscle pain, trigger points, or chronic pain syndromes from low thyroid function. This connection may be due to the effects of thyroid hormone on ATP production in muscle tissues.
- Changes to your skin including dry skin, cracking skin, brittle nails, or rashes – Thyroid hormone is very important for the regulation of normal skin, and low thyroid status results in cystic acne and other skin conditions (23). Skin changes tend to be an early sign of hypothyroidism.
- Inability to concentrate, brain fog, or poor working memory – Much like depression and anxiety these symptoms tend to resolve upon thyroid hormone replacement.
- Hair loss or changes to your hair including dry and brittle hair – Hair loss and changes to hair quality tend to be noticed very quickly by patients and may be a very early indicator of thyroid disease. If you have hair loss for unknown reasons make sure to evaluate thyroid function. You can read more about the complex relationship between hair loss and thyroid function here.
Perhaps more important than the presence of these symptoms may be the degree to which you are experiencing them.
Remember that the severity of symptoms will vary from person to person and will ultimately depend on the level or degree of hypothyroidism in your body.
Let’s unpack this a bit:
Let’s say you experience weight gain because of your thyroid function. You may experience only 10 pounds of weight gain while someone else may experience up to 50 pounds.
The same concept holds true for energy levels:
One patient may only be slightly fatigued with energy levels in the 7 out of 10 range, while someone else may almost be bed-bound with energy levels in the 3 out of 10 range.

Consider also the example of constipation:
It’s never normal to have constipation for any reason, but the severity of constipation may vary significantly.
Some patients may be constipated and experience a bowel movement every 2-3 days while some other patients may only have a bowel movement every 5-6 days.
So in this way, your symptoms can not only help detect the presence of hypothyroidism in your body but they also may help determine the severity as well.
They should, of course, always be used in conjunction with lab testing which we will discuss below.
Controversy Surrounding Thyroid Diagnosis & Management Explained
You may be asking yourself why is this post so long and why is this information relevant.
It has to do with the current “standard of care” in treating thyroid disease.
The “standard of care” is a term used to describe how the majority of physicians treat any given medical condition.
The standard of care is always changing (based on medical studies and the preferences of physicians) but is something that drives the decision-making for medical conditions and therefore treatment.
When we dissect the standard of care over time for thyroid management we see some very interesting trends.
Initially, thyroid treatment from the standard of care (dating back to the 1920s)(24) was to start patients on 3 grains of natural desiccated thyroid hormone (like Armour Thyroid) and to increase the dose until the basal metabolic rate (metabolism) was normalized.
We will discuss the importance of various thyroid medications below but for now, just realize that Armour Thyroid is a thyroid medication that contains both the active thyroid hormone (T3) and the inactive thyroid hormone (T4).
With the development of thyroid lab testing measurements, the recommended dose of thyroid hormone decreased dramatically from the 1920s to the 1970s when T4 became the recommended treatment of choice (25) for hypothyroid patients.
This change was due in part to some patients experiencing cardiac palpitations on high doses of thyroid hormone and also in part due to the ability to measure thyroid lab tests in the serum.
What’s interesting is that while the recommended dose decreased over time there was an emerging subset of hypothyroid patients that reported persistent hypothyroid symptoms despite being treated with the new standard of care (more on that below).
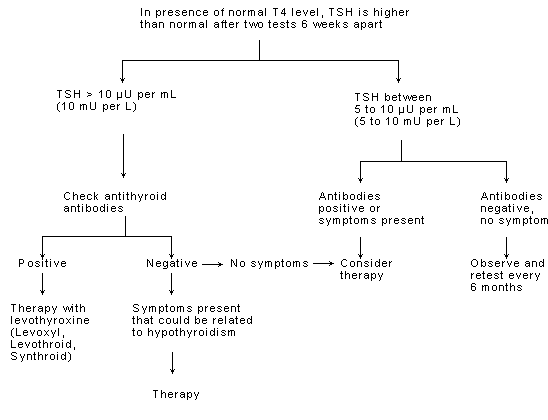
The current standard of care can be boiled down to a flowchart that looks something like this:
- Hypothyroidism is diagnosed based on an elevation in the TSH – if your TSH is > 5.0 you are considered to have subclinical hypothyroidism. If your TSH is > 10.0 you are considered to have hypothyroidism.
- If the patient is hypothyroid then start on T4-only medication such as Levothyroxine or Synthroid.
- Dose T4 medication based on the TSH down to a level of 1-2.
- Recheck labs every 8 weeks.
- If the patient is known to have Hashimoto’s recheck labs until TSH rises above 10.0 and then begin treatment with T4-only medication (known as the “wait and see” approach).
If this flowchart seems simple to you it’s because it is.
It’s difficult to believe that what we’ve discussed so far ranging from the complexities in the causes of thyroid function and the physiology of thyroid hormone in your body, that hypothyroidism can be treated in this way.
And it’s this treatment paradigm that may explain why so many patients are unhappy with their current treatment and remain symptomatic (up to 10-15% of hypothyroid patients)(26).
This standard of care does NOT take into account any of the other conditions that we’ve discussed previously:
- Individual Genetics – Each individual may differ in the amount of thyroid hormone produced, the effect of thyroid hormone at the cellular level, and so on.
- Peripheral Thyroid Conversion – Each person converts T4 into T3 at a different capacity (27). Those who convert more efficiently probably do better on T4-only medications while those who may have conversion issues due to SNP’s may do better on combination T4 + T3 medications.
- History of yo-yo Dieting – Excessive dieting reduces peripheral thyroid conversion and these patients often present with low T3 levels compared to normal body weight individuals.
- Presence of Hashimoto’s and how this influences thyroid function – People with Hashimoto’s often have symptoms of hypothyroidism but still maintain relatively “preserved” serum thyroid levels (28). These same patients tend to improve on thyroid medication.
- Existing co-morbidities – Medical conditions and the use of medications may alter thyroid function (29) in the body and alter the efficacy of thyroid serum tests.
- Exposure to endocrine disruptors – EDCs (as they are called) are ubiquitous and have been shown to alter circulating T3 levels without altering TSH levels in the serum (30). Certain individuals may be more susceptible to the effects of EDCs than others but it should still be considered.
- Reliance upon Lab Testing – In a world where multiple conditions range from individual genetics and exposure to endocrine disruptors it may be time to relax our reliance upon thyroid lab tests as the sole diagnostic measure of thyroid function in the body.
As a patient which kind of approach would you rather have?
It makes sense that a more individualized approach will always result in superior results when compared to a flowchart that is meant to work for every single patient.
The flowchart may be better for the physician in terms of time management and the ability to see patients, but it also may be the reason so many patients are unhappy with their current treatment.
Who uses the standard of care and conventional approach to thyroid management?
This approach is common among endocrinologists, family practice physicians, and most physicians (98%).
The alternative approach is generally followed by physicians who specialize in integrative or functional medicine.
I only provide this information so you know what to expect when looking into treatment options.
Don’t expect your Endocrinologist or family practice physician to take into account your genetics or thyroid conversion status.
If you want a more personalized approach you will need to look outside of conventional care (at least for the time being).
It is my belief that eventually all physicians will be taught this information in medical school or in residency but currently in order for a physician to have this knowledge, they must learn it on their own.
Thyroid Physiology 101 & Complete Thyroid Lab Testing
In order to have a more complete understanding of thyroid function and hypothyroidism, it’s also very important to discuss the serum lab tests that are used to assess thyroid function in your body.
You’ll notice that we are going to talk about more than just TSH or T4 here and that’s for good reason:
When most physicians look at your thyroid status they look at TSH and maybe T4 and then infer thyroid status based on these tests.

But these basic tests do not give insight into advanced thyroid measurements such as conversion status or thyroid hormone tissue levels.
Remember this important point:
Thyroid hormone exerts ALL of its actions on the CELLS in your body.
When we test for thyroid hormones in the blood we can only infer that if thyroid hormone is floating in your body it MAY be making it to its target destination.
But these serum lab tests don’t tell us about cellular resistance or about deiodinases that may interfere with thyroid hormone at the cellular level.
This phenomenon has been referred to in clinical studies as “tissue level hypothyroidism” (31) and is a term meant to describe a state in which the “serum or blood” levels of thyroid hormone tend to be normal but where the tissues in the body are not receiving sufficient thyroid hormone.
Tissue-level hypothyroidism may help explain why some patients feel poorly despite having a “normal” TSH.
We do have some surrogate tests that can help us determine if thyroid hormone is working at the cellular level and we will go over those below.
Let’s discuss the basics of thyroid physiology and why it matters for lab testing and treatment:
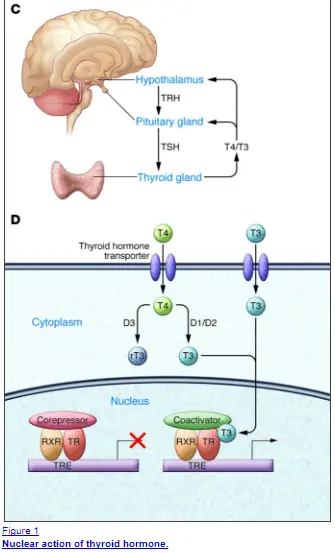
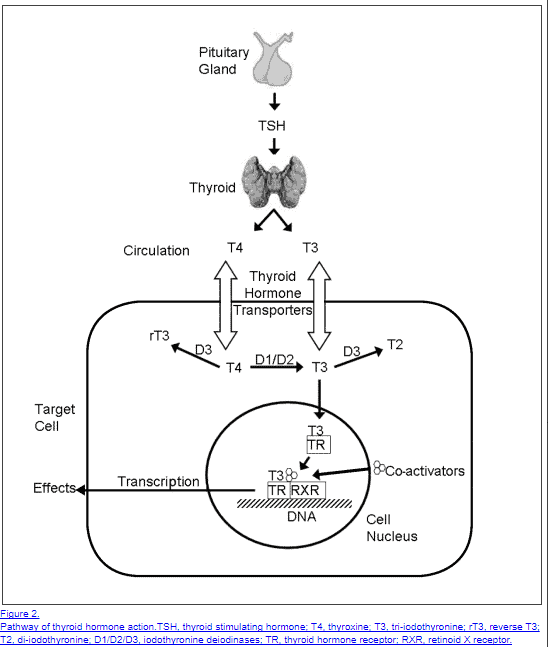
TRH (Thyrotropin-releasing hormone)
Thyroid physiology is complex but we can break it down as follows:
TRH is produced by your hypothalamus (a portion of your brain) in response to various triggers such as low circulating thyroid hormone in the bloodstream or due to environmental stimuli.
TRH then triggers a cascade of events that leads to the production of thyroid hormone from your thyroid gland.
In order to get there TRH kicks off the following sequences of events:
- TRH stimulates the release of TSH –> Changes in TRH may help us identify hypothalamic issues.
- TSH (thyroid stimulating hormone) is then produced by your pituitary gland (another portion of the brain) –> This is usually the only test that most physicians order but this only gives us insight into pituitary function.
- TSH which stands for thyroid stimulating hormone then acts on the thyroid gland which encourages the production and release of thyroid hormone
- Both T4 and T3 thyroid hormones are released from the thyroid gland and pumped into the bloodstream –> If the problem is at the thyroid gland itself then the production of both T3 and T4 may be low in the serum even if the TSH remains “normal”.
- Tissues (such as the liver and target tissues) either “activate” or “inactivate” thyroid hormone based on the needs of the tissues through the use of special enzymes known as deiodinases –> We can look at certain lab values to determine if your cells are using thyroid or not such as SHBG.
So why is this important?
We can basically use various serum lab tests to evaluate thyroid function at EACH individual step and determine how the thyroid is functioning at every step from TSH to cellular activation provided we know what to look for.
For this discussion, most people do not have significant issues with TRH because most people suffer from issues related to thyroid conversion or thyroid gland damage, but it’s important to discuss it nonetheless.
TSH (Thyroid stimulating hormone)
TSH is helpful in that it gives us insight into what is happening at the level of the pituitary.
In MOST cases of hypothyroidism, the TSH level will be ELEVATED.
In MOST cases of hyperthyroidism, the TSH will be SUPPRESSED.
This is also the test that most physicians order and use the most, but is it that valuable?
The TSH falls short for a couple of reasons.
Perhaps the most important is due to the relative differences in deiodinases in the pituitary versus in other cells in the body.
The deiodinases either activate or inactive thyroid hormone based on the needs of the tissues, but it turns out that the pituitary only has an “on” switch (32).
Compare this to other tissues that have both the “on” and “off” or “slow down” switch that they use to control thyroid function.
How is this important?
Because these enzymes compete with one another for the activation of thyroid hormone at the cellular level.
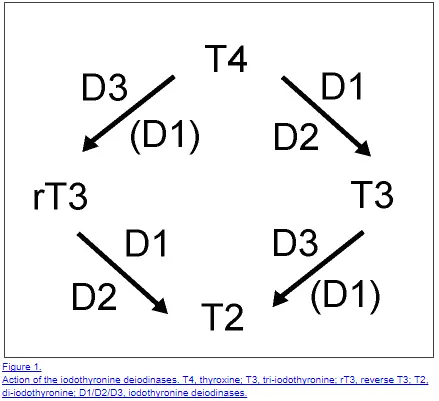
If you only have an “on” switch then there is no competition and it makes the body perceive more thyroid hormone than what may be available to other tissues.
In cases of elevated serum reverse T3, there may, therefore, be competition for thyroid conversion in specific tissues (33) which doesn’t exist in the pituitary gland and may not be reflected in serum TSH levels.
Does this mean that TSH is not a reliable or helpful test?
Not by a long shot – the TSH is still very valuable and should be ordered, but the weight that it carries may be altered based on various factors such as the serum reverse T3 level.
Free T4 (Thyroxine)
The T4 level in your body is an important measure of available thyroid hormone that can be used to either activate thyroid hormone or “slow down” metabolism by inducing the conversion of T4 to reverse T3.
T4 has 2 fates once it is produced in your body:
#1. Turn into the active thyroid hormone T3 by certain deiodinases in the liver and target tissues –> this is a good thing and we want this to happen.
#2. Turn into the inactive thyroid metabolite reverse T3 by certain deiodinases in target tissues –> If you are hypothyroid we don’t want this to happen or you are creating competition for binding on thyroid receptors in the body.
The activation or inactivation of T4 is referred to as “thyroid conversion” and this is a very important regulatory mechanism that occurs in the body and in certain tissues.
Why?
This conversion probably exists from an evolutionary standpoint as a way for the body to tightly regulate the amount of thyroid hormone that is being delivered to target tissues.
If you are in a state of starvation (as occurs in yo-yo dieting or calorie restriction) does it make physiologic sense for you to burn more calories at rest and deplete your fat stores that are critical for your survival?
Not really, which is why your body may preferentially turn OFF active thyroid conversion and turn ON inactive thyroid conversion (34).
The effects of reverse T3 may, therefore, block the beneficial effects on free T3 at the cellular level and lead to the symptoms of hypothyroidism.
T4 is important because T4 acts as the reservoir for this activation and the pool from which your body draws to convert thyroid hormone.
The serum T4 level is therefore important because if the “pool” of T4 is low then the amount of thyroid hormone being converted may also be low.
Free T3 (Triiodothyronine)
Perhaps one of the more important thyroid tests is the free T3 level which can be used as a marker for the amount of available and ACTIVE thyroid hormone in your serum.
Free T3 in your serum represents the amount of thyroid hormone which has already been activated and is ready for action.
When assessing thyroid hormone function in the body you want to evaluate free T3 and look for levels at least in the top 50% of the reference range.
Lower levels may be a tip-off to a condition known as low T3 syndrome (35).
Total T3
The total T3 represents the amount of T3 that is bound to carrier proteins in the body and is not quite as biologically active as free T3.
Total T3 is very useful in that it tends to be a sensitive and EARLY marker of thyroid dysfunction and can be used to diagnose early thyroid disease:
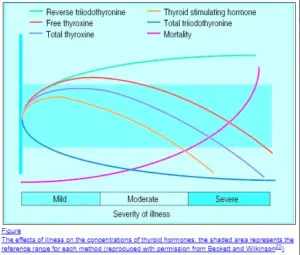
In early thyroid disease, the total T3 drops faster relative to TSH (36).
So while your TSH may remain somewhat “preserved” or “normal” in early thyroid disease, the total T3 will tell the tale.
The difference between Total T3 and reverse T3, which can both be assessed in the serum, may help diagnose those patients who remain symptomatic but have “normal” TSH and free T4 levels.
Total T3 can also be used as a marker to determine how much of the T4 in your body is being converted to the active thyroid hormone.
Thyroid conversion problems may be suspected in cases where patients receive T4-only thyroid medication such as levothyroxine but experience no change in Free T3 or Total T3 levels.
Reverse T3
Reverse T3 is another tool that you can use to help understand what is happening with thyroid conversion in peripheral tissues but also a way to understand metabolic function.
Studies indicate that higher serum levels of reverse T3 may be correlated with a reduction in basal metabolic rate (37) and thus how many calories you burn at rest.
This is very important for those patients who may not have overt hypothyroidism but struggle with the ability to lose weight.
Reverse T3 levels can also be used as an early indicator of thyroid dysfunction and abnormalities tend to occur before changes in TSH and free T4 levels are seen.
Sex Hormone Binding Globulin
Or SHBG for short is a serum marker that can be used as a surrogate marker for thyroid status in the liver.
Remember when we said that there are some blood tests that can help determine if your cells are utilizing thyroid hormone? Well, this is one of those.
The value in testing SHBG is that only 2 hormones are known to increase serum levels and they include T3 (thyroid hormone) and Estradiol.
If you are taking thyroid hormone and your body has no issues converting it then you should notice an INCREASE in sex hormone binding levels, provided estradiol levels stay the same.
Likewise, if you are taking thyroid hormone and your SHBG is NOT changing then it may be an indication to the physician that the type of thyroid hormone you are using may not work for that specific patient.
I have also used SHBG as a way to determine the absorption of thyroid hormone in the GI tract.
Why?
Physiologically speaking the absorption of drugs through the GI tract tends to hit the liver first (due to portal vein circulation).
It’s also well known that certain substances (including low stomach acid) may interfere with thyroid hormone absorption (38) in the GI tract.
SHBG can, therefore, also be used in some cases to help assess thyroid hormone absorption.
Thyroid Antibodies (TPO & TGAb)
The term thyroid antibodies refers to two tests which include Thyroid peroxidase antibody (TPO) and Thyroglobulin antibody (TGAb).
There are more antibodies that alter thyroid function such as thyroid-stimulating immunoglobulin but this usually leads to hyperthyroidism, not hypothyroidism which is the topic of our discussion here.
Why are thyroid antibodies important?
They can help identify the presence of the common autoimmune disease Hashimoto’s thyroiditis.
This condition is characterized by the body attacking its own thyroid gland.
These antibodies are produced by the immune system which then causes damage to the thyroid gland when your body tries to protect itself.
If left unchecked then eventually these antibodies will irreversibly ultimately destroy your thyroid gland and lead to overt hypothyroidism and reliance upon thyroid medication for life.
With this in mind, it seems important to know if this condition is occurring in the body, but this information isn’t always felt to be necessary by some physicians.
Many physicians opt NOT to test for thyroid antibodies with the following logic:
If the TSH is normal then the damage hasn’t reached a critical point and therefore there is nothing to do.
This is known as the “wait and see” approach in treating autoimmune thyroid disease.
That is – wait and see until the damage is done and then treat the hypothyroidism as you would normally.
This logic is employed by many physicians with the idea that the autoimmune component cannot reliably be treated.
But does checking the antibody levels have other benefits outside of thyroid management?
The answer is yes.
The presence of these antibodies does not necessarily mean that you have thyroid disease (they can be elevated in other conditions) but their presence may give you an idea of your future risk for conditions such as infertility and your personal risk of cancer or other autoimmune diseases (39).
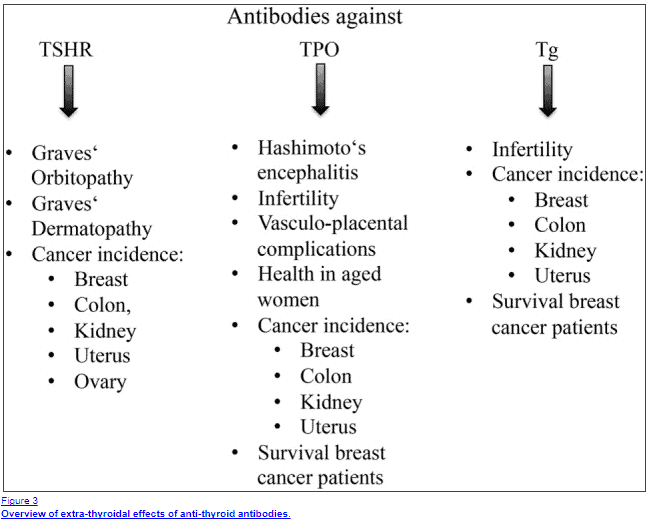
Beyond this correlation, the absolute value of thyroid antibodies may be helpful in determining your risk of developing overt hypothyroidism later in life.
Put another way, checking these antibodies may give you an idea of disease severity (40).
It might make sense that you can use these antibodies as a way to monitor if you are treating Hashimoto’s but studies have failed to show a correlation between absolute values of antibody levels and damage to the thyroid gland (41).
Bottom line?
Assessing the presence of thyroid antibodies should be done to establish a baseline and periodically throughout treatment.
Thyroid Medications
This discussion wouldn’t be complete without also discussing the various thyroid medications available to hypothyroid patients.
These medications differ from one another in very important ways:
Certain medications contain only the inactive thyroid hormone T4.
Other medications contain only the active thyroid hormone T3 and are therefore much more powerful than T4-only medications.
Some medications are created by crushing and desiccating the thyroid glands of animals and encapsulating the remains.
And still, each of these medications differs in the way that they are absorbed and assimilated due to how they are packaged with various fillers and dyes.
Let’s break it down and discuss how to navigate the landscape of thyroid medications and help determine which one is best for your body…
T4-only Thyroid Medications
T4-only thyroid medications are the most commonly prescribed for the treatment of hypothyroidism.
They are the preferred medication among endocrinologists and primary care providers.
T4-only thyroid medications are felt to be the “safest” among thyroid medications because they have the longest half-life (stay in your system the longest) and tend to have few side effects.
In addition, it is preferred because there are many strengths and dosages available and because it’s easy to “monitor” via the serum marker TSH.
When using T4 medications it’s important to realize that in order for the medication to be activated your body must convert the T4 you take into the active T3 form.
The supposition by many physicians is that as long as you provide the T4 that the body will take care of the rest.
This supposition only works in some patients and may explain why up to 15% of patients taking T4 still express the symptoms of hypothyroidism (discussed previously).
List of T4-only thyroid medications:
- Levothyroxine & Synthroid – These medications tend to contain many fillers/dyes which may interfere with absorption in certain patients.
- Tirosint – Tirosint is a “cleaner” version of T4 thyroid medication which contains only 3 inactive ingredients (along with the active T4 hormone). Tirosint may be considered in patients who don’t tolerate Synthroid/levothyroxine.
Who should consider using T4-only thyroid medications?
- Patients who do not have issues with peripheral thyroid conversion – those with normal total T3, free T3 and reverse T3 levels upon testing
- Patients who have never taken thyroid hormone medication before
- Those who may have trouble taking their medication in a consistent manner (at the same time each day)
- Patients who do not tolerate NDT and/or T3-containing medications – those who may experience heart palpitations or anxiety with these medications
While T4-only medications aren’t perfect for everyone they do work great in a large subset of patients.
Patients who do not do well on T4, however, may find an improvement in their symptoms and quality of life when exploring medications that contain the active thyroid hormone T3:
T3-only Thyroid Medications
Medications that contain T3 thyroid hormone are considered to be the most powerful of all thyroid hormone replacement medications.
The reason is simple:
T3 is the ACTIVE thyroid hormone and it exerts the effects of thyroid hormone in the body.
How much more powerful is it compared to T4?
That’s hard to assess directly but we know that T3 is about 3-4x more powerful at influencing (read: suppressing) the TSH when compared to T4.
Some take this to believe that it is 3-4x more powerful than T4 but I don’t believe this can be definitively declared by looking at pituitary function alone.
You also need to consider the cellular competition for binding to thyroid receptors from reverse T3 floating in circulation.
Either way the science is not clear, but what is clear is that T3 is more potent than T4 to some degree.
When considering the use of T3 it’s important to consider normal thyroid physiology in the body.
In other words, how much T3 is the thyroid producing naturally? If we can find that number would it make sense to supplement with that percentage of T3 in addition to T4?
When we look at physiologic studies we know that the thyroid produces both T4 and T3, of this total amount of thyroid hormone produced about 80% is T4 and about 20% is T3 (source)(42).
So while about 20% of total thyroid hormone produced is T3 directly the majority of T3 in circulation (floating around your blood) is produced by the conversion process we discussed previously.
This makes the T4 to T3 conversion process more important than the absolute production of T3 from the thyroid gland.
We can then use this information to potentially help dose patients by mimicking the natural production of thyroid hormone when using thyroid medication.
A ratio of 80:20 (T4:T3) may make sense for certain individuals especially if they are not doing well on T4-only medications alone.
T3 medications can, therefore, be added in low doses to existing T4 medications and can be titrated according to the TSH to prevent negative or adverse effects (43).
Some studies show (44) that patients who add or switch to T3 medications lose weight when they were weight-neutral on T4 medications.
But what about side effects? Is there a reason not to use T3?
T3 is felt to be more difficult to dose partially because of the absorption of this medication and its short half-life.
Put another way – once you ingest T3 your body rapidly absorbs the T3 and serum levels may peak within 2-3 hours (45).
If the dose is too high then T3 may reach excessive levels in the serum and through the non-genomic actions of thyroid hormone on cardiovascular tissue, may lead to symptoms such as heart palpitations.
So while T3 replacement doesn’t work for everyone (and doesn’t necessarily need to be tried as first-line therapy) it still has value in certain patients.
Because many physicians don’t use T3 it’s important that we mention the names of these medications.
T3 comes in 2 basic forms:
- Liothyronine & Cytomel – This is considered an immediate-release version of T3 in which serum levels peak around 2-3 hours after ingestion. T3 can be added in small doses (ranging from 5-20mcg) to existing doses of T4 (like Levothyroxine).
- Sustained release (compounded) T3 – This formulation of T3 is compounded in such a way as to slow down the absorption of T3 in the intestinal tract. You might consider using SR T3 if you experience heart palpitations or other issues with IR T3.
Who should consider using T3 thyroid medication?
- Patients who have failed to improve on T4 only thyroid medications such as Levothyroxine, Synthroid, and Tirosint
- Patients with known or suspected problems with T4 to T3 conversion
- Patients with euthyroid sick syndrome, Low T3 syndrome, or elevated serum levels of reverse T3
- Those who don’t tolerate or who have failed treatment with natural desiccated thyroid medication
Natural Desiccated Thyroid
Another form of thyroid medication includes all medications labeled under the name of Natural Desiccated Thyroid, sometimes referred to as NDT for short.
These medications are formulated by encapsulating the actual hormone glands of animals (porcine in this case).
By crushing and desiccating the thyroid gland in these animals you are actually ingesting active thyroid hormones which come from the animal itself.
It may sound weird or odd but this type of medication was the main form of thyroid replacement in the past (as the main form of therapy in the 1900s) and many activists currently suggest it may be the most superior form of thyroid replacement.
While NDT certainly has its place in the treatment of hypothyroidism it is not necessarily the perfect medication (for reasons stated below).
There are several types of natural desiccated thyroid medications (or NDT for short) which we will discuss below.
But first:
Is there some benefit to using thyroid hormones from animals over the synthetic versions of T4 and T3 we discussed previously?
One of the potential benefits of using NDT is that it contains both the active and inactive forms of thyroid hormone which can be helpful to many patients.
In addition, NDT also contains several other hormones including T1 and T2 (46)(other but biologically less active forms of thyroid hormone) and other enzymes/hormone precursors.
It’s possible that the ingestion of these other hormones may augment existing thyroid function in certain patients but this has not been well studied.
It would be silly to assume that just because T1 and T2 are much less biologically active than T3 and T4, they are therefore useless – they obviously serve a purpose, but we don’t completely understand this purpose quite yet.
The disadvantages of using NDT include the static nature of the dosing of both T4 and T3 in individual doses.
NDT contains about 38mcg of T4 and 9mcg of T3 in 1 grain (usually translated to 60-65mg).
The problem with static dosing is that you lose the ability to individually titrate T4 and T3 because the ratio is “set in stone” so to speak.
Another potential disadvantage to using NDT is that you are consuming animal products and the ingestion of foreign material (and hormones) may actually be antigenic to some individuals.
This “antigenic” material may set off the immune system and lead to an exacerbation of autoimmune thyroiditis (Hashimoto’s) or simply lead to the premature destruction or inactivation of the hormone after ingestion.
These problems mean that not all patients will do well on NDT – just like the other thyroid medications listed above.
Instead of trying to find the “best” thyroid medication you should instead search for a medication that compliments your body and the “natural” state of thyroid function that your body is used to.
Let’s discuss the various formulations of NDT:
- Armour Thyroid – Armour Thyroid is a popular NDT medication but may contain some inactive ingredients that lead to absorption issues in certain individuals.
- Naturethroid – Differs in dosage from Armour Thyroid in that 1 grain is 65mg vs the 60mg of Armour Thyroid. Tends to be well tolerated among NDT medications.
- WP Thyroid – WP thyroid contains the fewest inactive ingredients and may be better tolerated in individuals with GI-related issues.
Who should consider using natural desiccated thyroid hormone?
- Patients who have not done well on T4-only thyroid medications
- Patients who do not do well on T3 medications such as liothyronine or cytomel
- Patients with known or suspected peripheral T4 to T3 conversion issues
- Patients with low serum total T3 and/or low free T3
- Patients may consider switching to NDT if they notice some improvement on other medications but want to trial other formulations and medications
Does Everyone Need to Take Thyroid Medication?
The answer is even though you may have some thyroid dysfunction in the body doesn’t necessarily or automatically mean that you need to take thyroid hormone.
Remember that we described thyroid function as a spectrum in the body.
Certainly, some people will be reliant upon medications such as those who suffer end-stage thyroid gland atrophy from chronic Hashimoto’s disease or those post-thyroidectomy, but this isn’t true for all patients.
Some patients may experience slight thyroid dysfunction from various factors which may be reversible.
Some of these conditions include environmental factors such as minor nutrient deficiencies (iodine being one)(47), exposure to endocrine disruptors, exposure to chronic stress (48), and even being overweight.
In cases where thyroid dysfunction is NOT primary – meaning that thyroid dysfunction is the result of some other condition, there may be hope for returning thyroid function to its natural state.
The treatment for such conditions would be to address and reverse these conditions on a case-by-case basis.
Repleting nutrients, avoiding endocrine disruptors, managing your stress, and even weight loss may lead to a natural improvement in thyroid function and these steps should not be ignored.
Furthermore, these factors may also compound existing thyroid disease and make thyroid function worse.
In cases such as these, it’s always important to address and treat those problems that you are capable of influencing.
Because it may be difficult to ascertain the exact cause of thyroid dysfunction in your body it may make more sense to simply address these issues on your own.
One such option is using therapeutic and pharmaceutical-grade supplements to help in the management of your symptoms.
Supplementing for Your Thyroid
Hypothyroidism is unique among hormone imbalances in that it can directly or indirectly lead to nutrient deficiencies due to poor GI absorption.
It is well known that in order for optimal absorption of nutrients the stomach must be at a certain pH.
A deficiency in thyroid hormone may lead to states of reduced stomach acid which may, therefore, alter the absorption of medications, nutrients, and even macromolecules.
If this were true wouldn’t we expect to see certain nutrient deficiencies in hypothyroid patients?
Absolutely and that’s exactly what we see.
Studies have shown that up to 30% of hypothyroid patients (49) may suffer from sub-optimal serum levels of Vitamin B12.
Other studies (50) indicate that there is a bidirectional relationship between iron deficiency and hypothyroidism (especially autoimmune thyroid disease).
Still, more studies suggest (51) there is a link between low vitamin D levels and the development of hypothyroidism.
More studies show (52) that thyroid hormone is required for optimal absorption of other trace nutrients such as Zinc, Selenium, and Copper.
It’s clear that there is an important relationship between the absorption of these nutrients and thyroid hormones in the body.
What is less clear is how important the supplementation of these nutrients is in reducing the symptoms associated with thyroid disease.
This seems to be dependent upon the individual and their responsiveness to certain supplements.
Because of the importance of these nutrients in thyroid function, it’s important to address certain nutrients (especially those listed here) if you suffer from hypothyroidism.
The reason is simple:
The co-existing presence of Vitamin B12 deficiency may lead to confusing symptoms such as low energy or a decrease in cognition which may not be eliminated with the replacement of thyroid hormone.
Supplementing with B12 will be required (in this hypothetical case) for complete improvement in symptoms.
This logic extends to other nutrients, especially in the case of hair loss which can be caused by hypothyroidism but also by low iron and/or zinc deficiency.
You can learn more about supplementing and which supplements I recommend hypothyroid patients take in this guide.
Wrapping it Up
I hope you will agree that the treatment of hypothyroidism should be individualized and tailored to each specific person.
Because of the complexities involved in assessing and managing thyroid status in the body, it’s important for each patient to have a broad and even deep understanding of everything related to thyroid hormone ranging from medication replacement to physiology.
This kind of information and education will serve you well and help you become an advocate for your own health for years to come!
When it comes to your life there is nothing more important than your health or your quality of life.
With this in mind, I recommend that you actively seek out competent and willing physicians to help you along your journey.
It may take some searching but it will be worth it in the end.
Over the coming decades, I suspect that the way we look at thyroid hormone (and many other diseases!) will dramatically change as advanced genetic tests are developed which allow physicians to tailor hormones and medications to each patient.
This kind of technology may be years away but you can still piece it together with the help of a competent physician!
Now I want to hear from you:
Please share your thyroid story below!
I want to hear about your experience in finding out how to improve your health, the pitfalls you’ve gone through, and what it took to finally start feeling better.
If you haven’t reached that point yet please share your experience and tell us why you think that is!
You’d be surprised that so many patients find comfort in the comment section in knowing that other patients may be dealing with the same problems that they are.
Leave your comments below!
Scientific References
#1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3433956/
#2. https://www.ncbi.nlm.nih.gov/books/NBK285561/
#3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907936/
#4. https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072785/
#5. https://www.ncbi.nlm.nih.gov/books/NBK221535/
#6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3271310/
#7. https://www.ncbi.nlm.nih.gov/books/NBK459262/
#8. https://www.ncbi.nlm.nih.gov/pubmed/19540303
#9. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(74)92070-4/abstract
#10. https://www.ncbi.nlm.nih.gov/pubmed/20578900
#11. https://www.ncbi.nlm.nih.gov/pubmed/12055988
#12. https://www.ncbi.nlm.nih.gov/pubmed/19594417
#13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3219766/
#14. https://www.ncbi.nlm.nih.gov/pubmed/17970771
#15. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3743364/
#16. https://www.ncbi.nlm.nih.gov/books/NBK221535/
#17. https://www.ncbi.nlm.nih.gov/pubmed/28982017
#18. https://www.ncbi.nlm.nih.gov/pubmed/22484490
#19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3821486/
#20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017747/
#21. https://www.ncbi.nlm.nih.gov/pubmed/21532331
#22. https://www.ncbi.nlm.nih.gov/pubmed/8808101
#23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3219173/
#24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4980994/
#25. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4980994/
#26. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4980994/
#27. https://www.ncbi.nlm.nih.gov/pubmed/19190113/
#28. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3271310/
#29. https://www.ncbi.nlm.nih.gov/pubmed/20578900
#30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2174406/
#31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3169863/
#32. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1578599/
#33. https://www.ncbi.nlm.nih.gov/pubmed/3428867
#34. https://www.ncbi.nlm.nih.gov/pubmed/12055988
#35. https://www.ncbi.nlm.nih.gov/pubmed/16840838
#36. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1127319/
#37. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3608008/
#38. https://www.ncbi.nlm.nih.gov/pubmed/28153426
#39. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5422478/
#40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5422478/
#41. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5422478/
#42. https://www.ncbi.nlm.nih.gov/pubmed/12915350
#43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3205882/
#44. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3205882/
#45. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5167556/
#46. https://www.ncbi.nlm.nih.gov/pubmed/24602963
#47. https://www.ncbi.nlm.nih.gov/pubmed/16131334
#48. https://www.ncbi.nlm.nih.gov/pubmed/19913515
#49. https://www.ncbi.nlm.nih.gov/pubmed/16969140
#50. https://www.ncbi.nlm.nih.gov/pubmed/28202844
#51. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3921055/
#52. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746228/