If you’ve been on my website before, or if you’ve read my blog, then you know that one of my major goals is to try and change how doctors think about treating thyroid-related issues.
My personal belief is that patients do not benefit from the archaic treatment paradigm which focuses solely on TSH.
Today I want to dig into that topic a little bit further and talk about how doctors look at TSH, what it actually means, and why we treat the thyroid differently from all other hormone systems in the body.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Thyroid Testing and the TSH
As you probably know, doctors tend to look solely at the TSH when they are determining how your thyroid is functioning (1).
This isn’t necessarily a problem by itself, but it should cause some alarm bells to go off once people start realizing that this treatment doesn’t always deliver the results people are looking for.
What do I mean?
When I first started training I found out fairly quickly that thyroid patients tend to be very difficult to treat.
From a conventional standpoint, they don’t ever seem to get better! (Obviously, this isn’t true knowing what I know now, but in the beginning, this is how I felt).
They would come into my office complaining of fatigue or just not feeling like themselves and I would quickly diagnose them with hypothyroidism when their TSH came back as “high”.
The only problem?
The symptoms wouldn’t go away once they were “treated” and their TSH was lowered back to normal.
This didn’t sit well with me from a logical standpoint.
I knew that fatigue was one of the major side effects of hypothyroidism, so wouldn’t it make sense that this fatigue should resolve once the main problem was treated?
It’s always possible that their fatigue could be from some other cause, but I started to second guess my personal bias in regards to treatment when I saw this trend happening over and over.
It caused me to reflect on the TSH as a marker of thyroid function and compare that to how we look at other hormone systems in the body (by we I am referring to doctors).
And I realized that we treat the thyroid differently than other hormone systems in the body.
In fact, it’s almost unfair in a way because we look at thyroid function differently than we do cortisol, estrogen, progesterone, and testosterone even though ALL of these hormones are regulated in a similar way to your thyroid.
It’s actually very easy to understand so let me explain.
This is how it works:
Your pituitary produces pro-hormones which then go act on different organs in your body and cause the release of specific hormones.
For the thyroid, your body produces TSH (thyroid stimulating hormone) which stimulates your thyroid gland (the organ) to produce thyroid hormone.
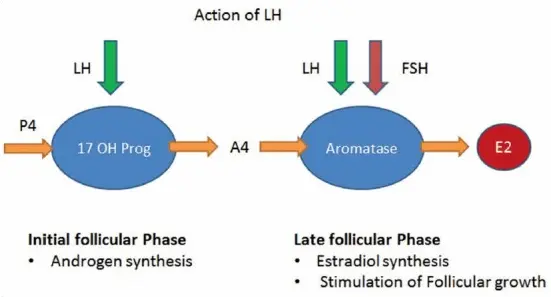
For estrogen and progesterone, your body produces FSH (follicle stimulating hormone) and LH (luteinizing hormone) which act on your ovaries (the organ) to produce estrogen and progesterone (2).
For cortisol, your body produces ACTH (3) (adrenocorticotropic hormone) which acts on your adrenal glands (the organ) to produce cortisol.
Do you see the pattern here?
Almost all of these hormone systems work in a VERY similar way.
They all are influenced by the pituitary gland and result in the release of very important hormones.
It would make sense then that we would evaluate each hormone system for problems in the same way.
But we don’t.
When it comes to your thyroid gland, we look directly at this TSH number and use that number as a way to estimate how well the gland is functioning.

For ALL other hormone systems here we nearly completely disregard the pituitary equivalent pro-hormone and instead look directly at the absolute concentration of hormones in the body.
This may not sound like a big deal, but it can have profound consequences.
For instance:
By looking at the TSH as a marker of thyroid function we are making the assumption that whatever outside forces we use to “alter” this number (usually thyroid medications) results in the same physiologic consequences as whatever your body does when it is producing thyroid hormone normally.
But how can we make that assumption when no other hormone system works that way?
When doctors give patients insulin they don’t give patients the exact amount of insulin that the pancreas produces normally. They alter the required amount of insulin based on the NEEDS of the patient (4).
And that’s what I propose we do for thyroid patients, even though we currently don’t.
Let’s take a look at other hormone systems to give you a better idea.
Let’s Look at Birth Control Pills
Birth control pills are probably the worst offender.
These pills contain synthetic hormones which are designed to completely shut down the normal function of estrogen and progesterone.
They do this by completely suppressing FSH and LH in your body (5), which are your pituitary pro-hormones.
FSH and LH can be compared to TSH because they all cause the release of their specific hormone from their target organ.
As you know, it’s a big no-no to suppress the TSH if you are treating with thyroid medication, but this is completely ignored if you are taking birth control pills!
In fact, if you tested any patient taking birth control pills you would find that both their FSH and LH are likely suppressed down to an undetectable level.
If we treated birth control pills like we do thyroid hormone then doctors would start with a small dose of birth control and then titrate the dose based on the FSH and LH.
Would it surprise you to know that doctors rarely even check the FSH and LH once they start taking birth control pills?
Do you know how they know if they are working or not?
They usually look at a clinical symptom which is the absence of the menstrual cycle as an indicator that the dose is just right.
If you aren’t having your cycle then the medication is “working”.
When we apply this same concept to people on thyroid medication, that is that we increase their dose until their symptoms disappear it is considered malpractice.
Doctors will tell you that the reason we don’t suppress TSH is that it can lead to negative consequences.
But the only consequences they cite are bone loss (6) and risk of atrial fibrillation (7).
I’ve already written about how the science isn’t settled in that lowering the TSH definitely results in these conditions and you can read more about this idea here if you’d like.
And if we are using the same logic, we might ask ourselves, “does suppressing the FSH and LH with birth control pills also cause any problems”.
And the answer is most likely, yes.
Newer studies are showing that using birth control pills may increase your risk of certain types of breast cancer (8).
In addition, there are probably other consequences that should be considered such as weight gain and consequences from excess synthetic estrogen.
The thyroid system is somewhat different from the estrogen/progesterone system in that all medications used to treat thyroid conditions are considered “bio-identical” or exact replicas of the same hormone that a normal healthy body produces.
None of our current iterations of birth control pills are considered bio-identical, in fact, they are all slightly manipulated synthetic versions of estrogen or progesterone.
This means that we can’t compare both therapies and consequences, but it’s still a very interesting exercise to look at both of them together.
And, by the way, when women go off of the pill they also tend to experience a rebound rise in FSH and LH (9) which is similar to what thyroid patients experience when they stop taking thyroid medication.
Let’s Look at Steroids
Next on the list are steroids.
And by steroids, I am referring to cortisol.
Cortisol is perhaps more closely related to thyroid hormone when compared to estrogen and progesterone simply because both cortisol and thyroid hormones are required to sustain life.
Having incredibly low levels of both cortisol and thyroid hormone in your body may lead to death.
So you can imagine that doctors take low cortisol very seriously and rarely ever prescribe cortisol unless it is absolutely necessary.
But do you know how doctors test for low cortisol?
They look directly at your serum cortisol level (first thing in the morning).
If both the thyroid and cortisol systems were the same then we would determine if you have enough cortisol by looking at your ACTH level and then prescribe the dose of hydrocortisone based on that.
But that’s not what we do at all.
In fact, it’s the exact opposite.
Doctors know that prescribing even SMALL doses of steroids results in complete suppression of the ACTH (10).
And, as you might imagine, the ACTH plays a minimal role in helping to determine the dose needed.
But, unlike estrogen and progesterone, doctors do care a little bit more about the ACTH because it impacts how long it takes for a patient to recover.
The longer you take steroids (synthetic or hydrocortisone) the more suppressed your ACTH will become and the longer it takes for it to recover after you stop taking your medication.
For this reason, doctors never let people who have been on steroids for longer than 1 month stop taking their steroids cold turkey.
Instead, they prescribe a “taper” dose which allows them to lower their dose slowly over time.
This gives their body (and HPA system) time to recover.
This same phenomenon occurs when you start taking thyroid hormone as well, but your thyroid system seems to recover faster than your cortisol system.
So, despite the similarities between your thyroid system and your cortisol system, they are both treated completely differently.
Let’s Look at Testosterone
Next on the list is testosterone.
And for this section, I’m going to focus mainly on men, even though the same logic applies to women.
When a man goes into the doctor’s office to test his testosterone level how do you think it’s done?
It’s done by testing DIRECTLY for serum testosterone levels (both free and total testosterone).
It’s NOT done by testing for the LH or FSH (which would be the same logic used when testing your thyroid).
In addition, once a man is being treated for low testosterone his dose is titrated based on the absolute concentration of testosterone in his blood, not the LH or FSH.
If we applied this logic to your thyroid then we would care a lot more about your absolute thyroid hormone concentration (which can be tested by looking at free t3, and free T4, by the way) and a lot less about your pituitary pro-hormone TSH.
And, much like estrogen and progesterone therapy, the FSH and LH in men taking testosterone are extremely suppressed.
In fact, even low to moderate doses are enough to shut down the HPA system and reduce FSH and LH to undetectable levels.
It appears that while the pituitary system is great for managing your sex hormones, thyroid, and cortisol on its own, it’s exquisitely sensitive to outside forces or hormones.
We can and should use this information when we look at your thyroid.
Do your Free T3 and Free T4 Have Value?
The question is:
Why do doctors not care about free thyroid hormone levels and instead focus on TSH?
The answer is that they don’t believe that free T3 and free T4 have any value.
And that’s a big problem because there is emerging evidence to suggest the exact opposite.
For instance:
#1. Newer studies (from 2017) have shown that free thyroid hormones are a better predictor of weight loss when compared to TSH (11).
People who have higher free T3 and total T3 levels tend to lose more weight than those people with low free T3/total T3.
This is a problem when you realize that doctors don’t care what your free T3 is so long as your TSH is fine, but it’s very possible for you to have both a low free T3/total T3 and a “normal” TSH.
If the TSH is the best measurement of thyroid function then why doesn’t the TSH track with weight loss when compared to free thyroid hormone levels?
The answer is because it’s not the best marker.
#2. In addition, there are genetic variants that are now documented and known which alter how well a person can metabolize or break down thyroid hormone.
Certain individuals, no matter how much thyroid medication they take, will NEVER be able to produce enough T3 thyroid hormone on medications like Synthroid if they have this genetic variant (12).
How can you compare someone with this genetic variation to someone who doesn’t have it?
You can’t, and the only way to know if someone has it is by testing free T3 and total T3.
And, by the way, there are plenty of other genetic variations which influence how your body responds to thyroid medication.
In the near future, we should be able to run your genetics to determine how well you might respond to the various types of thyroid hormone medications.
#3. If that wasn’t enough, we also know that there are endocrine-disrupting chemicals that can influence free thyroid hormone levels without altering the TSH.
Certain chemicals, which you and I come into contact with on a daily basis, have been shown to interfere with normal thyroid hormone processing at the cellular level (13).
These chemicals look similar enough to thyroid hormone that they are able to sit on your thyroid hormone receptors.
This is a problem because then your normal thyroid hormones can’t activate cellular receptors because they are blocked.
And the only way for thyroid hormone to work is to hook onto these receptors and activate the cells.
You can imagine, then, that as these receptors are blocked your body will be in a state of relative hypothyroidism (depending on which cells are blocked) even though your blood tests are “normal”.
The only way to find out if this problem is occurring is by evaluating free thyroid hormone levels.
These are just a handful of documented reasons which should give physicians who use the TSH as a marker of thyroid function pause.
And, as a patient, you should also be aware of these because it will help you understand if your doctor is up to date with current literature or not.
If you are working with a doctor that doesn’t recognize these factors (for whatever reason), then you may want to seek out a second opinion from someone who is more up-to-date.
Surprisingly (or not), you will find that many doctors are behind new research by an average of 17 years or more (14), so it may take some work on your part to find those doctors who are actively reading new research.
Is Suppressing your TSH Dangerous?
I know that it may seem like I am advocating for the complete disregard of the TSH in favor of looking directly at your free thyroid hormones but that’s not my stance or my opinion.
Instead, my idea is that we should use a combination of lab tests to help us better understand what is going on with thyroid function in thyroid patients.
There are so many thyroid patients out there who are suffering from symptoms related to low thyroid function despite taking “adequate” amounts of thyroid hormone.
Doesn’t it make sense that we re-evaluate our current treatment paradigm to see if we missed anything?
I think TSH is an important measure of thyroid function, but it simply doesn’t give a clear picture of what is happening with the thyroid system.
How can it, when there are so many other factors at play?
Instead of focusing solely on the TSH, we should look at the TSH in conjunction with free T3 levels and free T4 levels.
While doing this, we should put preference on optimizing these free thyroid hormone levels even if it means slightly lowering or suppressing the TSH.
We should, however, not blatantly disregard the TSH and ignore it completely.
The TSH certainly has value and can help us understand how a patient responds to thyroid hormone and how high or low their dose may need to be.
Conclusion
Doctors place a huge emphasis on TSH when they evaluate thyroid function.
Even though the TSH can be useful, it may not be the best or most appropriate tool for diagnosing and managing thyroid problems.
If you are someone who is struggling with persistent hypothyroid symptoms DESPITE taking ‘adequate’ thyroid medications, then you may be someone who needs more advanced testing.
Not everyone will fit into this category, however, as some people may be perfectly fine when looking at the TSH.
But if problems arise during your treatment then the next step should be to look at your free thyroid hormone levels.
Now I want to hear from you:
Are you someone who is feeling poorly despite taking thyroid medication?
Do you have a normal TSH but still remain symptomatic?
Have you had your free thyroid hormone levels tested?
Leave your questions or comments below!