Weight gain, crushing fatigue, the inability to sleep…
These are only some of the symptoms associated with adrenal problems and yet this condition is ignored by so many physicians and Doctors.
In addition, there is much confusion regarding which is the best way to actually evaluate your cortisol levels and which is the best cortisol test.
This post will walk you through why testing your cortisol level is important, how to determine if you need testing, the best way to actually test your cortisol, and how to treat yourself once you find out.
Let’s dive in:
What is Cortisol & Why do we care about your levels so much?
Cortisol is a hormone involved in many different functions in the body (many we will go over today).
The problem with this hormone is two-fold:
First:
High levels of cortisol cause problems by themselves and may lead to the signs and symptoms of adrenal fatigue.
Second:
Dysregulation of cortisol levels also may cause problems with other hormones (1) in your body leading to weight gain, difficulty with concentration, and many other symptoms.

This gives you more than just 1 good reason to not only understand your cortisol levels but to treat them if necessary.
The problem with cortisol testing today
This problem extends beyond what we’ve already discussed.
Like other hormones in the body (think thyroid, testosterone, estrogen, progesterone, etc.) doctors and physicians don’t have a really good understanding of what these hormones do, how to test for them and how to treat them.
This leads to a lot of confusion – especially on the side of the patient, and frustration on the side of the physician.
This problem may explain why so many patients step out on their own to ask for tests or purchase their own cortisol tests.
To add to the confusion there are many different ways to actually test for cortisol levels (some certainly better than others) that may give conflicting or confusing results.
To complicate problems further most physicians don’t know how to interpret or understand cortisol testing which leaves patients on their own for treatment and management.
Sound confusing?
It can be, but let’s shed some light:
What defines normal cortisol vs high cortisol vs low cortisol
Part of the problem with understanding changes in cortisol levels stems from a lack of consistency and branding/naming conditions.
Most doctors are intimately familiar with the conditions known as Addison’s disease and Cushing’s disease.
These conditions range from zero cortisol to extremely high levels of cortisol (both outside of the reference range that doctors love):
Addison’s disease is basically a complete lack of cortisol in the body due to autoimmune (or other damage) resulting in almost zero cortisol – this is a life-threatening condition and requires cortisol or steroid replacement.
On the other hand, Cushing’s disease is a syndrome that causes an incredible amount of cortisol in the body leading to many serious and potentially life-threatening conditions.
When you talk to your doctor about your cortisol levels they are going to be looking at your cortisol levels with these conditions in mind.
When they check your cortisol and find that you are decidedly in the “normal” range you will be branded as completely normal and fine.
But does this make sense?
Surely there are conditions in between the two extremes of absolutely zero cortisol and total excess of cortisol in the body, right?
Of course – just like other hormones can become dysregulated and sub-optimal, so too can cortisol.
Like other hormones in the body, small changes to concentrations of these hormones can lead to big symptoms that are felt throughout the body.
Symptoms that fall in this range are frequently lumped into the category of “adrenal fatigue” and that’s what we are going to be discussing in this post today:
The difference between “normal” and “optimal” levels of cortisol.
We will not be focusing on Addisonian or Cushingoid levels of cortisol, but instead, we will focus on the mid and “gray” range of cortisol testing.
Testing for Cortisol levels
So how do you find out if your cortisol tests are abnormal?
Surely, some tests are better than others for determining this…
There are several ways to test for cortisol in your body but I’m only going to focus on the best ways.
The first place to start is always with your serum (blood levels).
I know what you’re thinking…
Serum levels of cortisol are the worst! They don’t tell you anything!
That’s generally true if you have cortisol receptor issues, but these levels can be very useful to start with because they are easy to get and much cheaper than the alternative forms of testing (which we will detail below).
Serum cortisol levels are especially helpful if they are low normal or high normal, but not much if they are simply “normal”.
What defines low normal and high normal?
- Low normal cortisol range: 8 am Serum cortisol levels ranging from 4.0 to 10.0
- Normal cortisol range: 8 am Serum cortisol levels range from 11-18
- High normal cortisol range: 8 am Serum cortisol levels greater than 20
You can see an example of a low-normal patient below:

In this example, the 8 am serum cortisol level is 6.5 with a range of 4.0-22.0.
Obviously, this is in the “normal” range, but certainly, it is suboptimal when you consider that cortisol levels should peak at 8 am (2).
This peak should represent the highest your cortisol levels should be throughout the day and low levels are often consistent with symptoms of fatigue.
As mentioned previously serum testing is really only useful if your cortisol levels are either high normal or low normal, they are largely unhelpful if your cortisol level is in the standard “normal” range.
In addition to this, serum levels change at least 8 times throughout the day and may peak due to various substances (like caffeine) or changes to stress.
For this reason, serum levels are not often considered the “best” test, but they are certainly an easy test and the first place you should start.
But what is the best test?
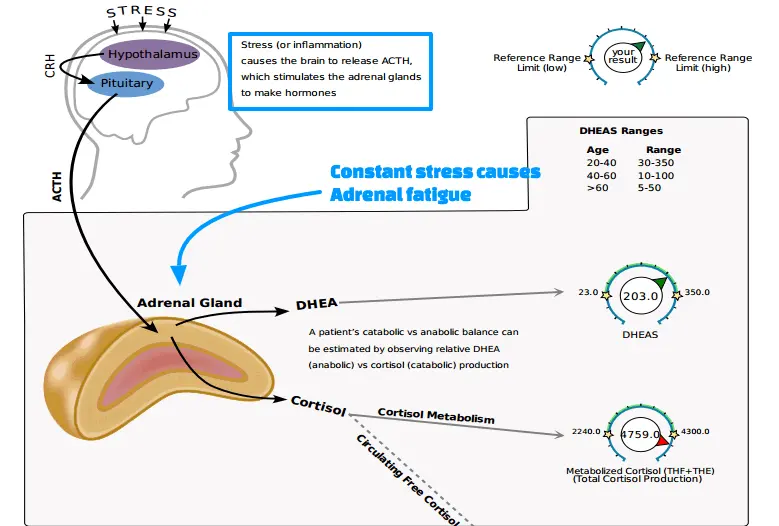
Testing your Cortisol pattern with DUTCH
In order to get a full evaluation of your cortisol levels, it may be necessary to evaluate the “rhythm” of your cortisol throughout the day.
By checking your cortisol several times per day you can accurately see how your body is responding to various situations.
This allows for more detailed information which can then be used for treatment.
The most accurate form of testing is through urinary measurements which are taken several times throughout the day (compared to a 24-hour urine test).
This is even more accurate than salivary levels.
You can learn more about DUTCH testing in the video below or at this link.
You can see an example of my test, taken several times throughout the day which tracks both urinary cortisone and urinary cortisol levels.
You can see the benefit you get from this evaluation because my 8 am serum cortisol levels were in the “normal” range, and yet in this example, you can see that my 10 am cortisol levels spike very high.
This pattern that you see above is seen in people who are reliant upon stimulants for energy each morning (as I was at the time).
Does this mean that everyone needs their urinary cortisol levels tested?
No.
Instead, start with your serum 8 am cortisol levels to see what kind of information you can get, and then move to the DUTCH test if necessary.
It’s also worth a trial of treatment if you are simply symptomatic with “normal” cortisol levels, because even though these tests are helpful there is no test that is 100% accurate.
Many patients stand to benefit from treatment due to the other benefits that adrenal adaptogens and adrenal glandulars provide.
Symptoms of Adrenal problems
The problem with many hormone imbalances is that they tend to share many of the same symptoms as one another.
For this reason (and to ensure proper treatment) it is usually wise to test prior to any treatment you undergo.
Having said that, the value of assessing your symptoms is also very helpful because it gives you a starting point prior to treatment.
Because of this, it’s a good idea to understand some of the symptoms you may be experiencing if you have adrenal-related problems.
Common symptoms of cortisol dysregulation:
- Constant fatigue throughout the day classically with a 2-3 pm “crash”
- The sensation of being “wired but tired”, especially at night
- The feeling of getting a “second wind” at night, especially around 9-10 pm
- Weight gain and/or weight loss resistance
- Other hormonal problems in the body, especially hypothyroidism
- Changes in mood including depression, anxiety, and/or irritability
- Intense carbohydrate or sugar cravings
- Reliance upon stimulants (like caffeine) with frequent use throughout the day for “energy”
- The sensation of more energy after eating a carbohydrate-rich (or sugar-rich) meal
- Cravings for salty foods
This isn’t an exhaustive list but it really hits the highlights that many patients with adrenal problems experience.
You can see that some of these symptoms are highly specific and you will relate to them if you’ve ever experienced them before.
Classically these symptoms build up over time and continue to get worse and worse unless treatment occurs.
But why do patients experience them?
A huge part of this problem has to do with constant everyday stress.
As you may know, cortisol is a stress hormone that your body releases when it’s under some influence that it perceives as stress.
The problem is not that this response is necessary, but the fact that this response tends to get triggered day in and day out.
“Stressors” to the body may include any or all of the following:
- Frustration or changes in emotion from job/work/social life
- Over-exercising or exercising too much for what your body can tolerate
- Anything physically stressful on the body(including exercise, manual labor, etc.)
- Lack of sleep(especially if prolonged over months to years)
- Pressure from school work/workload/etc.
- Poor diet or nutritional deficiencies(especially diets lacking in fruits and vegetables)
- Constant use of stimulants like caffeine(energy drinks, coffee, soda, etc.)
- Complete lack of exercise or a sedentary lifestyle
- Known chronic medical conditions(high blood pressure, insulin resistance, metabolic syndrome, cholesterol problems, etc.)
- Recent illness or sickness
- And anything else that may cause you frustration, annoyance, or “stress”
This is not an exhaustive list, but it’s easy to see how these little things from day-to-day activities stack up over time.
Each time your body undergoes one of these stressors your body will instinctively release cortisol as a way to “cope” with this stress.
The cortisol allows your body to deal with stress by liberating sugar stores and increasing epinephrine and adrenaline.
This is what you want to have happened, and this isn’t necessarily the problem.
The problem comes when this system is constantly activated day after day.
This causes hormonal changes like an increase in insulin resistance, changes to your autonomic nervous system, weight gain, and all of the other symptoms we mentioned above.
This constellation of symptoms has been documented in business executives (3) and even in the military after deployments and other stressful situations.
The point is this:
As humans, we weren’t meant to experience this constant level of stress day in and day out and it really leaves a toll on the body that is actually measurable.
The problem isn’t in diagnosing the disease (that’s actually the easy part) but in getting the proper treatment from conventional doctors.
It’s not also uncommon for kids (children) to experience these symptoms, the only difference is that they tend to respond differently than adults.
Children may have changes in their behaviors, extreme fatigue, and poor grades.
One of the best ways to catch this condition in children is by checking reverse T3 levels which will usually be elevated in children under extreme stress.
Treatment based on your test results:
Treatment for adrenal-related issues is actually quite complex but can be simplified.
Treatment should be based on a combination of your symptoms plus your lab results.
For instance:
Even though high normal cortisol levels and low cortisol levels may present with similar symptoms the treatment of both may vary.
For this reason, it is helpful to understand your levels.
Herbs and supplements that INCREASE cortisol levels wouldn’t necessarily be helpful if your levels were already elevated.
Make sense?
With that in mind let’s talk about how to evaluate and treat these conditions.
For the purpose of this article, we will focus primarily on herbal and adaptogenic intervention but realize that lifestyle changes are ALWAYS required for optimal results.
Treatment for low cortisol
With low cortisol levels, you will want to focus on supplements and herbs that are designed to provide your body with the precursors necessary for the production and creation of cortisol.
Cortisol is a hormone, much like other hormones in the body, that requires several different nutrients to function properly.
With that in mind there are several that can help the cortisol in your body function more efficiently:
- Adrenal glandulars: These tend to work best for patients with very low cortisol levels, they also tend to provide an immediate boost to energy levels. Using glandulars in combination with other supplements listed below is very effective for low cortisol levels. Should be used for 6 + months.
- Adrenal adaptogens: Adaptogens can actually help to lower cortisol levels as well (4), but should at least be considered in the treatment. There are many types of adaptogens but I find that blends of multiple adaptogens tend to work best. These adaptogens can be combined with glandulars as well for more benefit. Should be used for 3+ months at least.
- CoQ10: This coenzyme is involved in proper mitochondrial energy production (5) and can help increase energy levels. Because energy levels are often low in adrenal-related issues, mitochondrial boosters are particularly effective. Use 2 capsules (240mg) per day for several months.
- Alpha Lipoic acid: ALA helps increase mitochondrial energy production, and acts as a powerful antioxidant and an anti-inflammatory agent (6). ALA can also help with weight loss due to its effects on insulin.
- Vitamin B6: Vitamin B6 is used in several pathways in the creation of adrenal hormones and is a nutrient that many patients are deficient in (7). Taking higher doses of B6 during the acute phase of treatment may be necessary for short periods of time.
- DHEA: DHEA is the precursor to testosterone and other estrogen metabolites. With low cortisol and low adrenal hormone production, supplementing with hormone precursors may be of benefit. Start with a low dose every 2-3 days and increase to daily as tolerated. Be careful because DHEA can turn into androgens or estrogens (8) in high doses.
- Pregnenolone: Pregnenolone is another hormone precursor and can be helpful (9) if used along with DHEA. Watch out for acne as a side effect and like DHEA, start low and go slow. The use of these hormones may be necessary for 3+ months.
Taking 3+ of the supplements listed above may be necessary for a minimum of 6 months in order to see continued results and an increase in cortisol levels.
Most patients experience an improvement in their symptoms within 4 weeks of treatment.
Be careful when using DHEA and/or pregnenolone as these are actual hormones that have influence and make changes in the body.
Treatment for high cortisol
- Phosphatidylserine: Phosphatidylserine has been shown to reduce cortisol levels (10) if taken in doses up to 600mg per day. Use 4-6 capsules at night (each capsule is 100mg) and recheck cortisol levels in 2-3 months.
- Ashwagandha: Ashwagandha is an adaptogen that can actually help to lower cortisol levels, boost libido, and may help with weight loss. You can read more about ashwagandha in this comprehensive post.
- Melatonin: Melatonin has been shown to reduce cortisol levels (11) and may actually help improve your sleep at night. Even if you are sleeping well, melatonin can still help reduce cortisol levels and should be considered. Dosages vary from 1-3mg, but starting with 3mg is generally tolerated unless you are very sensitive.
Because fewer supplements lower cortisol, it’s helpful to use several supplements listed above and combine them with the lifestyle changes listed below.
Lifestyle interventions
Lifestyle changes create the backbone of treating adrenal problems and should not be ignored.
Most people have problems in at least 2 of the areas listed below, make sure you focus on your “weak” areas…
Sleep:
You should be getting at least 8 hours of quality sleep per night. Failure to address a lack of sleep may result in weight gain (12) and persistent fatigue.
Diet:
With adrenal-related problems, it’s important to get adequate servings of carbohydrates (healthy carbohydrates like fruits and vegetables).
Make sure you are also eating a real, whole-food diet.
A diet like whole 30 is a great place to start.
Stress:
You need to be actively taking steps to reduce the impact of stress on your life.
If possible the complete elimination of stress from your life is ideal (but this isn’t always possible).
Instead, if you know will be under stress then you need to take steps to help reduce the impact that it plays on your body.
You can do that through regular meditation, the practice of yoga, the practice of religion, or the practice of mindfulness.
Each of these has been shown to help reduce the impact that stress plays on your life.
Exercise:
While exercise can be difficult with the crushing fatigue that accompanies adrenal-related problems it is still quite important.
Instead of focusing on going to the gym to sit on a treadmill for an hour, you should focus on staying active each and every day.
Simple changes like walking for 1 hour per day, taking regular breaks throughout your work day, and making time to do outdoor activities that are fun can make a huge difference.
If you have the energy to work out, make sure you don’t over-exercise and try to stick to 10-30 minute bouts of exercise at medium intensity.
Recap & Final Thoughts
Understanding your cortisol levels is critical if you are suffering from the symptoms of adrenal-related problems.
By understanding the difference between “optimal” and “normal” cortisol you can then determine how to treat your cortisol levels.
Start by testing your 8 am serum cortisol level and then move to DUTCH urine testing (4x urinary tests throughout the day) for optimal results but only if absolutely necessary.
Remember that the combination of supplements plus lifestyle interventions will be necessary for long-term success and a reduction in your symptoms.
Also, remember that treating your adrenals takes time!
I’m talking 6 plus months of active work may be necessary before you restore your adrenals back to optimal health.
Now it’s your turn:
Are your cortisol levels off?
Have you been able to improve your symptoms?
Why or why not?
Leave your questions or comments below!