As a thyroid patient, you should probably know a little bit about the protein known as thyroid peroxidase.
For starters, it’s one of, if not, the most important enzymes in your thyroid.
It is responsible for ensuring that your body can actually produce thyroid hormone.
If there is ANYTHING wrong with this enzyme then there is a good chance you will not be able to produce enough thyroid hormone and you may end up with the symptoms of hypothyroidism.
The good news is that most people don’t have any issues with thyroid peroxidase so they don’t have issues with thyroid function.
But many people, including those with Hashimoto’s thyroiditis, can develop antibodies to this very important enzyme.
And guess what happens if this occurs?
The enzyme is disrupted, you won’t be able to produce thyroid hormone, and you will become hypothyroid (or low thyroid).
We are going to spend a lot of time talking about this enzyme, how it becomes disrupted, what it means if you have antibodies to it, how to determine if your levels are normal, what symptoms are associated with high antibodies, and much more.
Before we do, though, let me explain a little more about thyroid peroxidase.
Thyroid peroxidase, when it is functioning normally, helps your body use iodine to create thyroid hormone (1).
It does this by oxidizing iodide into iodine, a process that is actually fairly dangerous for your thyroid cells.
This oxidation results in the formation of reactive compounds that can damage your thyroid gland!
When everything is functioning normally, your thyroid gland will use anti-oxidants to get rid of the dangerous compounds so no harm is done.
But if your body doesn’t have enough of these anti-oxidants your thyroid gland may become damaged.
When everything is working correctly, thyroid peroxidase creates iodine which is then taken up by another larger protein called thyroglobulin.
Thyroglobulin then smashes two halves of thyroid hormone together to form the full thyroid hormone complex.
Both thyroid peroxidase and thyroglobulin are incredibly important because they are often the site of thyroid antibody attacks.
And, often, when you see antibodies to one of these proteins you will see antibodies to the other (though not always).
Even though we aren’t talking about thyroglobulin antibodies today, I want you to realize that they are both important in creating thyroid hormones.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
What are Thyroid Peroxidase Antibodies?
What I just described is what thyroid peroxidase does inside of the thyroid gland but this is completely different from thyroid peroxidase antibodies.
If you’ve been told that you have thyroid peroxidase antibodies, also referred to as TPO antibodies, then this information applies to you.
Your body creates antibodies to things that it wants to kill or get rid of.
In a healthy state, you should really never see antibodies to any part of your own body or tissues.
Why?
Because why would you want to get rid of something that is supposed to be in your own body?
Antibodies are usually created to help your body eliminate infections or viruses (2) but they can sometimes be created by your immune system to target your own body.
When this happens you are said to have an autoimmune disease (3).
We can break apart the word to understand exactly what it means:
Auto (meaning self), immune (meaning your immune system), and disease (meaning something is wrong).
In the case of thyroid peroxidase antibodies, your own body is creating antibodies that target, damage, and destroy the thyroid peroxidase enzyme.
These antibodies are produced by the immune system and flow through your entire body until they find their target.
Once they reach their target their goal is to destroy it.
And because their target (thyroid peroxidase, in this case) is located in the thyroid gland, your thyroid becomes the site of a war between your immune system and thyroid peroxidase.
As you might imagine, this results in damage to your thyroid gland which can become permanent if the damage is severe enough.
Thyroid peroxidase antibodies are often associated with the autoimmune disease known as Hashimoto’s but that’s not all.
Conditions Associated with High Thyroid Peroxidase Antibodies (What Your Antibodies Actually Mean)
What does it mean if you have thyroid peroxidase antibodies floating around in your blood?
Well, it can mean several things:
- It may be a marker for the autoimmune disease known as Hashimoto’s thyroiditis.
- It may also be a marker for another autoimmune disease of the thyroid gland known as Graves’ disease (4).
- It may be a transient thing that may eventually go away on its own (which sometimes occurs in pregnancy (5)).
The presence of thyroid peroxidase antibodies is never “normal” but it doesn’t always guarantee a poor outcome.
For instance, as I mentioned above, some people see elevated antibodies during pregnancy which then fall after birth.
The significance of thyroid peroxidase in this exact setting is not well understood but it does give some hope that not every situation of elevated antibodies points to autoimmune disease.
Why would you want to check your thyroid peroxidase antibodies?
Your doctor can use this test in a number of useful ways:
- The first is to help diagnose autoimmune thyroid disorders – if you are experiencing certain symptoms (either symptoms of hypothyroidism or hyperthyroidism), your doctor can order this test to help with the diagnosis.
- The second is that checking thyroid peroxidase antibodies can help rule out other causes of both hyperthyroidism and hypothyroidism. If you have a non-immune mediated thyroid disease then checking your antibody level can help rule out autoimmune causes of thyroid disease.
- The third is that they may be helpful in diagnosing people who have “normal” thyroid lab tests but still experience thyroid-related symptoms. In some cases, your antibodies may elevate before any other thyroid lab test. You can use this to your advantage to get an early diagnosis if that is the case. Many conditions, including Hashimoto’s thyroiditis, often go undiagnosed until the condition is advanced because that is when you start to see abnormalities in thyroid function tests. You may be able to catch your disease early by testing for thyroid antibodies as opposed to thyroid function lab tests.
- Lastly, you can use thyroid peroxidase antibodies if you are having trouble with fertility. Elevated thyroid peroxidase antibodies are often associated with thyroid problems which are known to cause infertility. As mentioned above, the first sign of thyroid problems may be an elevation in your thyroid antibodies.
What is a Normal Level for Thyroid Peroxidase Antibodies on my Lab Tests?
When you get your thyroid peroxidase lab results you will see a range of what is considered “normal”.
The range is usually somewhere between 0 and 34 IU/mL (6).
If your thyroid peroxidase antibodies fall within the 0 to 34 range they will be considered “normal” and they won’t flag as high on your lab tests.
Any value that is higher than 34 IU/mL will flag as high and is an indication that thyroid dysfunction is likely on its way.
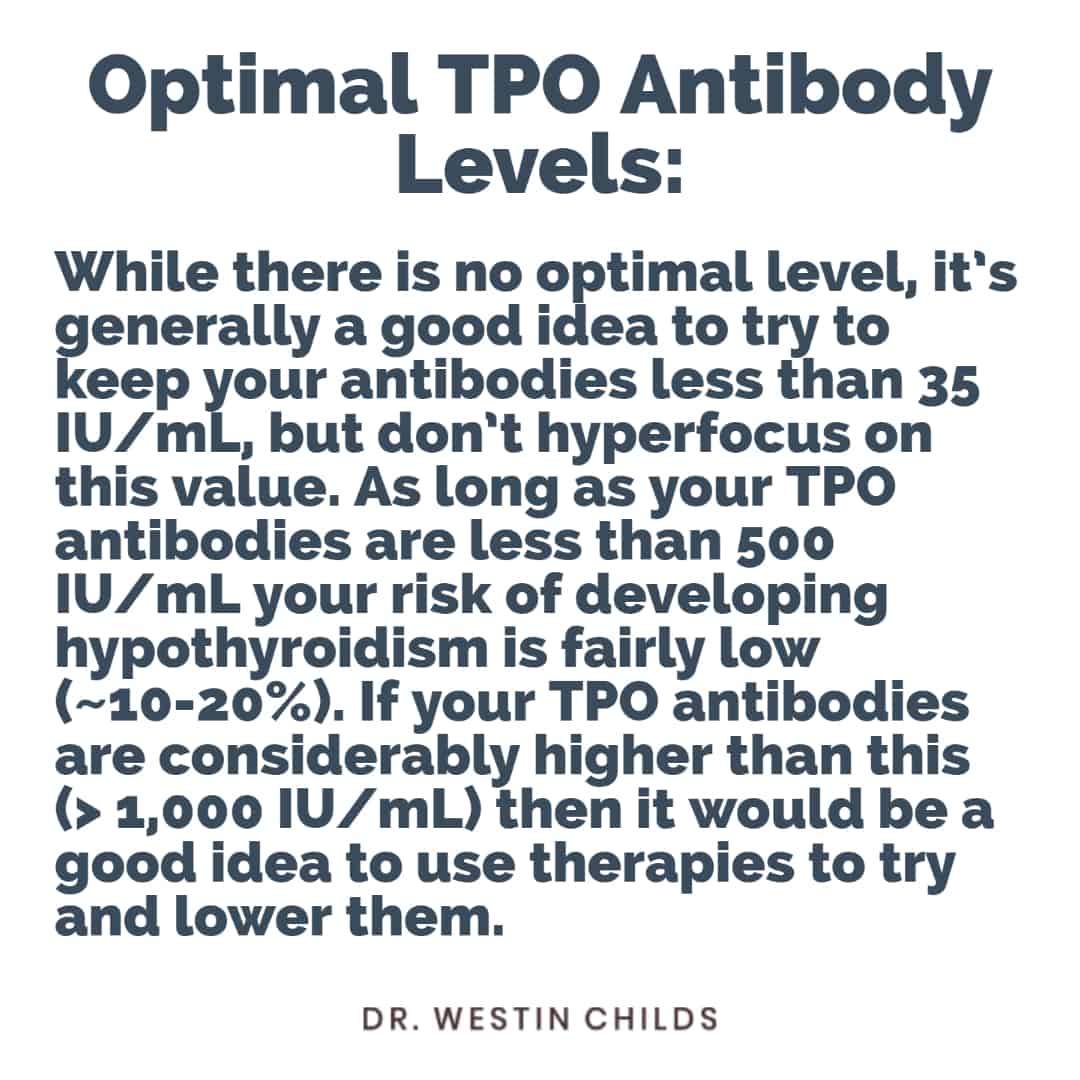
Despite this so-called “normal” range, there are a number of people who advocate for near-zero levels of antibodies.
The idea goes something like this:
Even though thyroid peroxidase antibodies of, let’s say, 25 IU/mL are technically “normal” wouldn’t it be better to have a value as close to zero as possible?
In other words, because the presence of any non-zero level of antibodies indicates a problem in the body, isn’t any level of thyroid antibodies a problem?
And the answer to this question is more complicated but I do tend to agree with the logic.
The presence of thyroid peroxidase antibodies (in any non-zero value) is probably more likely to be problematic in the future than not and should, therefore, be taken seriously.

Because of this, it is generally a good idea to aim for TPO antibody levels as low as possible so long as you aren’t causing more harm or stress to your body in the process.
Here’s why:
We know from some studies (7) that the risk of developing hypothyroidism with TPO antibodies in less than 500 IU/mL is still quite low, somewhere around 20% or so.
The higher your antibody level the higher your risk of developing thyroid disease in the future but this relationship seems to be non-linear.
But, as far as I’m concerned, a risk of 20% is still far higher than I would personally be willing to accept if I had this issue which is why I still advocate for lower thyroid antibody levels whenever possible.
Another way to think about this issue is like this:
Imagine that you are in the very EARLY beginning stages of developing Hashimoto’s thyroiditis.
Before you experience full-blown Hashimoto’s you will experience moderate Hashimoto’s.
And before you experience moderate Hashimoto’s, you will experience minor Hashimoto’s.
And before you experience minor Hashimoto’s, there will be a point when Hashimoto’s is in the process of developing in your body but before it is reflected in your lab tests.
If you can catch your thyroid disease process in its infancy then it will be easier to treat (see this article for more information on why this is).
With this in mind, it’s probably best for you to aim for thyroid peroxidase antibodies as close to zero as possible.
On the other end of the spectrum, we see thyroid patients who have incredibly high thyroid peroxidase antibody levels.
Some people see levels in the 1,000s and even in the 2,000s.
At the time of this writing, I don’t think I’ve ever seen anyone higher than the 2,000’s but it definitely happens from time to time.
Are Extremely High Thyroid Peroxidase Antibodies Dangerous?
The real question to answer here is whether or not the absolute level of thyroid peroxidase antibodies tracks with disease severity.
In other words, does having a higher level of antibodies (say, > 2,000) mean that your disease is more severe and more dangerous than someone with fewer antibodies?
The answer is not as clear cut as you might think but it is probably the case that the higher your antibody levels are the more severe and more dangerous your disease state.
Logically, this makes sense.
If you have more antibodies floating around in your bloodstream then there will be more damage done to your thyroid gland over a shorter period of time.
More antibodies mean more inflammation which means more thyroid gland damage which means more symptoms.
Evidence that supports this idea is in the case of seronegative Hashimoto’s.
Some people have Hashimoto’s with negative antibody levels, otherwise known as seronegative Hashimoto’s.
Patients with this condition experience much more mild side effects compared to patients who have high levels of antibodies in their blood.
Having said that, the presence of high thyroid peroxidase antibodies does NOT necessarily mean that your disease state is more difficult to treat.
Put another way, the presence of extremely high antibodies is worrisome but it doesn’t mean that you can’t do something about it (more information on that below).
We also know that thyroid antibodies play some role in the development of certain cancers (8).
Even if it isn’t the case that high thyroid antibodies destroy the thyroid gland faster, you still want lower antibody levels to reduce your risk of other conditions and disease states.
The Connection Between Thyroid Peroxidase Antibodies, Hashimoto’s, and Graves’ Disease
Does the presence of elevated thyroid peroxidase antibodies guarantee that you have Hashimoto’s?
Definitely not!
Elevated TPO antibodies are seen in 90-95% of patients with Hashimoto’s and 50 to 80% of patients who have Graves’ disease.
The best way to determine what your antibodies mean for you is to look at your thyroid lab tests, your thyroid peroxidase antibodies, and your symptoms:
- The presence of thyroid peroxidase antibodies with a LOW TSH and symptoms of hyperthyroidism point towards a diagnosis of Graves’ disease
- The presence of thyroid peroxidase antibodies with a HIGH TSH and the symptoms of hypothyroidism point toward a diagnosis of Hashimoto’s thyroiditis
- The presence of thyroid peroxidase antibodies with a normal TSH and no symptoms predicts an increased risk of developing a thyroid condition in the future
- The absence of thyroid peroxidase antibodies does not rule out hyperthyroidism or hypothyroidism as both of these conditions can be caused by other conditions
Symptoms Associated with High Thyroid Peroxidase Antibodies
Thyroid peroxidase antibodies typically do not cause any major symptoms by themselves.
They can sometimes be associated with minor symptoms including a minor decrease in energy, feeling run-down, or just feeling “blah”.
These symptoms occur as your body attempts to deal with the immune dysfunction present as well as minor changes to thyroid function.
Most of the major symptoms associated with TPO antibodies come from direct damage to the thyroid gland.
Remember the war zone that I mentioned previously?
Inflammation and damage to the thyroid gland may result in changes to thyroid function and this change to thyroid function results in symptoms that are hard to miss.
These symptoms vary based on whether you have a diagnosis of HYPERthyroidism (high thyroid function) or HYPOthyroidism (low thyroid function).
You can use your symptoms, in conjunction with your antibodies and thyroid lab tests, to see where you fit.
#1. Symptoms of Hashimoto’s Thyroiditis:
- Fatigue
- Weight gain
- Hair loss, hair thinning, or hair breakage
- Changes to the menstrual cycle
- Muscular pain
- Joint pain
- Constipation
- Cold intolerance
#2. Symptoms of Graves’ disease:
- Weight loss
- Hair loss, hair breakage, with fine/brittle hair
- Rapid menstrual cycle
- Anxiety and panic attacks
- Rapid heart rate
- Heart palpitations
- Tremors
- Sweating and hot flashes
- Heat intolerance
- Fatigue
#3. You may be asymptomatic.
Don’t forget that some people, especially those who are pregnant, may have no symptoms at all!
We don’t know how many people fit into this category, though because most people do not get tested for thyroid peroxidase antibodies unless they are feeling poorly at which point they can be diagnosed.
It’s also possible to be asymptomatic in the early stages of your disease, especially if you catch it early enough.
Is it Possible to Reduce Thyroid Peroxidase Antibodies If They are Elevated?
Absolutely!
And this might just be the most important part of this article.
After all, if you know that TPO antibodies are causing problems in your body, doesn’t it make sense to try and do something about them?
Of course!
But here’s the problem:
From the perspective of your doctor, there’s nothing that can be done about elevated thyroid peroxidase antibodies.
Doctors take what is called the “sit and wait” approach (9) to manage people who have elevated thyroid antibodies.
They sit and wait until your own body damages the thyroid gland to the point that you need prescription medication.
Just because your doctor doesn’t have any medical treatment options for you doesn’t mean you can’t do anything, though!
Seeing a doctor is important, for sure, but when it comes to managing your thyroid antibodies you are probably going to be on your own.
It may sound difficult but it actually isn’t.
Making some changes to your lifestyle can have an impact on your immune system and thyroid health and this may directly (or indirectly) help your antibodies.
Doing things like changing the food that you eat can have a huge impact on your antibody levels.
Avoiding foods that are known to be inflammatory is a great place to start.
Eating foods that are known to possess natural anti-oxidants and plant-based nutrients is also a wise decision.
You can also focus on improving your lifestyle.
Ensuring that you are sleeping enough each night, making sure that you are taking time for yourself, managing your stress, and exercising regularly can have an impact.
And guess what?
You don’t really need a doctor to tell you that eating fruits and vegetables is a good thing, right?
This should just make sense.
Even though it’s painfully obvious that these things work, so many people neglect them and instead take the advice of their doctor to “wait and see”.
If you are serious about preventing long-term damage to your thyroid then I would strongly recommend trying these therapies out to see if they can help you.
The best-case scenario is that they do and you see a reduction in your antibodies.
The worst-case scenario is that you don’t see a change but you have done zero harm in the process.
Final Thoughts
Remember:
There is a difference between the thyroid peroxidase enzyme and thyroid peroxidase antibodies.
The thyroid peroxidase enzyme is found within your thyroid gland and plays an important role in helping your body produce thyroid hormone.
Thyroid peroxidase antibodies are antibodies that your own immune system creates that target and destroy the thyroid peroxidase enzyme.
The presence of these antibodies indicates dysfunction in your immune system and is associated with several types of thyroid conditions.
If you find that your thyroid peroxidase antibodies are elevated you will want to take whatever steps necessary to try and reduce that number to as close to zero as possible!
Now I want to hear from you:
Do you have elevated thyroid peroxidase antibodies?
Do you know why your antibodies are elevated?
Do you know or suspect that you have a thyroid condition?
If so, what condition do you have?
Are you going to try and reduce your antibodies?
Let me know in the comments below!
Scientific References
#1. https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/thyroid-peroxidase
#2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4159104/
#3. https://pubmed.ncbi.nlm.nih.gov/26212387/
#4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1542488/
#5. https://pubmed.ncbi.nlm.nih.gov/20664399/
#6. https://journals.lww.com/md-journal/Fulltext/2020/09180/Normal_range_of_anti_thyroid_peroxidase_antibody.54.aspx
#7. pubmed.ncbi.nlm.nih.gov/28052092/
#8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5422478/
#9. https://www.mayoclinic.org/diseases-conditions/hashimotos-disease/diagnosis-treatment/drc-20351860