Hashimoto’s is the number 1 cause of hypothyroidism in the US and developed countries.
And while that statistic is interesting, there’s something much more interesting about Hashimoto’s…
The fact that many people who have Hashimoto’s have no idea that they do.
And it’s not because Hashimoto’s is a hard condition to diagnose.
Quite the opposite actually.
Because Hashimoto’s is an autoimmune disease, you can test for thyroid antibodies in the bloodstream.
The two thyroid antibodies associated with this condition include thyroglobulin antibody and thyroid-peroxidase antibody.
For most people, it’s as easy as checking your bloodstream for these two antibodies.
If they come back positive AND you have thyroid problems you are officially diagnosed with Hashimoto’s.
Sounds pretty easy, right?
Well, yes and no.
Despite how easy it is to diagnose Hashimoto’s, many doctors fail to order the antibody tests which leaves many patients diagnosed with a thyroid problem of unknown origin/cause.
But things can get a little more complicated than this.
It turns out that as many as 5-10% of people with Hashimoto’s have NEGATIVE thyroid antibodies in their bloodstream.
And yet, these people still have all of the signs and symptoms, including thyroid gland inflammation, of Hashimoto’s.
What gives?
There are at least 2 medical conditions in which you can have NEGATIVE thyroid antibodies but still have Hashimoto’s.
And it’s very important for you to understand if you have either of these conditions because if you don’t, you may never get the correct diagnosis.
Before you walk away thinking that it doesn’t matter whether you know if you have Hashimoto’s, let me address that as well.
There is a big difference in treatment between those with Hashimoto’s and those with regular run-of-the-mill hypothyroidism.
Knowing you have Hashimoto’s means that you can tailor your treatments to more than just thyroid function.
You can focus on treatments that ALSO impact your immune system.
Doing this will help you reduce the inflammation and damage to your thyroid gland and may help you prevent or reverse future damage.
Conditions that result in Negative Thyroid Antibodies
As I mentioned previously, there are at least 2 different medical conditions in which you can have Hashimoto’s thyroiditis without the presence of thyroid autoantibodies.
While it is uncommon to have Hashimoto’s and not have thyroid antibodies, these conditions are still fairly common.
It’s also unlikely that your doctor will even be thinking of these conditions and may not even be aware that they exist at all.
This means it will be up to you, as a thyroid patient, to have some basic knowledge that they exist.
You may need to advocate for some additional testing (which we will talk about below) if you strongly believe that you have Hashimoto’s in the face of negative antibodies.
With this in mind, let’s talk about the conditions associated with Hashimoto’s and negative thyroid antibodies…
#1. Seronegative Hashimoto’s Thyroiditis
The first condition is known as seronegative Hashimoto’s.
The word ‘sero’ refers to the serum, the word ‘negative’ refers to the absence of something, and ‘Hashimoto’s refers simply to the medical condition.
So we can break down the word to mean the absence of Hashimoto’s in the bloodstream (serum is another word used to describe testing in the blood).
And that’s exactly what this condition is.
People with seronegative Hashimoto’s do NOT have antibodies to thyroglobulin or thyroid-peroxidase (the typical antibodies associated with Hashimoto’s) and yet they still have Hashimoto’s.
How can this be?
Well, it’s not exactly clear but the hallmark of Hashimoto’s is inflammation and immune cell-mediated damage of the thyroid gland tissue.
And people who have seronegative Hashimoto’s do NOT have thyroid antibodies but they DO have this thyroid gland damage (which you can test for).
So clearly they have Hashimoto’s.
But, again, this is not a common occurrence among patients with Hashimoto’s.
Roughly 90% of all patients who have Hashimoto’s will have positive thyroid antibodies in their bloodstream.

This leaves the other 5-10% (depending on which study you look at) with negative antibodies but with the signs and symptoms of the disease.
5-10% is not insignificant, though, and it leaves roughly a 1 in 10 or a 1 in 20 chance that you may fall into this category.
People who have seronegative Hashimoto’s thyroiditis are often missed by both conventional doctors and even more experienced thyroid doctors/endocrinologists.
The only way to diagnose seronegative Hashimoto’s is by directly evaluating the thyroid gland with an ultrasound and doctors are not likely to order such a test unless they see thyroid gland enlargement.
Standard thyroid lab tests will not show the presence of this condition either.
While it is very difficult to diagnose, the silver lining is in the fact that it is often less severe compared to antibody-positive Hashimoto’s (1).
It is felt that those with seronegative Hashimoto’s have a less severe disease compared to those with positive antibodies.
But it’s still worth pointing out that therapies that impact immune function (including supplements, diet, stress reduction, detoxication, and so on) will still help those with seronegative Hashimoto’s.
In fact, the treatment between those with seronegative Hashimoto’s and those with antibody-positive Hashimoto’s is not any different.
#2. End-Stage Hashimoto’s Thyroiditis
There is at least one more condition that can make diagnosing Hashimoto’s difficult and that is end-stage Hashimoto’s.
People who have end-stage Hashimoto’s frequently do NOT have any antibodies present in their bloodstream, but clearly have Hashimoto’s.
But this group of people should be differentiated from those with seronegative Hashimoto’s.
Let me explain:
The standard course of Hashimoto’s (for 90% of people) is that thyroid antibodies slowly rise, reach a peak, and then eventually decline over time (2).
See this image below:
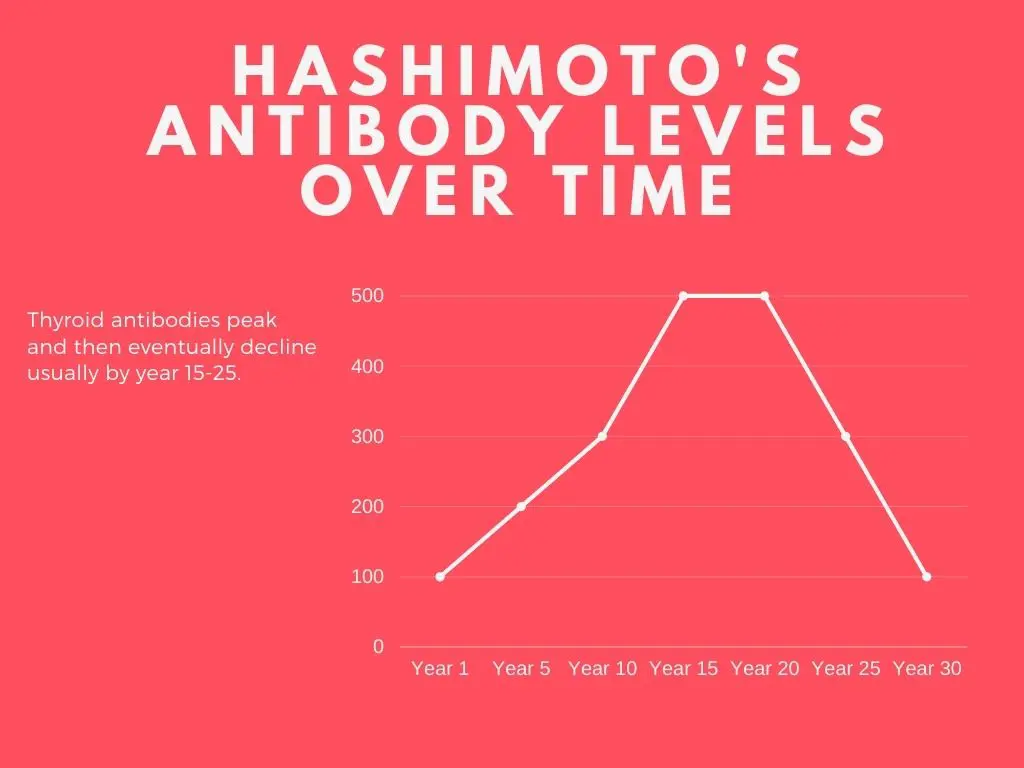
This is obviously just an illustration, but it shows what I am trying to explain.
The reason that antibody levels fall over time is due to the eventual destruction of the thyroid gland.
Your body produces thyroid antibodies designed to kill thyroid gland tissue.
Once the tissue is dead, the body no longer sees your thyroid as a threat and your antibody levels will fall.
But did your Hashimoto’s go away? Not really, it’s still there, you just don’t see the antibodies anymore.
People generally don’t miss this condition, though, because they have typically been diagnosed many years ago.
You don’t reach this end-stage until you’ve had Hashimoto’s for at least a couple of decades (usually 20+ years).
But it is still a condition in which you can have Hashimoto’s and NOT have positive antibodies so we are including it here.
How to Tell if You Have Hashimoto’s (Even if Antibodies are Negative)
I know what you are probably thinking…
“How can I test for Hashimoto’s if it won’t show up in my bloodstream?”
That’s exactly what we are going to talk about now.
There are several ways that you can identify if you have Hashimoto’s without checking for thyroid antibodies.
Looking for thyroid antibodies is obviously the easiest method, but you can’t count on it if you are one of the lucky (or unlucky, depending on how you look at it) few who have seronegative Hashimoto’s thyroiditis.
- Thyroid Ultrasound – The first and easiest way to identify Hashimoto’s is with a thyroid ultrasound. The thyroid gland is very superficial which means you can look at its shape, size, and other features using ultrasound. If Hashimoto’s is present, you will see signs of thyroid gland inflammation as well as changes to the normal volume of the thyroid gland. This usually is described as hypoechoic or dark patterns seen inside of the thyroid gland, a diffusely enlarged thyroid gland with heterogeneous echotexture, a doppler study with normal or decreased flow, and reactive cervical nodules (you might see this language on your ultrasound report (3)). In addition, you might see that your thyroid gland is enlarged (bigger than it should be) or smaller than it should be. Both can occur in Hashimoto’s and should not be seen in regular hypothyroidism. Getting a thyroid ultrasound is a very simple, non-invasive way to test for Hashimoto’s and it should be your first step if you believe you have seronegative Hashimoto’s.
- Complete thyroid lab tests – You can also look at your thyroid lab tests, and you should be getting these. And I’m not just referring to your thyroid antibodies. You can use your other thyroid lab tests (such as TSH, free T3, and free T4) to identify EARLY thyroid problems. If you find, for instance, that your TSH is normal and your thyroid antibodies are negative, but your free T4 and free T4 are low, then you might want to consider getting the thyroid ultrasound done. In this way, you can use your thyroid lab tests to help identify EARLY Hashimoto’s so you can get ahead on your treatment. The reason this is so important is that most people are not diagnosed with Hashimoto’s until they’ve had it for several years. If you check a full thyroid lab panel you may be able to diagnose your disease much earlier!
- Checking for inflammatory markers in the bloodstream – The next thing you will want to consider ordering are tests that assess for inflammation in your body. And specifically, I am talking about ESR and CRP. ESR stands for erythrocyte sedimentation rate and CRP stands for c-reactive protein. If either is positive then it’s a sign that you have inflammation in your body. This is important because regular causes of hypothyroidism are NOT associated with inflammation in the body. And remember, Hashimoto’s is first and foremost an immune disease which means that it IS associated with inflammation. If you find that you have high levels of inflammation in your body (because your CRP or ESR are elevated) AND you have thyroid problems (with negative antibodies) then it would be a good next step to get that ultrasound I talked about previously!
- Biopsy of the Thyroid Gland – Lastly, and I don’t recommend getting this done, you could always get a biopsy of the thyroid gland (4). Getting a biopsy is the gold standard for diagnosing Hashimoto’s, but it comes with a cost. When you stick a needle into your thyroid gland and pull out tissue, that tissue is gone forever. You don’t really want to cause permanent damage to your thyroid gland when you can get all of the information you need through other methods. I’ve included this option here though because sometimes it’s necessary to get a biopsy, in which case you might as well test for it, and for completeness’ sake. This should be your last option, though, for diagnostic purposes.
Wrapping it Up
Hashimoto’s thyroiditis is the #1 cause of hypothyroidism in the developed world.
As such, it’s incredibly important for patients who have this disease to get diagnosed with it as soon as possible.
There are some conditions that make diagnosing Hashimoto’s difficult because they are associated with negative thyroid antibodies.
These conditions include seronegative Hashimoto’s and end-stage Hashimoto’s.
You can diagnose these conditions by getting certain tests including a thyroid ultrasound.
For this reason, a thyroid ultrasound is a very helpful tool in patients who have thyroid disease!
Now I want to hear from you:
Do you have Hashimoto’s?
Do you have elevated antibodies?
Is your case of Hashimoto’s not as clear-cut as you want it to be?
Do you suspect or think that you have seronegative Hashimoto’s?
Leave your questions or comments below!
Scientific References
#1. https://pubmed.ncbi.nlm.nih.gov/24743395/
#2. https://pubmed.ncbi.nlm.nih.gov/18631004/
#3. https://radiopaedia.org/articles/hashimoto-thyroiditis
#4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3821498/




I have seronegative hashimotos. Mildly elevated TSH but five negative antibody tests over 3-4 years. Confounded me for years until I finally got an ultrasound that showed mild damage to the gland.
Go get checked if you’re having thyroid difficulties! It’s so much better to know what’s going on with your body.
seronegative Hashimoto’s, I had ultrosound came back normal, I have inflammation on my thyroid, I am taking armour thyroid. Any vitamins or nutrition should I take.
Hi Katherine,
Yep! You’d want to use the same supplements recommended for someone with regular Hashimoto’s 🙂 Please see this bundle: https://www.restartmed.com/product/hashimotos-bundle/
I have all the indicators for seronegative hashimoto’s, including a AI test by Cyrex Labs. I can’t find an ENDO that knows anything about this. Do I even need an ENDO?
Do you know any doctors of any sort that understand this who are located in Orange County, CA?
Hi Linda,
You don’t really need an endo to treat seronegative Hashimoto’s and, in fact, that would probably be the worst option: https://www.restartmed.com/endocrinologist-for-thyroid/
I would recommend checking out this resource for more information on how to find a knowledgeable doctor: https://www.restartmed.com/how-to-find-a-doctor-to-treat-your-thyroid/
Hi! I have had hypothyroidism since 2016 and have been on levothyroxine since then. I started to feel terrible about 5-6 months ago progressively starting with massive fatigue, joint pain, dizziness/vertigo, headaches/migraines, nausea, hair loss, dry skin, weight gain/increased appetite, mood swings and irritability, waking in the middle of the night every night and terrible gastro pain and constipation. I finally couldn’t take it anymore and had my TSH retested and it came back near 15 iu/ml. I never stopped taking my levo, by the way. My levo script was doubled about 2 months ago and I have experienced less fatigue and joint pain as well as some better sleep but overall I still don’t feel back to myself. I just took at at home test with Paloma Health to try to understand if I have Hashimoto’s and it says I do not. Results are below. I believe my results below are in the lower end of the normal range since my meds increased but I’m still not well. Could the levo dosage increase be masking the TPO results? Do these results mean I do not have Hashimoto’s? If not, how do I explain this sudden drop in my thyroid function and not feeling well yet despite standard treatment? I’m not sure what to do from here. Any help or advice would be so appreciated!
fT3 Result: 2.6 pg/ml (normal range: 2.1 – 4.2 pg/ml)
TSH Result: 1.1 uU/ml (normal range: 0.5 – 4.7 uU/ml)
TPO Result: 49 IU/ml (normal range: 0 – 60 IU/ml)
fT4 Result: 1.8 ng/dl (normal range: 0.8 – 2 ng/dl)
Hi Marcie,
Please see this article for more information 🙂 https://www.restartmed.com/reasons-hypothyroid-symptoms/
I don’t have antibodies and my ultrasound came back normal sized and clear, does that mean I have regular hypothyroidism?
Hi Vikki,
Most likely, yes. The only way to 100% know for sure is with a biopsy but that’s not really recommended. Instead of getting a biopsy, it would just be better to assume you have Hashimoto’s and use the treatments such as diet, exercise, supplements, etc. to improve thyroid function. There’s virtually no downside to using these therapies and they only have the potential to help.
Is it the same for hyperthyroidism? Can you have Grave’s disease if your antibodies are negative and ultrasound says thyroiditis?
Hi Anna,
Yes, there is a similar condition that can occur in Graves’ disease.
It really looks as if doctors don’t want to diagnose thyroid issues because it will ultimately cut into their pocket book. Instead of going to the root cause, they can treat all the symptoms associated with thyroid diseases with meds and can fill their pocket books with money.
Hi John,
I honestly don’t think it’s about money. The treatment for thyroid conditions (levothyroxine) is just a $4 generic drug so there isn’t much incentive to prescribe it from the perspective of the doctor. And the pharmaceutical companies would rather you pay for the much more expensive brand name drugs. Instead, I think it’s more about ignorance on the part of doctors.
I was diagnosed with Hashimoto- but: I have hyperthyroidism..\
how to treat such case?
Hi Anna,
It depends on which condition predominates!
Hey. Sorry to sidetrack the focus of the post, but this article has prompted a question. I’m a long-term Hashi’s patient. My last serum tests showed elevated TPO (1300+) and anti-Tg (129) antibodies, with low CRP (<0.5). Would you please comment – shouldn't CRP be elevated if the other readings are elevated? Thanks.
Hi Loz,
Not necessarily, CRP is just a nonspecific marker of inflammation.
defin “Low in relation to thyroid range. Labs as follows: TSH 5.90 H
Free T4 .88
Free T3 2.60
In relation to Hashimoto’s what do they mean? y VA doc isn’t talking.
Hi there, I have had low thyroid for about ten years but have never had a positive Hashimotos result. I take a very low dose of Tirosint (other meds make me feel like I am on speed and I have tried them all) for a few months now and a low dose has always kept my thyroid levels in check. In all of the years I have taken thyroid meds it has never varied from said low dose. I don’t have typical thyroid symptoms such as weight gain and fatigue, in fact I have the opposite, my symptoms present as hyperthyroid (weight loss and too much energy) yet when I am tested my results come back normal. I have always felt something else is in play that is effecting my thyroid yet no doctor will help or look beyond standard tests…any thoughts?
Hi Terri,
Have you had a complete thyroid lab panel yet? If not, that’s the first place to start: https://www.restartmed.com/thyroid-tests/
I have had hypothyroidism for well over 20 years but never tested positive for antibodies. Suspecting seronegative hashimotos, I finally got a thyroid ultrasound that shows the following: thyroid is smaller than normal, no cysts or masses, normal color flow, both sides show heterogeneous echogenicity. Does this mean I have hashimotos?
Hi Donna,
The findings of your ultrasound should be discussed with your physician. You can see this article for more information on what heterogeneous echogenicity may imply/mean for your thyroid gland: https://pubmed.ncbi.nlm.nih.gov/24237991/
My 23yo daughter has had thyroid symptoms for 2 years. Her ultrasound shows her thyroid is enlarged and heterogeneous. No nodules. Her tsh has been .9 at the last test and her free t3 is just above mid range at 3.5. Her free t4 is just below midrange at 1.24. Would it be appropriate to be on a thyroid med to help shrink her thyroid and help symptoms? She sees a gastroenterologist and rheumatologist who have not found a diagnosis. The endocrinologist is considering thyroid treatment.
Hello Dr.,
I have hypothyroid symptoms that started over 10 years ago, prior to the hypothyroid symptoms I had hyperthyroid symptoms. My antibodies are negative and my TSH has very slowly increased starting at 1.08 with hyperthyroid symptoms to 4.35 now. Recently had an ultrasound and no follow-up yet, but I seen the online report stating nontoxic multinodular goiter…? Does that mean my thyroid has been under attack? And if so does that mean my numbers will just increase more and more until I have to take medication? Just recently diagnosed with narcolepsy and that’s autoimmune, so maybe I’m finally about to get all the reasons for my medical nightmares for all these years. As bad as I feel I should have Discoverable antibodies and through the roof numbers! But I don’t. So confused.
Hi Mel,
The story presented here is a little bit confusing. Normally, people experience hyperthyroid symptoms as the TSH declines (not increases) so perhaps I am not understanding the store completely. Can you please clarify?
It would be really nice to know what I have. I was diagnosed with hypothyroidism 28 years ago. Nothing more was ever said. 18 months ago, I was told I had Hashimoto’s thyroiditis during a thyroid ultrasound but have consistently showed negative blood test for both TPO AND TgAB. During my ultrasound I was told the right side was dark “black” with 2 nodules. The left side was lighter but not bright with 1 micro nodule. The size was average but definitely not enlarged. I have had continual sore throats and many other issues that relate to Hashimoto’s. So it sounds like I have seronegative or endstage Hashimoto’s… what does that mean? What do I don?
Hi Shannon,
There isn’t enough information here for me to say for sure but it may also be that you are just in the end stages of Hashimoto’s thyroiditis which is why your antibodies have declined: https://www.restartmed.com/end-stage-hashimotos/
I was not diagnosed with Hashi’s until I was 36. I was always a sickly child with dark circles under my eyes, zero energy, sinus infections and laryngitis that would keep me out of school for weeks. Being on Levothyroxine helped but it never made me 100% better. I have always suspected I had Celiac disease but the tests never show up. I always look like I’m pregnant while the rest of my body is normal and I have been pre-diabetic for years. After my Father’s death, I officially became diabetic but Metformin does not agree with me so I just exercise and take Berberine or Gymnema Sylvetre which I thinks works better than Metformin with no side effects. I started following the gluten free just last week and have noticed a dramatic different in the my elimination system. We’ll see how this goes. I will try some of your supplements and let you know.
Hi Rene,
That sounds like a good place to start! You can also learn more about additional therapies aside from supplements here: https://www.restartmed.com/natural-remedies-for-hashimotos-thyroiditis/
Hi!
I have a family history of lupus, and hypothyroidism that does not show in labs, but I have all the associated symptoms. Also have Raymauds to add. Recently have had chronic hives. Could this be a Hashimotos?
Hi Amanda,
It could be, yes, but you’d want to get an ultrasound of the thyroid to check for inflammatory changes or signs of thyroiditis before stating it as such.
Dear Dr. Childs,
Thanks for this video!
I’ve been treated for hypothyroidism for nearly 30 years now, first with porcine thyroid, then T4 only until recently. Finally had antibody tests done and they are negative. Last year, I had a parathyroid adenoma removed and the surgeon remarked that my thyroid appeared quite atrophied. I’m assuming this means I currently have (or have in the past had) sero-negative Hashimotos. I’ve been on T3 and T4 for the past year or two. What other therapies, if any, could be helpful at this point?
Hi Laurie,
Tons! I would recommend checking out these resources:
https://www.restartmed.com/natural-thyroid-remedies/
https://www.restartmed.com/thyroid-supplements/
I have had my thyroid levels checked periodically throughout the last 13 years or so when I was first diagnosed with Raynaud’s and it was always normal. Recently I was feeling “off” so I had my TSH checked and it was 6.643 (0.43-3.55). I notified my PCP who had me wait a while and recheck. The repeat TSH was 6.488 and the free T4 was 0.76 (0.7-1.25) and antithyroperoxidase antibodies were 25 (<33). My PCP then ordered a thyroid ultrasound which read: Heterogeneous and hypervascular thyroid, possibly related to thyroiditis, no discrete nodules identified. Right lobe 3.9X1.5X1.8, Left lobe 4.1X1.4X1.7. Would I be considered the 5-10% testing negative for antibody or am I still an inconclusive case? I eat healthy and exercise which I think keeps most of my symptoms manageable. My PCP has ordered a low dose of synthroid. I do see a rheumatologist regularly since my Raynaud's diagnosis. I also am treated for dry eyes since 2019. Blood tests for Sjogren's were negative though clinical exam by the opthamologist confirmed inflammation in the eyes. Also have always had normal inflammation markers, ESR, CRP. I do have a positive ANA.
I’ve showed symptoms of thyroid disease for over a decade but can’t get a diagnosis or treatment. I’ve been to as. Primary care, allergist, hormone specialist, gynecologist, endocrinologist, dermatologist, and rheumatologist. Does this ever present with a rash?
Hi Joy,
I’m sure it’s possible that Hashimoto’s could present with a rash but I would say it’s highly unusual that this would be the predominant and only symptom. It’s far more likely that someone with Hashimoto’s would present with the combination of a rash plus other thyroid-specific symptoms.
I’m 33f. I had been experiencing fluctuations between hypo and hyper symptoms for a few years and when I asked my doctor to test my thyroid he said I couldn’t have symptoms from both so it must be mental health. However the phases of hyper have been getting more debilitating especially when I lost my voice for 5 weeks and had trouble swallowing. I kept going back saying I think its my thyroid but was told it was probably a virus. All bacterial and viral swabs were negative. TSH was normal. But Symptoms kept persisting and I keep persisting until finally they agreed to a thyroid panel and send me for an ultrasound which showed mild enlargement and inflammation.
TSH 2.47 mIU/L
Free T4 13.5 pmol/L
TPO Ab < 28.0 IU/mL
Thyroglobulin Ab < 1.3 IU/mL
TSH-R Ab < 0.10 IU/L
Euthyroid.
GP then diagnosed subacute viral thyroiditis and said it would go away on its own. It has recurred twice in the last 6 months. I have a family history of hashimotos. I asked for repeat bloods and they've gone back to only testing TSH which was 2.88 this time. I have pushed for a repeat ultrasound to see if anything has changed. I've been given a referral to an ENT not a rheumatologist.
Does this sound like the onset of serum negative hashimotos?
How can my bloods look so normal but feel this atrocious. My hair is falling out my muscles are so weak and achy, insomnia is ridiculous, this really strange pervasive jittery anxiety that isn't situational and doesn't go away despite all the meditation, polyvagal techniques and being really consistent with therapy. I have this constant heat and pressure in my neck and I keep loosing my voice which I need for work! I get so hungry I have to get up and eat during the night and yet I'm lighter than I was as an 10 year old. When I do get sleep, waking up feels like being hit by a truck.
Hi Holly-lee,
Whether it is or not is mostly irrelevant as it really wouldn’t change the treatments all that much. You’re still going to want clean up your diet, exercise more frequently, take thyroid supporting supplements, etc. You can start with these treatments and then, depending on what type of improvement you see, add in the more Hashimoto’s specific treatments down the line. But the core treatments don’t really change that much so the uncertainty regarding which exact thyroid problem you have is less important early on.
If Serum Negative Chronic Autoimmune Thyroiditis is suspected and you go on meds. Wouldn’t your levels then become hyper ?
Hi Linda,
No, because you can still have inflammation and damage to the thyroid gland, resulting in hypothyroidism, without antibodies. It’s certainly still possible to take too much thyroid medication resulting in the hyperthyroid state, though.
I spent 14 years going from one specialist to another trying to figure out what was wrong. I has neurological symptoms with my Hashimotos. I was misdiagnosed with MS. All my labs were always in the normal or borderline normal range and the one or two times they tested for thyroid antibodies I was negative. 14 years after onset of symptoms, a cervical spine MRI revealed a large nodule on my thyroid. I was sent for an ultrasound needle biopsy that came back with suspected thyroid cancer. Had to have thyroid removed and the biopsy revealed Hashimotos.
Hi Shellye,
Thank you for sharing your story and experience. It sounds like a frustrating and difficult journey.