Thyroid hormone absolutely does impact both your blood pressure and heart rate.
But what are you supposed to do if you feel good on your thyroid medication but you still have high blood pressure?
How can you manage high blood pressure on medications like Cytomel, liothyronine, or Armour thyroid (which are actually amazing for thyroid patients)?
If you are experiencing high blood pressure while taking thyroid medication then this article is for you.
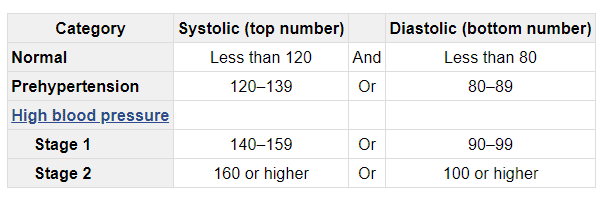
Your goal, as a thyroid patient, should be to have a blood pressure that is no higher than 120 over 80 mmHg (1).
Let’s talk about the changes you can make to your medication to normalize your blood pressure.
Thyroid Hormone and Your Heart
It is well known that thyroid hormone influences your heart.
And, because your heart pumps blood throughout your body, any changes to your heart rate or force of contraction can also cause changes to your blood pressure.
We also know, from plenty of studies, that maintaining a healthy blood pressure is absolutely vital to leading a long life and avoiding complications such as stroke, end-organ damage, kidney failure, and heart disease.
Doctors go to great lengths to help manage blood pressure because of these negative side effects!
So, why (or how) then does taking thyroid medication cause high blood pressure in some situations?
It has to do with how thyroid hormone interacts with cardiac tissue (heart cells).
In almost every cell in your body thyroid hormone works by entering into your cell and changing genetic transcription (2).
This process results in changes to your DNA which take weeks to kick in.
But in your heart cells, thyroid hormone activates receptors on a different part of the cell.
This means that the effects of thyroid hormone occur much faster when compared to the genetic changes that occur in other cells in your body.
Through this mechanism, thyroid hormone medication can potentially lead to elevated blood pressure even though you might feel great otherwise.
Effects of Thyroid Hormone on Your Blood Pressure
When you are hypothyroid (meaning that your body can’t produce enough thyroid hormone on its own) you may need to take thyroid medication.
These medications (you probably know them as Synthroid or levothyroxine) contain thyroid hormones and are meant to supplement whatever thyroid hormone your body can produce naturally.
If your body can only produce 80% of whatever is normal thyroid hormone for you, then we try to give you back that other 20% so you can get as close to 100% as possible.
The problem is that sometimes you can actually get more than you need.
Imagine if your body produces 80% but we give you back 40%.
All of a sudden your body is getting 120% of whatever is considered “normal” for you.
This is when side effects such as heart palpitations and elevated blood pressure tend to kick in (there are other reasons that I get into below as well).
As you take too much thyroid medication your heart may start to beat faster and harder which results in an increase in blood pressure.
This effect is regulated through calcium channel pumps (3) found on your cardiac cells (the same pumps and channels that blood pressure medications block to LOWER your blood pressure).
The more thyroid hormone that you take (beyond what is considered normal for you) the more these pumps will work, the higher your blood pressure will go, and the more symptomatic you may become.
The good news is that you can relatively easily modify your dose of thyroid medication to fix this problem.
Effects of Thyroid Hormone on Your Heart Rate
I’m mentioning heart rate here because both high blood pressure and heart palpitations tend to occur hand-in-hand.
Why?
Because thyroid medication is stimulating to both the FORCE and CONTRACTION of the heart.
If you increase the force with which your heart beats then you will naturally be increasing your blood pressure.
If you increase the contraction rate of the heart, along with the force with which it beats, then that is a recipe for a symptom known as heart palpitations.
This sensation can be uncomfortable for people and some people even describe it as painful.
But this condition needs to be differentiated from a rapid heart rate which is known as tachycardia (5).
It is certainly possible to have both heart palpitations AND tachycardia (rapid heart rate) but they don’t always go together.

In fact, most people with heart palpitations do not have tachycardia, they just feel their own heart beating.
I find that most people are often surprised when I check their actual heart rate and find the rate to be in the 70’s (beats per minute).
People with heart palpitations feel like their heart rate must be racing, but that is usually not the case.
The way to deal with heart palpitations is very similar to the way to deal with blood pressure (more info on that below).
How to Deal with High Blood Pressure From Thyroid Medication
If you are taking thyroid medication and you notice that your blood pressure is raising then that is certainly an issue.
But how do you deal with it?
#1. The first step is to take a look at your dose.
Is it possible that your dose is too high? Is it possible you are taking too much thyroid medication?
If so, then that is the most obvious and common cause of high blood pressure secondary to thyroid medication.
Excess thyroid medication results in excess thyroid hormone in your body which will overstimulate your heart.
As your heart is overstimulated with thyroid medication it will respond by increasing your blood pressure and your heart rate.
There’s an easy fix for this:
Simply reduce your dose.
You can check to see if your dose is too high by looking at your thyroid lab tests.
If your dose is too high you will most likely notice a low or suppressed TSH in combination with high free T3 or high free T4.
#2. The second step is to take a look at the type of medication you are using.
Not all thyroid medications are created equal!
For instance:
It’s much more likely that you are experiencing high blood pressure or heart palpitations if you are using thyroid medication that contains T3 thyroid hormone.
Medications like Cytomel, liothyronine, and even high doses of Natural Desiccated Thyroid are notorious for causing high blood pressure and heart palpitations.
But this can often put you in an interesting predicament.
Why?
Because most people who switch to these medications often feel BETTER on them.
In fact, blood pressure is not usually something that causes any symptoms, but it is still concerning.
So, how do you reconcile the fact that you feel better on these medications and yet you are still experiencing negative symptoms?
It has to do with how thyroid hormone influences different cells in your body.
You see…
Your heart tissue is much more sensitive to thyroid hormone (especially T3) when compared to other tissues in your body.
If you flush your heart with a large amount of T3 (exactly what happens after you take thyroid medication and it is absorbed into your intestinal tract) you may experience an elevation in blood pressure.
The good news is that this can absolutely be managed and the way to do it is by reducing how quickly thyroid hormone is absorbed into your bloodstream.
Let’s stay that you are taking 10mcg of Cytomel each day.
If you take all 10mcg at once then it will be absorbed into your body about 2-3 hours after you take it by mouth.
Around that time your heart will be flushed with this hormone.
But what if you split it up into 2 or 3 doses throughout the day?
By doing this you are still getting the same TOTAL amount of Cytomel but your heart gets slightly different doses instead of getting hit all at once.
This strategy works when dealing with both heart palpitations and elevated blood pressure from Cytomel and liothyronine.
Another option is to switch to a sustained-release version of T3 medication.
SR T3 is specifically formulated to delay the release of T3 into your system, so you can still take your total dose all at once but instead of it being absorbed rapidly it is absorbed slowly throughout the day.
In order to get this medication, you will need a prescription to a compounding pharmacy from your Doctor.
#3. The third step is to consider switching thyroid medications.
What if none of these options work for you?
Your last option is to simply switch to a different medication or switch to a T4-only thyroid medication.
T4-only thyroid medications such as Synthroid and levothyroxine tend to not be associated with high blood pressure (unless your dose is extremely high).
Maintaining high blood pressure for years and years is not something that you want to do.
It is well known in the scientific community that high blood pressure leads to vascular conditions and increases your risk of organ damage and even stroke.
These consequences are usually only seen after years and years of high blood pressure, though, so don’t let them freak you out if you just noticed your blood pressure is slightly elevated.
You have a few months to play around with your medication to try and lower your blood pressure, but it’s certainly not something you want to ignore.
Taking Blood Pressure Medications
It’s also entirely possible that you may suffer from high blood pressure from an unrelated cause!
The people I am talking to in this article are those who have normal blood pressure before they start taking thyroid medication and then suddenly experience high blood pressure.
If you have high blood pressure at baseline and then it stays high after taking thyroid medication then you probably just have high blood pressure from some other cause.
What’s important here is that some blood pressure medications can interfere with your thyroid function.
Medications like beta-blockers can slow down thyroid peripheral conversion (6) which may make your thyroid medication slightly less efficient.
This can be a good and a bad thing.
If you find that you are incredibly sensitive to heart palpitations from your thyroid medication then using beta-blockers may be the only way you can use thyroid medication without experiencing heart palpitations.
But, on the other hand, taking a beta-blocker for blood pressure can negatively impact your thyroid function and potentially make you feel worse.
The moral of the story is to try and AVOID taking blood pressure medications if you have thyroid disease of any type.
This means you will need to focus on the underlying cause of your elevated blood pressure instead of trying to cover it up with anti-hypertensives.
One of the major causes of high blood pressure is insulin resistance (7) and obesity (8) (both of which can be worsened by hypothyroidism).
But, in addition to obesity, other conditions such as stress (9), smoking, a poor diet, and a lack of exercise can all contribute!
If you address insulin resistance and lose weight, there is a high chance that your blood pressure will not only improve but your thyroid function will as well.
Conclusion
Thyroid medication can definitely impact your blood pressure in a positive or negative way.
The goal when using thyroid medication is to try and normalize your blood pressure and get you back to a healthy level.
Sometimes, if you take too much medication, or if you take certain medications that contain T3, then your blood pressure might start to rise beyond normal.
If this happens to you then you can get your blood pressure back to normal by modifying your dose (or potentially switching your medication).
Now I want to hear from you:
Are you dealing with high blood pressure from your medication?
Have you been able to take any steps to reduce your blood pressure?
What has worked for you? What hasn’t?
Leave your comments or questions below!
Scientific References
#1. https://www.ncbi.nlm.nih.gov/pubmed/12698067
#2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC329808/
#3. https://www.ncbi.nlm.nih.gov/pubmed/9064969
#4. https://www.ncbi.nlm.nih.gov/pubmed/9160219
#5. https://www.mayoclinic.org/diseases-conditions/tachycardia/diagnosis-treatment/drc-20355133
#6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1714646/
#7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996172/
#8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5038894/
#9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3694268/