Thyroid deiodinase enzymes serve to manage thyroid hormones at every level of metabolism.
Even more important is the fact that these enzymes can become dysregulated by everyday common medical conditions.
Understanding the importance of these enzymes is critical to understanding how to further treatment, especially if you are taking thyroid medication such as levothyroxine or Synthroid.
This post will break down these deiodinase enzymes, in an easy-to-understand way, and teach you the basics including what they do, what conditions cause disruption in how they function, genetic problems associated with them, and more:
What is Thyroid Deiodinase?
I’m going to try and talk about one of the more complicated aspects of thyroid function and try to make it easy to understand.
If you have thyroid problems, and this could be anything ranging from hypothyroidism to hyperthyroidism, then you need to have at least a basic understanding of thyroid deiodinase enzymes.
These deiodinase enzymes are in most of the cells in your body and they are the things that help your thyroid do its job.
If you know a little bit about thyroid function then you probably know that it’s an incredibly important topic.
Why?
Because up to 5-10% of the population suffers from thyroid disease in some way and the management of thyroid-related problems results in unhappy patients (1).
A large part of the problem relating to unhappy patients with thyroid disease may have to do with a fundamental misunderstanding of how thyroid hormone operates in the body.
It’s much more complex than your thyroid gland releasing thyroid hormone into the bloodstream and calling it a day.
It turns out, instead, that thyroid hormone is highly regulated by these deiodinase enzymes which serve to either activate, inactivate, or control the concentration of thyroid hormone in both your cells and bloodstream.
Thyroid Function and Deiodinase Enzymes
To help illustrate and explain what deiodinase enzymes do we are going to use a simple image:
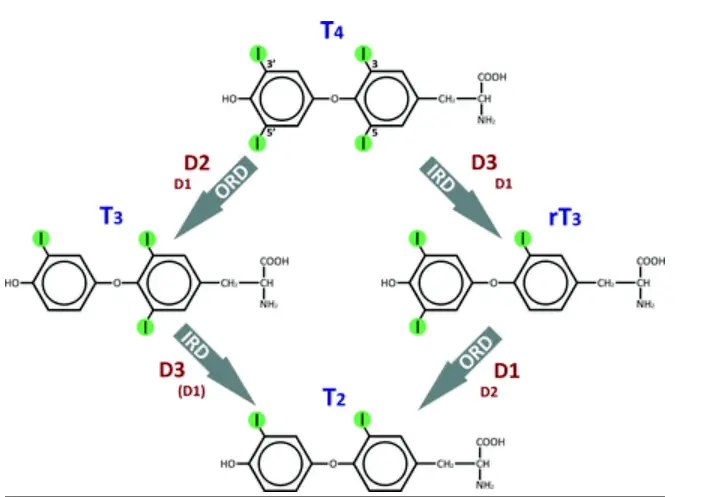
Don’t let the image scare you away because I’m going to explain it:
This image illustrates how T4 (the predominant thyroid hormone) is metabolized inside your body and inside of your cells.
T4, also known as thyroxine, comes from the thyroid gland where it is produced under the influence of TSH (thyroid stimulating hormone).
Once your body produces T4, also known as thyroxine, it is then acted upon by the deiodinase enzymes to either become active as the T3 thyroid hormone or become inactive as the reverse T3 (rT3) metabolite.
Your body uses these enzymes to tightly regulate thyroid hormone activation and inactivation depending on what is happening to your body.
Factors such as stress, how much food you eat, exposure to bacteria, illness, medications, the presence of hormone imbalances, and nutrient deficiencies all impact how well (or not) your enzymes function.
And the function of these enzymes is perhaps more important than the status of free thyroid hormone levels in your body!
Studies have shown that the concentration of free thyroid hormones in your body (meaning what is produced by your thyroid gland) is not produced in high enough amounts to adequately trigger thyroid hormone receptors inside of your cells (2).
The only way they can achieve a high enough concentration to actually become active is through the influence of these enzymes.
To make this clearer let’s break down the process of thyroid hormone physiology, starting from the beginning:
- TRH is produced in the hypothalamus.
- TRH stimulates the release of TSH from the pituitary.
- TSH stimulates the release of T4 and T3 directly from the thyroid gland
- T4 circulates in the bloodstream to target tissues such as your liver, kidney, muscles, heart tissue, brain cells, skin cells, and so on.
- T4 is either activated or inactivated based on the demand of each tissue. If you are exercising and using your muscles then your body may activate more thyroid hormone in your muscles but deactivate it in your intestinal tract (you don’t need to digest food while exercising!). If you are thinking really hard or studying for a test your body may activate more thyroid hormones in your brain and inactivate some in your muscles.
- Deiodinase enzymes are responsible for controlling the activity and metabolism of thyroid hormone systemically (for the whole body) and locally (in each cell).
- The amount of T4 and T3 feedback up to your hypothalamus which influences how much TRH is being released.
This is a (very) simplified version of the entire process from start to finish, but it really helps put everything into context.
It’s also important to realize that most physicians focus only on step 2 of this process, where TSH is produced, and use TSH as a marker for assessing the entire process.
By doing so, these physicians are missing out on the impact and important role of deiodinase enzyme activity and how they influence specific tissue levels of thyroid hormone.
This, in my opinion, is, at least in part, why so many thyroid patients are unhappy with their current thyroid management and treatment plan!
Now that you have a basic understanding of how these enzymes work we can dive into the three main enzymes and what they do for your body:
Function of D1
D1, also known as DIO1 or iodothyronine deiodinase 1 (3), should be considered an ‘activating’ thyroid enzyme.
The main job of D1 is to help control how much thyroid hormone is being produced from the thyroid gland and it also contributes to T3 levels found in the serum.
D1 plays a major role in regulating how much thyroid hormone is being produced systemically or for the entire body.
DIO1 is found in the liver, kidney, thyroid, and pituitary tissues.
The liver and kidney are organs in your body that receive a rich supply of blood, so it makes sense that these tissues contain the D1 enzyme.
As the blood reaches these organs, D1 can take the T4 which is being produced from the thyroid gland, and either activate it or tell the body to produce more.
Naturally, as you might suspect, a decrease in this enzyme would result in lower than normal free T3 levels and lower than normal T3 and T4 levels in the blood.
Function of D2
D2, also known as DIO2 or iodothyronine deiodinase 2 (4), can also be considered an ‘activating’ enzyme.
DIO2 is responsible for the majority of T4 to T3 conversion found in circulation around 70%.
You can compare this value to DIO1 which is responsible for around 30% of T3 found in the bloodstream.

You can think of D2 as being the most important regulator of thyroid function and metabolism in the peripheral tissues or inside of the cells.
In this way, D2 is primarily responsible for activating and inactivating thyroid hormone cellularly and based on the demands of each tissue.
DIO2 is found in the thyroid, central nervous system, pituitary, and skeletal muscle.
A problem with DIO2 may result in reduced free T3 levels.
Function of D3
D3, also known as DIO3 or iodothyronine deiodinase 3 (5), should be considered an ‘inactivation enzyme’.
D3 is responsible for taking T4 and inactivating it by turning it into the inactive metabolite reverse T3 (rT3).
D3 also stimulates the breakdown of the active thyroid hormone T3 into a less active form known as T2.
So, your body can upregulate the expression of DIO3 to help inactivate thyroid hormone at the cellular level and in the serum.
There are certain conditions that cause your body to increase the function of DIO3 while downregulating the function of the other enzymes.
These problems, which you’ll find to be quite common, are discussed below.
Dysfunction Causes Thyroid Abnormalities
Remember when I said that most physicians don’t take into account the function of these enzymes?
It may turn out that this is a big mistake.
We already know, undisputedly I might add, that these deiodinase enzymes impact how thyroid hormone is processed in your body.
The prevailing thought, when it comes to thyroid management, is to assume that the body does the conversion process perfectly well and without any issues.
So, as the thought process goes, if you provide the body with enough substrate (in the form of T4 thyroid medication) then it will have no problem activating or inactivating thyroid hormone as it sees fit.
There’s one big problem with this logic:
There are many factors, that many patients suffer from, that serve to inactivate these deiodinase enzymes.
Below you’ll find a list of common medical conditions that result in the deactivation or inhibition of deiodinase enzymes with clinical references:
- Inflammation: Inflammation inhibits DIO1 activity (6) thereby reducing thyroid conversion capacity.
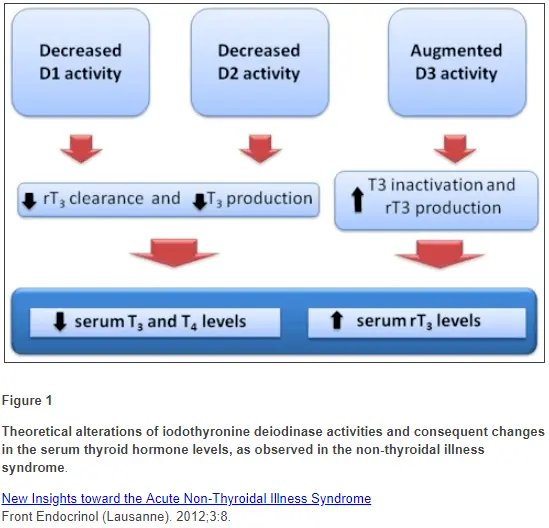
- Nonthyroidal illness or euthyroid sick syndrome: This thyroid lab pattern results in decreased D1 and D2 activity with an increase in D3 activity (7). The net results are decreased free t3, high reverse T3, and a normal TSH. This condition is the result of many conditions including recent acute illness, chronic illness, and dieting.
- Exposure to LPS: LPS (which stands for lipopolysaccharides) causes a decrease in DIO1 expression and activity (8). LPS or endotoxin are components of the bacteria in your gut. In conditions that result in increased intestinal permeability (commonly referred to as leaky gut), LPS levels may rise and cause dysfunction in thyroid function.
- Dieting and Fasting: Fasting and caloric restriction have been shown to reduce deiodinase activity (9). This is probably a protective response from the body to help reduce caloric burn in starvation states and may explain why dieting is harmful to thyroid function.
- Selenium Deficiency: Selenium is required for deiodinase activity (10) and a deficiency in this mineral results in both decreased receptor expression and decreased enzyme function.
- Insulin resistance: Excess insulin (known as insulin resistance) has been linked to certain polymorphisms in deiodinase enzymes (11).
As you start to dive into this concept more heavily you may notice that many of the problems listed above are common among medical conditions that patients suffer from today.
Take for instance inflammation:
The inflammatory process is at the heart of almost all major disease states and medical conditions ranging from heart disease to gingivitis.
From your perspective, what this means is that these conditions, which many of you probably have, may further disrupt your thyroid hormone status and complicate your medication management.
Thyroid Lab Tests vs Deiodinase Enzymes – Which is More Important?
While we know that the function of these deiodinases is of utmost importance to your thyroid function, how do they fit in together with your thyroid lab tests?
Currently, we don’t have a great way to assess the function of deiodinase activity because all of this activity is happening inside the cells in your body.
Studies have even gone as far as to say that the function of these enzymes is more important than the absolute level of thyroid hormone in your body or serum.
Why?
Because, even in the presence of low circulating thyroid hormone, your deiodinase enzymes can potentiate the action of thyroid hormone by constantly activating T4 into T3.
Imagine this scenario:
Let’s assume that you have hypothyroidism from Hashimoto’s thyroiditis.
Hashimoto’s, as you know, causes damage to the thyroid gland which ultimately results in a reduction in circulation of T4 and T3 in the body.
This reduction in thyroid hormone will be felt by cells in the body and the consequence will be a change in how deiodinase enzymes function.
As T4 levels fall, your body may constantly attempt to keep T4 to T3 conversion active in the cells to keep T3 levels high enough to latch onto thyroid hormone receptors and activate genetic transcription.
This is primarily done through the upregulation of deiodinase activity (12) (especially D1 and D2) and the downregulation of D3 activity.
So, your body can maintain a relatively “normal” level of thyroid hormone in the cells even in the face of thyroid gland damage.
This is how regulation occurs at the local level and may explain why patients with Hashimoto’s (even with thyroid gland damage) can still have relatively normal free T4 and free T3 levels in the serum.
I call this your thyroid reserve capacity or the ability of your body to utilize what little amount of thyroid hormone it has available.
And this phenomenon, shouldn’t be surprising because we know that other organ systems and tissues display similar behavior under stress or damage.
Your liver, for instance, can continue to function even in the face of over 50% damage to its cells.
Thyroid lab tests offer a way for us to potentially look into the cells and look into deiodinase activity.
Using thyroid lab tests such as Free T3, Free T4, Reverse T3, and TSH may help to provide insight into the function of these enzymes.
They won’t allow us to look at the tissue-specific activity (for instance, how well is your pituitary functioning vs. your heart and so on) but they can give us a general idea as to how they are functioning in the entire body.
We know from basic thyroid physiology, that in order for T4 to become activated it must be acted upon by either D1 or D2.
From there, T4 will lose an iodine moiety and be turned into free T3.
The more that this occurs we would expect that free T3 levels should increase while free T4 levels should decrease.
On the flip side, if T4 is acted upon by D3, we know that it will lose an iodine moiety but it will be converted into the inactive metabolite reverse T3.
We would, therefore, expect that in cases of conversion from T4 to reverse T3 that free T4 levels would be low-normal, free T3 would be low, and reverse T3 would be high.
The absolute values of these free hormones may not be as important as the change in the values over time or in the pattern that you see in your labs.
Thyroid lab patterns to look for:
- Increased D1 activity pattern = normal-high free t3, normal-low free t4, normal-low reverse T3
- Increased D2 activity pattern = normal-high free t3, normal-low free t4, normal-low reverse T3
- Increased D3 activity pattern = normal-low free t3, normal-low free t4, normal-high reverse T3
One way to evaluate the function of these enzymes is to compare your current results to whatever your ‘baseline’ lab results should be in an ideal scenario.
For best results, this would require that you have a baseline set of normal labs from when you were healthy to compare your current results.
If you don’t have a new set of labs then you can always monitor these thyroid lab tests as you change medication dosages and as your disease progresses or regressions (hopefully).
Deiodinase Polymorphisms & SNPs
Not only can certain medical conditions cause disruption to the function of deiodinase enzymes, but you can also experience problems simply by virtue of your genetics.
Many different SNPs have been associated with the presence of certain medical conditions (you can see the list below).
SNPs, which stand for single nucleotide polymorphisms, are tiny changes in your DNA and the presence of these SNPs have been used to determine your risk of developing certain medical conditions.
Genetic tests such as 23andme can show you if you have any of these SNP’s.
It’s important to understand, though, that the presence of the SNP doesn’t necessarily mean you will have the disease, but it certainly increases the likelihood that you will.
In the context of thyroid function, these SNPs seem to be associated with the function of deiodinase enzymes in certain tissues.
Most of the SNPs we are concerned with seem to impair the ability of your enzymes to function, and it may be this lack of function that has significant clinical importance.
For instance:
Certain SNP’s, such as rs225014, if present, may impact your ability to tolerate certain medications or utilize certain medications.
Studies have found that patients who have this specific SNP tend to do much better on a combination of T4 and T3 thyroid medication compared to T4 medication alone.
You can see a growing list of identified SNPs that may impact deiodinase function below:
- DIO2
- rs225014/rs12885300 (13) = associated with the development of osteoarthritis
- rs225010/rs225012 (14) = associated with mental retardation in iodine-deficient areas
- rs225014 (15) = associated with psychological well-being on T4 only medication
- rs225014 (16) = Preference for T3/T4 thyroid medication over T4 only medication
- rs225014 and rs225017 (17) = Increased risk of developing type II diabetes and worse blood sugar control with diabetes
- rs225014/rs12885300 (18) = associated with bipolar affective disorder
- rs225014 (19) = associated with hypertension/blood pressure
- DIO1
- rs11206244/rs12095080 (20) = associated with changes to IGF-1 levels
As we learn and understand more about these SNP’s I am confident that they will allow for a more personalized approach to thyroid management and may become an integral part of thyroid hormone management.
You can test these SNP’s right now, but the chances of your doctor understanding what to do with it may be slim.
Conclusion
Your deiodinase enzymes serve a very important purpose in maintaining thyroid function in both the entire body and at the cell level.
Dysfunction in these enzymes can occur in the presence of certain medical conditions and should be taken into account if you are not doing well with your current management.
The function of these enzymes may also help to explain why certain patients do better on T4-only thyroid medications and why others may benefit from combination treatment with LT4 and LT3.
Your genes may also play a role in how active (or inactive) these enzymes are.
Many different single nucleotide polymorphisms have been associated with the development of certain disease states.
You can identify the presence of these SNP’s through genetic testing.
From there you can use this information to help determine your treatment and be mindful of your risk for certain medical conditions.
Now I want to hear from you:
Do you suspect that you have deiodinase dysfunction in your body?
Are you doing well on your current medication?
Do you think your genes are playing a role in how you tolerate certain medications?
Leave your comments or questions below!
Scientific References
#1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3169863/
#2. https://academic.oup.com/edrv/article/23/1/38/2424136
#3. https://www.ncbi.nlm.nih.gov/gene/1733
#4. https://www.ncbi.nlm.nih.gov/gene/1734
#5. https://www.ncbi.nlm.nih.gov/gene/1735
#6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155120/
#7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155120/
#8. https://www.ncbi.nlm.nih.gov/pubmed/23296981
#9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5661015/
#10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2721352/
#11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3175696/
#12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4979226/
#13. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3937864/
#14. https://www.ncbi.nlm.nih.gov/pubmed/15286152
#15. https://www.ncbi.nlm.nih.gov/pubmed/19190113
#16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5527224/
#17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4126657/
#18. https://www.sciencedirect.com/science/article/pii/S0278584609001560?via%3Dihub
#19. https://www.ncbi.nlm.nih.gov/pubmed/17224473
#20. https://www.ncbi.nlm.nih.gov/pubmed/15483075/







Hi,
Is there anything I can do to improve the function of the D1, D2 and D3 enzymes?
Keren
Hi Karen,
I’m working on providing some more information on that topic in the future but you can get a basic improvement with some supplements, exercise, stress reduction and so on.
You can find some basic info here: https://www.restartmed.com/increase-free-t3-naturally/
And info on supplements here: https://www.restartmed.com/product/t3-conversion-booster/
Hi, I’m post-thyroidectomy and feel ill all the time! I have high TSH high free t4 yet low free t3 what does this mean?
Hi Alison,
I would check out this article for more information: https://www.restartmed.com/levothyroxine-thyroidectomy-patients/
I was diagnosed with non-functional thyroid twenty plus years ago, so have been on levothyroxine, with constant changing doses. Approximately 6 months ago I started on essential oils to try and get back to natural treatment. And I have, for many years, even with the thyroid replacement, had many other health issues, some including got flashes, extreme mood swings, severe depression, muscle/joint issues and other. So I took myself off all my antidepressants/anxiety meds and my thyroid supplement. Within a couple of weeks let’s say I felt so much better, and in an even keel. No ups and downs and a lot of other issues.
Two weeks ago had my yearly wellness check. Thyroid levels were 40,000 plus and liver enzymes were elevated. Dr. told me to start back on 125mg of Levi again, but since restarting I feel worse then I ever did. My joints hurt so bad I have a hard time walking, depression is off scales, with strong suicide thoughts, short of breath, breath-holding, I’m a mess. Tried taking meds different times, half twice a day but am going to stop taking it again. Please help me understand because I am feeling hopeless.
are you back on the anti-depressant drug(s)?? Almost all of the drugs in that entire drug class can and often do cause depression as a side effect as well as suicidal tendencies in some people.
Yes, the very thing that anti-depressents are intended to treat, (depression) also happens to be one of the side effects they can cause.
Kim, how are you doing now? What essential oils did you find helpful, I wonder?
So my Lpa is high, had genetic testing done and I carry the gene for LPA. Would taking Armour help me better with my hypothyroidism than NP Thyroid or would both meds be similar to one another?? Thanks.
Hi, I am someone who doesn’t convert hardly any t4 to t3. I have heard via Paul Robinson that TSH is essential in the production of DIO enzymes for conversion. But that even with a little bit of TSH most people still won’t convert as much via DIO 1 and 2 as they will just reverse t3 via DIO 3. Is it true that you need some TSH for production of these enzymes? And if so, would that leave us with t3 only therapy being the best option?
Please provide more I for plz. I am on a T4 plus cytomel combo. Trying to understand how much cytomel with doc that is needed as body very sensitive and seems I dont absorb my meds. Know am seeing functional med doc have seen improvement through food and supplements and labs looking better. Just trying to get a handle of the dosing.
Hi Christine,
More information on which part?
Thanks for this super informative post. I suspect I have an issue with D1, D2, and or D3.
I have been on every iteration of thyroid meds you can imagine over the decades, both synthetic and desiccated, T4 only, T3 only, synthetic T3 and T4, every brand of desiccated, etc. Recently, I have become intolerant of my meds. Actually it feels like my brain is actively rejecting them. Approximately 45 mins. after taking my meds (can be T3, T4 or desiccated), I get this huge pressure in my head (not pain) and bad brain fog and derealization to the point I can’t read or type or drive a car, etc. I feel very woozy. I also can’t remember what happened just hours before. (I’ve read about hyperthyroid amnesia.) Then if I wait to long to take more, I feel like I’m going to lose consciousness almost literally, like the life force is draining out of me. It’s like I go from hyper to hypo in a matter of hours. (I get that sounds super weird, and I get that different meds have different half lives, but that is my experience.)
It makes sense to me that something with the deiodinase is off. (I wonder if extreme stress of taking are of a dying parent could do it?) Any thoughts would be so greatly appreciated, including anyone who is knowledgeable that I might consult with. My doc knows this is going on, but it’s out of his purview.
Thanks again for all your hard work!
I hope you found some info. I think some of us can relate. If you are under stress, perhaps hydrocortisone can help?
I know exactly what you are referring to Syd. It’s such an awful and scary feeling (from Levo). In my novice understanding, I was sending myself into Thyrotoxicosis, which can be deadly. I am in a research study (unrelated to Hypothyroidism) in which they did Whole Exome Sequencing (Different from Whole Genome Sequencing). I highly recommend finding a genetic research study if you are writing on this site – I found by reading research papers and looking up the authors, and then calling them myself. A never before reported/novel SNP regarding DIO1 is appearing suspect, will require extended laboratory research to prove – as well as finding others who have the mutation and illness. More shall be revealed. I struggled with doctors and ordered some blood tests through an independent lab (went to the grocery store to have bld drawn, paid out of pocket). My Iodine and Zinc are low, my Selenium is high. I highly recommend getting those tested as they are intricately involved with the Thyroid, especially before blindly taking supplements. Iodine can also send you into Thyrotoxicosis, especially if one has been deficient for a very long time. I am in my 40’s, live in the US, only diagnosed this past year with Hypothyroidism (specifically Central Hypo with no Pituitary Adenoma) and it is believed that I have had this since birth. Insanity! At this point, I only take a very small dose of exogeneous (skin) Iodine (no t4 Levo or T3 Lio) and my Thyroid numbers have stabilized. I am absolutely leading my own recovery as doctors are at a loss. My main support comes through the doctors in the research study. I am not a doctor, but don’t just take Iodine without testing your numbers. Iodine and Levo together can be especially dangerous for some = Thyrotoxicosis = very bad. There are lots of research studies out there on DIO 1/2/3. As mentioned in this article and from the research I have read, certain environmental factors can help (depending on which Deiodinase is the issue) such as fasting/not fasting, temperatures/weather, hormones (such as melatonin, insulin, leptin – to avoid or or to take), glucose intake and nutritional states. The more people that can get in to genetic research studies, the more Physician Scientists will be able to learn and help people like us.
After decades of ill-health (since 1981!), difficulty getting diagnosed with hypothyroidism (blood tests said I was normal) but a good doctor diagnosed it anyway; still feeling less than well on T4; awful symptoms for years, tried T4 plus T3 and still not well. Eventually found a doctor about 15 years ago who prescribed T3 only. Eureka! It worked, and I was happy and well. Until two years ago, when I was diagnosed with heart failure and told to take beta blockers. My health deteriorated again and I found that ALL the ill-health involved symptoms of hypothyroidism! Even though my dose of T3 was right. Can you tell me if beta blockers disrupt thyroid function? If so, I would be beta blocker intolerant. Most cardiologists seem to make beta blockers compulsory. One I saw on youtube said that one in five of his patients are beta blocker intolerant, but he did not say what he prescribed instead. Can you help?
Hi Valerie,
Yes, beta blockers limit T4 to T3 conversion.
I am not taking T4, i have been taking T3 ONLY for many years.
And can you not tell me what drug can replace a beta blocker for a person who is beta blocker intolerant?
Beta blockers increase dio3 which can make t3 go to t2
Do you see patients who are homozygous for D2? I have tried every possible medication combo and can’t get better. I’m losing my life.
I have a normal TSH and slightly high T4 but my T3 is low. I cold all the time and always very tired (fatigue). I suspect that there is something with deiodinase. I have been suffering this for more than two and nobody can help. I have taking vitamin centrum every day and an extra selenium but tiredness still remains. I was treated with radiotherapy for 35 times in the neck and now I am taking Thyrax hormone (T4).
Your much needed help will be highly appreciated.
Thanks a lot,
Dominic Diaz
If you have a homozygous variant for DIO2 and perfectly fine DIO1, what do you do? Because t3 only means further stimulation of my DIO1 which help inactivate t3 to t2. Bit t4 works very little. I’m not able to be well on anything!
I’m confused. Does everyone have those SNPs? I see in my dna that I have rs225014 TT allele and rs11206244 CC allele. Also have rs2235544 CC which seems to be associated with more Dio1 activity and increased T3 ratio. Half my thyroid was taken out due to a rare hurthle cell adenoma and I can feel functional on levo but I need my FT4 levels to be elevated to get my T3 into 70% of the reference range. I don’t know how to read these SNPs but they seem to indicate I will do better on T4 only. I’ve been trying to add T3 onto my usual dose an not feeling good.
Thank you for your article, is very informative!
Could you clarify how to find if we have the gene mutations you mentioned? Should I simply search in my RAW DNA data for them? Is there a specific chromosome/allele that I should check for?
Also, for rs225014 you mentioned both psychological well-being on T4 only medication and Preference for T3/T4 thyroid medication over T4 only medication. Which one is correct? I seem to have this in my DNA report but I am doing better on T3 only so it would be good to know what the correct way to look at this data is?
Thanks!
Hi Sara,
Unfortunately, both are correct and that’s the problem when looking at genetic data. It’s only so helpful and should only be used as a guide and not a definitive treatment tool. Having a specific SNP shouldn’t solely guide treatment but it can suggest that you may do better on one treatment over another. If you are doing better on T3 only then I wouldn’t stress too much about it.
Hi Dr. Childs,
Thanks for writing on the subject of the “D” enzymes. I am curious… Has anyone created supplements for these enzymes? Why or why not? Or better said, could we create some and simply take them and solve the problem?
Hi Hadassah,
The best you can do is provide the body with the nutrients needed BY the enzymes. Even if you could take the enzymes by mouth there is no guarantee they would make it to the place needed to function.
I have taken 23 and me and although I can find DIO2 rs77075531 genotype which is C/C which I have read indicates the polymorphism but when I enter in rs225014 it says “not genotyped” do you have any recommendations?
Hello, just commenting that I’ve been reading your articles while going through hell with hypothyroid symptoms that have occurred throughout my life but got worse & combined in the past 12 yrs where I can’t function, hold a job, can’t return to schooling for a better job, etc. It’s terrible and I had to push my endo to test for T3, at which point they only ordered Total. My associated thyroid minerals are ok (zinc 72), D3 perpetually low but she thinks it’s just from the added weight. But when I lost weight in the past (was on metformin for pcos & levothyroxine at the time was still a struggle to lose 30lbs i had gained in short amount of time). Something isnt right, I was recently diagnosed with sleep apnea with symptoms since childhood. CPAP hasnt fixed my symptoms, only 2 or 3 specific things… I still pass out in my chair & sleep often. Nothing makes sense. My TSH, T4, Total T3 are low end of normal range. She tested my cortisol for Cushing’s but I don’t look like a Cushing’s person or have some of the telltale signs. Family history of thyroid… my aunt had hers removed after normal blood tests but extreme hyper symptoms and increasingly nodule saturated thyroid. IDK what is going on…
Hi Posh,
I would recommend comparing your lab tests results to the optimal ranges found here: https://www.restartmed.com/normal-thyroid-levels/
I’m on Armour.
TSH 2.6 (0.4-4.5)
T4, Free 1.0 (0.7-1.8)
T3, Free. 2.4 (2.0-4.4)
T3, Total 80 (80-200)
T3, Reverse 10 (8-25)
I recently added Iodine (Lugol’s Solution). Hoping helps with fatigue issues. Also curious about adding Relora.
Hi JJ,
Iodine can help but it typically only helps if you are deficient and replacing low levels. Taking high dose iodine when you don’t need it can sometimes cause issues: https://www.restartmed.com/high-dose-iodine/
Hi Dr Childs
I consume T3 and T4 but my TSH is suppressed although my intake is only 30mcg t3 and 50mcg t4.
I have got an early osteoporosis at age 40… I had Hashimotos. I was unable to function with T3 only.
Hi Sepi,
You may also want to look into other causes of bone loss such as estrogen levels.
Re: Thr92Ala Polymorphism (homozygous)
Why isn’t mono treatment with T3 (Cytomel; liothyronine) the treatment of choice? Thanks.
TST
Hi Terry,
Most likely because very few people even know they have that genetic polymorphism since it’s not standard to check/test for it. In addition, physicians are not as comfortable with T3 dosing as they are with T4 dosing so they will tend to lean towards what they know.
Hi doctor,
I’m researching what is going on with my body and found this. Interesting, thank you. My PCP wants me to do an MRI to look at pituitary/hypothalamus. For the last 10 years I have had extremely low TSH and T4. My T3 tends to be normal BUT I always took a combination T3/T4. I’m very active, tend to restrict calories, and am about 10-15 pounds overweight. I’m feeling fine (mild tiredness) on my medication now with T3 at the middle range and T4 at 0.9 (0.7 + range) but TSH at 0.002 and my doctor wants me to increase T4 but decrease T3 and thinks I might have pituitary/hypothalamus issue. Do you have any information on why my body won’t signal to create T4? Anything I can test for without the MRI (I don’t want the dye)? I am currently 44 and pretty good labs otherwise.
Hi Catherine,
One possible explanation is that calorie restriction has caused hypothalamic suppression. There are many other potential causes of pituitary/hypothalamic issues that can also be looked into.
Hi Thanks the such brief and rich Info. in a way any one would understand. I have a brother who had thyroid surgery results complete removal. he uses LEVOTHYROXINE SODIUM. But after his surgery 5 weeks now he feel very un usual fatigue like he can not even walk. he use to walk 5-6 miles a day . So in my opinion HE might had some T4-T3 conversion problem . since he lose energy to do any thing.
what is advice on this.
Thank you
Hi Amha,
Yes, it is very likely that your brother doesn’t convert T4 into T3 very well. I discuss why taking levothyroxine isn’t enough for most patients after thyroid removal in this article: https://www.restartmed.com/levothyroxine-thyroidectomy-patients/
Hi, Dr. Childs. I came across your website and it has educated me more than you know. I was diagnosed with Hashimoto’s ( which I believe I got first) after being diagnosed with Fibromyalgia and Celiac. I’ve maintained my body fairly well on Naturthroid and NP Thyroid , but they stopped working it seems. I’ve recently have had a huge flair up of what feels like inflammation and quick weight gain (30 pounds) after losing weight and maintaining for 5 years. I am gluten free, dairy free (dairy allergy) already. My physician and Endochronologist ( put me on Levothyroxine a month ago- ugh, dairy) do not agree on the process to help me and both believe I’m heavier due to lack of exercise and overeating. I’m frustrated, fatigued, fatter and fuming. I’m going to share some of your information with my physician, but I don’t know where else to start.
Hi Angela,
The single best thing you can do is find the right type of doctor to help. I would check out this resource for help: https://www.restartmed.com/how-to-find-a-doctor-to-treat-your-thyroid/
Have you noticed any connection between the Moderna Covid vaccines and the effect on the thyroid receptors? After taking my 2nd vaccine dose I had to eliminate the compounded T3 I was taking along with my Tirosint.The T3 caused nasty rashes after the vaccines. I also had to decrease my Tirosint dose. I now continue to have trouble keeping the thyroid in balance. I have Graves disease that was controlled 35 years ago with the Radioactive iodine and caused me to be hypothyroid.
How do thyroid hormone enzymes are involved in hyperthyroid conditions? How much I understand what happens is that person lacks enzymes that break down thyroid hormones, most likely because liver is overburdened and can’t make enough. What is your take on that, and possible solutions?