There’s no question that hypothyroidism is a complex disease but does it deserve the designation of chronic disease?
A chronic disease implies that you may never be able to 100% treat or manage your condition.
And I’m here to tell you that hypothyroidism should NOT be evaluated in this way.
Why is this important?
Because how you look at a disease influences the type of therapies that you will use for that disease and the type of outcome that you can expect after treatment.
What is Chronic Disease?
Put simply:
Chronic disease is a disease that is managed with the use of medication or other therapies but one that is never actually cured.
Chronic diseases include conditions such as hypertension (high blood pressure), high cholesterol, arthritis, type II diabetes, some intestinal issues, and so on.
When you are labeled as having a chronic disease it’s almost as if the doctor making that diagnosis says that this disease is NOT reversible but it can be managed.
Implicit in this logic is the idea that you will most likely suffer from some of the symptoms related to this disease off and on for the rest of your life.
As a patient reading this you probably aren’t thrilled about the idea of obtaining one of these disease states.
The good news is that most of the time chronic diseases can be managed with the right therapies and the right treatment.
I’m not talking about the therapies that your doctor is likely to prescribe, I’m talking about the obvious therapies such as dietary interventions, stress reduction, the right type of exercise, the right use of hormones/medications, and the use of supplements.
These ‘alternative’ therapies are often enough to reverse even the most difficult-to-treat conditions.
I have case studies on this very blog that show that type II diabetes can be reversed (and I’m not the only one (1)).
But you probably won’t find that your current doctor is willing to discuss these types of therapies with you (2).
Why?
Because it has to do with how doctors look at different diseases.
If you are conventionally trained (meaning you are seeing patients in the insurance model and you are used to using pharmaceutical drugs to treat anything and everything), then you are likely to only consider medications or surgery as the answer to any medical question.
If, however, you are more in tune with the research and have spent time practicing these alternative therapies on yourself and others, you will most likely be aware that these therapies are incredibly powerful (3).
It’s far more efficacious for a provider to spend 30 minutes talking 1 on 1 to a patient about diet than it is to see 3 patients for 10 minutes each and to only have time to manage a couple of their medications during that time.
But when was the last time that you had 30 minutes 1-on-1 with your doctor?
Probably never.
The current model of medical care doesn’t allow for that kind of time.
But why am I spending so much time on this topic?
Because it directly influences you if you have thyroid disease.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Is Hypothyroidism a Chronic Disease?
As I mentioned earlier, how you look at a disease will influence the type of therapies that you consider for patients and it also impacts the type of outcomes you are willing to accept during treatment.
Consider this example:
Let’s say that you have type II diabetes and you go to your doctor.
Your doctor has 1 of 2 choices regarding your treatment.
#1. He/she can attempt to reverse the disease using intensive dietary strategies while helping you alter your lifestyle with the hopes of reversing that condition and helping you to eliminate it from your body completely.
Or…
#2. He/she can give you a medication that lowers your blood sugar and follow up with you every 3 months (4) adding more medications as time goes on.
In the first example, your goal is to completely reverse the disease and you are expecting that the symptoms associated with this disease will someday be eliminated.
In the second example, your goal is to simply manage the disease with medications and you are accepting that you will probably suffer from the consequences of not only the medications you are using but also symptoms of the disease itself for the rest of your life.
As a patient, obviously, you would want to choose the first option but in order to pick that option, you must be aware of it in the first place.
And this exact same problem occurs with patients who have hypothyroidism.
Patients with hypothyroidism are often treated as if their thyroid is a medical condition that they will live with for the rest of their lives.
They are often, either explicitly or implicitly, that they are going to have to suffer from some of the symptoms of hypothyroidism for the rest of their life.
That might mean anything from fatigue to weight gain to depression.
But is this actually true?
It all depends on how you look at hypothyroidism and which box you put it into.
But hypothyroidism should NOT be considered a chronic disease because it is something that can be 100% managed if done correctly.
Hypothyroidism is simply a state of thyroid function in your body.
If you have low thyroid hormone in circulation then you are said to be in a state of low thyroid function and in a state of hypothyroidism.
But you can completely replace the lost thyroid hormone in your body with the use of thyroid medication and other therapies.
If you replace this lost thyroid hormone 100% then you should NOT continue to experience any of the symptoms of hypothyroidism.

This is different from “curing” the condition of hypothyroidism as that may not be possible in all individuals.
Instead, what you are doing, is attempting to replace this lost amount of thyroid hormone that your body is no longer able to produce.
Let’s say that you have the autoimmune condition Hashimoto’s thyroiditis which has partially damaged your thyroid gland.
In this example, let’s say that your thyroid is functioning at 70% of normal.
In this case, when using thyroid medication, we would be trying to account for that lost 30% with thyroid medication.
So if the thyroid medication you are taking accounts for that lost 30% and your body is still producing 70% then you would be back at 100%.
And, really, this should be the goal for all patients who have thyroid-related issues.
And it should also be the goal of doctors who are treating these patients.
But there is one problem:
The current treatment paradigm and standard of care do not allow for the individualized care necessary to get to 100%.
To give you an idea of how deep this dogma runs, you can look directly at the mayo clinic website which states that “synthetic thyroid medications contain thyroxine only, and the triiodothyronine your body needs is derived from the thyroxine” (5).
This runs in direct contradiction to studies that show that T4-only thyroid medication is not sufficient to bring free thyroid hormone levels into the ‘normal’ range (6).
So, drawing from the example above, instead of replacing 30% of thyroid hormone with thyroid medication, you might only be replacing 10%.
Instead of getting to 100%, you may only be getting to 80% or less!
The Current Standard of Care for Treating Hypothyroidism
So what is the problem? Why do so many thyroid patients continue to struggle with thyroid-related symptoms even though they could potentially be feeling much better?
The answer is actually quite simple:
It has to do with the current standard of care and the current treatment paradigm.
This standard of care defines how ALL doctors should be treating a particular medical condition.
And anyone who deviates from this standard of care is potentially put at risk of disciplinary action.
This is both a good and a bad thing.
Good in the sense that it protects the public from doctors who are using untested therapies but bad in the sense that it slows down the progress and the changes in the development of certain medical conditions and therapies.
Right now, the current standard of care for treating thyroid-related conditions is set in stone and isn’t likely to change even though there are many signs pointing to the fact that there may be better options available.
What is this standard of care?
You’ve probably already encountered it, especially if you’ve been to a doctor who manages your thyroid.
Believe it or not, I can explain this standard of care in just a few sentences:
- Diagnose hypothyroidism on the basis of the TSH. An elevated TSH is an indication of hypothyroidism.
- If the TSH is > 5.0 then initiate therapy with Synthroid or levothyroxine.
- Recheck the TSH while taking these medications.
- If the TSH is > 2.0 then increase thyroid dose, if the TSH is < 1.0 then reduce the dose of thyroid medication.
- Rinse and repeat.
That is 98% of the treatment paradigm in just a few sentences.
This algorithm has reduced the complexity of the thyroid system down to a few simple steps.
While these steps are great for the doctor (because they are easy to follow) they are not good for the patient and have contributed to the growing dissatisfaction that many thyroid patients are experiencing.
Take this recent poll of 840 thyroid patients (7), for instance, which showed that only 6 percent of thyroid patients feel satisfied with their treatment whereas 1 in 5 feels completely unsatisfied.
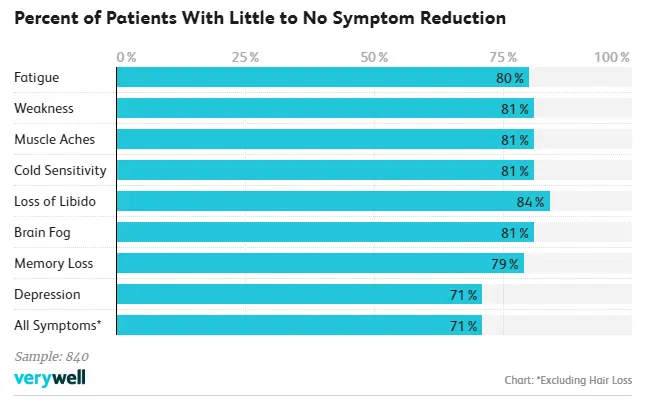
You wouldn’t see these levels of dissatisfaction if their treatment was considered adequate.
A New (and Better) Approach to Thyroid Management
If that approach isn’t the best, then what is?
I’ve found that the best way to approach thyroid management includes all of the following:
- Look at each patient as an individual.
- Diagnose hypothyroidism by evaluating the complete array of thyroid serum lab tests available: TSH, free T3, total t3, free T4, reverse T3, and thyroid antibodies.
- Use a combination of T4 and T3 thyroid hormones in ratios that mimic normal thyroid function in healthy individuals.
- Consider the genetic variances among individuals and how these genetics impact the needs of thyroid hormones and the dose of thyroid medication that this person needs.
- Attempt to naturally improve thyroid function as much as possible through the use of lifestyle changes and therapies.
- Use the combination of thyroid lab tests and patient symptoms to help with dosing thyroid medication.
- Understand that each patient will be different and no two treatment regimens will be the same.
As you follow this outline there is more room for patient variability and it becomes possible to shift the way we look at thyroid disease and management.
Instead of just looking at hypothyroidism as a chronic disease that will never fully be “treated”, patients can instead take back their lives and begin to live comfortably.
The question is, does this approach really work?
And the answer that I would give you is yes.
In fact, I’ve treated hundreds of patients with this very approach with great success and you can read more about their success stories here.
In addition to being tested on hundreds of patients, you can also find all of the research to back up these claims and others that I make on my blog in posts such as these.
Why Thyroid Medication Isn’t the Only Answer
I’ve spent a lot of time talking about using the right type and dosing of thyroid medication to help supplement whatever thyroid hormone your body is capable of making.
But this isn’t the only variable that should be considered.
The other, very important variable, is that of your innate thyroid function.
Meaning, how well is your thyroid actually producing thyroid hormone?
You should ALWAYS evaluate this problem and separate it from the problem of using the right type and dose of thyroid medication.
Why is this the case?
Because your innate thyroid function influences how much thyroid hormone you can potentially make.
Because of this, it’s very important for you to put effort and energy into assessing if there is anything that is potentially reversible which is negatively influencing thyroid function in your body.
If there is, then you can easily address that problem and potentially improve thyroid function.
This is also one of the ways that some people find a complete cure for their thyroid problem.
If the issue that is causing you to not produce enough thyroid hormone is reversible, then once you fix that problem your thyroid function may return to 100% normal.
But please note, however, that this is not always possible.
Some of you will have impaired thyroid function which is NOT reversible through any known medical interventions at this time.
A Word for Thyroidectomy Patients
The information presented here primarily applies to those people who have at least some thyroid function available to them.
This means that if you do NOT have a thyroid, or if it’s been damaged from radioactive iodine, then the information does not apply to your situation 100%.
Unfortunately, once the thyroid has been removed or completely damaged you are 100% reliant upon thyroid medication for the rest of your life.
It also means that you do not have any assistance from your normal thyroid gland.
Even though you can take thyroid hormone medication to replace your lost thyroid hormone, it’s very difficult to match the same quantity of thyroid hormone produced by your thyroid with the use of oral medication.
You can get close, close as in 80-90% of normal, but it is not realistic to expect that you can get back to 100% while taking thyroid medication.
There are too many variables at play including dosage, the frequency with which you take your medication, and so on.
All of these factors influence how well you will feel on thyroid medication.
It’s not that you can’t see improvement, because you can, but you should reduce your expectation from getting 100% better down to 80-90% better as a best-case scenario.
Conclusion
It’s best for you as a patient to NOT consider hypothyroidism as a chronic disease.
Instead, consider hypothyroidism as a disease that can be 100% managed with the use of thoughtful therapies.
These therapies, including thyroid medication and lifestyle intervention, can help bring your thyroid function back to 100% normal which should eliminate any negative symptoms that you may be experiencing.
Do not accept hypothyroid symptoms as part of your new ‘normal’.
Experiencing the symptoms of hypothyroidism such as fatigue, weight gain, constipation, cold intolerance, and hair loss are all indications that your thyroid is not optimized.
As you get closer and closer to 100% of normal thyroid function you should find that all of these symptoms subside.
Now I want to hear from you:
Are you currently treating your hypothyroidism as a chronic disease?
How close to 100% of normal are you?
What therapies are you using to help you get there?
Have you tried the personalized approach that I mentioned above?
Leave your questions or comments below!