The answer is yes!
But what I find in most patients is that the underlying cause of high blood sugar is typically not the thyroid.
Even though thyroid function can play a role, it’s usually other underlying conditions such as how much stress you are under, how much thyroid medication you are taking, what types of foods you are eating, how much inflammation is in your body, and more, contributing the most.
The good news is that managing your blood sugar if you have hypothyroidism is possible.
The bad news is that it may take a little more work compared to someone that doesn’t have thyroid problems which is exactly what we are going to be discussing today.
In this article, you will learn:
- The connection between insulin resistance and hypothyroidism
- The connection between blood sugar and insulin levels
- How insulin impacts your weight
- How to treat insulin resistance if you have hypothyroidism
- And much more
Let’s jump in…
High Blood Sugar Stems from Insulin Resistance (& Sugar Consumption)
Treating high blood sugar is incredibly important from an overall health perspective but also from a weight loss perspective.
Why?
Because the fact that you have high blood sugar is usually a sign of something known as insulin resistance.
You’ve probably heard of insulin in the past but perhaps you didn’t really understand its significance.
So what exactly is insulin?
Insulin is a hormone secreted by your pancreas typically in response to food (1) but stress can also stimulate it.

Your body produces insulin after you eat a carbohydrate-rich meal because it wants to utilize the energy you just consumed.
Insulin acts to take that sugar and push it into your cells thereby storing it for later.
And this is a good thing, usually.
Insulin is just a hormone doing its job but, under the right circumstances, can become dysregulated (2) that’s when it becomes an issue.
This is why understanding the distinction between the hormone insulin and insulin resistance is important.
Insulin resistance is a state of cellular resistance to insulin that occurs in response to repetitive and repeated carbohydrate (sugar) intake.
And that’s when things start to become a problem.
As your body becomes resistant to insulin, your blood sugar will rise (3) because your body has a harder time putting inside of your cells.
This leaves extra sugar floating around in your bloodstream instead of inside your cells where your body wants to put it.
This blood sugar starts to bind to things in your body including your red blood cells (this is where the hemoglobin A1C test comes in) and can even damage organs and tissues (such as your kidneys and eyes).
Insulin resistance is actually quite common, especially among hypothyroid patients.
The incidence of insulin resistance is estimated to be around 50% (4) of the adult population in the United States.
Among hypothyroid patients, this percentage is likely far higher given the connection between your thyroid and insulin levels.
Hypothyroidism and Blood Sugar
It turns out that your thyroid is actually a potent modulator of both insulin and glucose (sugar) metabolism (5).
What does that mean?
It means that if there is something wrong with your thyroid function then it will almost always affect your blood sugar (6) in some way.
This effect occurs independently of other factors which may trigger insulin resistance (such as stress or sugar consumption).
What this means is that patients with thyroid disease, of any type, are at higher risk of developing insulin resistance because of their thyroid condition.
And I find this to be true.
It’s rare that I see someone with hypothyroidism who doesn’t also have insulin resistance (this also applies to hyperthyroid patients (7), by the way).
It is likely the case that at least some amount of insulin resistance was present before the diagnosis of hypothyroidism in most people but that insulin resistance was then made worse by the added thyroid problem.
Thyroid hormone, under normal conditions, is supposed to act to help your body get rid of excess sugar inside of your cells.
In this way, it opposes the action of insulin.
The interplay of thyroid hormone and insulin/blood sugar is actually more complex than that (8), but this serves to drive home the point.
If there is an issue in thyroid status (meaning that your thyroid levels are abnormal) then it will always affect your blood sugar and insulin receptor sensitivity to some degree.
It’s best to think of the connection between thyroid function and blood sugar as a balance.
If thyroid hormone is too low then it will result in high blood sugar and insulin resistance.
On the flip side, if thyroid hormone is too high then it will also result in insulin resistance and high blood sugar.
You want your thyroid status to be just right in order to balance blood sugar.
This also means that patients with hypothyroidism or low thyroid function are at a distinct disadvantage when compared to other healthy people when trying to treat insulin resistance.
Why?
Because the current treatment paradigm for hypothyroidism may leave up to 20% of thyroid patients ‘undertreated’.
You will know if you fit into this category because you are likely already taking thyroid medication but still experiencing low thyroid symptoms.
You can also fit into this category if you have a normal TSH but low circulating free thyroid hormones such as free T4 and free T3.
In either case, the result is the same, you do not have sufficient thyroid hormone in your body to balance the effect of insulin.
This means that treating insulin resistance and losing weight will always be more difficult for thyroid patients unless their thyroid medication dose is optimized.
You can also obtain thyroid optimization through the use of natural thyroid remedies so don’t think you necessarily have to use medication to get there.
Regardless of the situation, though, your goal should be to obtain 100% thyroid optimization to make treating insulin resistance easier.
Does Thyroid Medication Worsen or Treat Insulin Resistance?
It is well known that there is a connection between the thyroid and blood sugar which is why thyroid patients often ask how thyroid medication fits into this equation.
After all, thyroid medication contains active thyroid hormone and, therefore, will impact blood sugar levels when taken.
How your thyroid medication impacts blood sugar depends on many factors, though, and is not as straightforward as you might think.
First of all, how much thyroid medication you are taking is very important.
What do I mean?
How well are you being dosed?
Is your dose allowing you to obtain 100% normal thyroid function? Are you taking too much thyroid hormone? Or are you taking too little thyroid hormone?
When doctors prescribe thyroid medication they try to get you as close to normal as possible but this rarely happens.
Instead, it’s not uncommon for thyroid patients to experience bouts of high thyroid function and low thyroid function as they try to adjust their dose.
These ups and downs in thyroid dosing obviously will impact insulin and blood sugar levels.
Because of this, it’s possible for thyroid medication to make insulin resistance (and blood sugar) worse but it’s also possible for thyroid medication to improve your blood sugar.
It all depends on your dose.

If you take too much thyroid medication, in any form, and you become hyperthyroid, then you may raise your blood sugar and make insulin resistance worse.
As insulin resistance worsens, you may also find that you gain weight!
This doesn’t always make sense to thyroid patients because they often want to increase their dose because they want to try to lose more weight.
But it doesn’t always work out that way.
Sometimes taking too much thyroid hormone can lead to weight gain. It’s rare but it does occur.
On the flip side, not taking enough thyroid hormone can also lead to insulin resistance and weight gain.
Being underdosed is typically more common than being overdosed though but it is not uncommon for some patients to be both underdosed and overdosed at various times during their treatment.
Being underdosed generally leads to persistently high blood sugar (and insulin resistance (9)) and the inability to lose weight.
When it comes to being underdosed, the right type of thyroid medication can often make all of the difference.
Often this means using a combination of both T4 and T3 thyroid medications instead of just isolated T4 like levothyroxine.
Medications such as Cytomel and Armour thyroid, for instance, contain the more active thyroid hormone T3.
Using these medications provide more oomph to your thyroid medication dose and may make all of the difference in both how you feel and how well your thyroid is managed.
Cortisol, Blood Sugar & Thyroid Function
The connection between your thyroid and blood sugar goes even deeper than what we’ve discussed so far.
Going deeper, we also see a connection between thyroid function, stress, and blood sugar.
Before we talk about this, let’s do a quick recap of what we’ve already discussed:
So far we know that both hypothyroid and hyperthyroid states can lead to high blood sugar.
We also know that medications that impact thyroid hormone levels can also impact blood sugar.
Thyroid medications such as levothyroxine or Cytomel must be dosed correctly if you want to have normal blood sugar.
Antithyroid medications like methimazole can also result in insulin resistance and high blood sugar due to their impact on thyroid function.
Any medication which impacts your thyroid will have an impact on your blood sugar. Period.
The degree of that impact will depend on the dose and therapeutic strength of the medication you are taking.
But there’s another factor that can impact blood sugar in hypothyroid patients as well.
And that is cortisol.
We know that there is a strong connection between thyroid function and cortisol levels.
Physiologic studies have shown that as cortisol rises it also tends to bring up TSH levels (10).
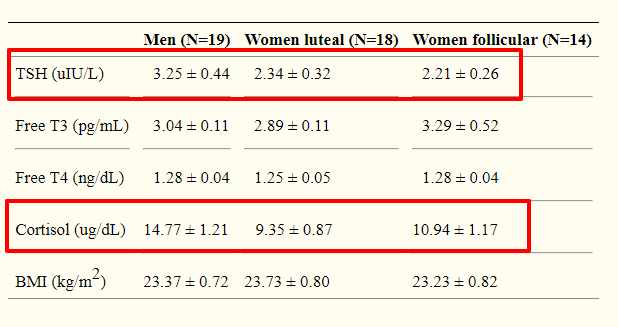
For those who may not understand the TSH lab test, a rising TSH is an indication of low thyroid function or hypothyroidism.
In other words, high cortisol causes low thyroid function.
So now we have a system that looks like this:
Stress causes decreased thyroid function which causes increased insulin resistance which causes increased blood sugar which causes weight gain and weight loss resistance.
And it doesn’t stop there.
We also know that stress by itself causes the release of blood sugar and excess stress can lead to insulin resistance on its own (11).
Because of this, it’s probably more important for you to manage stress than it is to focus on your thyroid if you have a thyroid problem.
Focusing on your stress and cortisol levels will impact both thyroid function and blood sugar and give you more bang for your buck.
Excessive stress tends to lead to issues with cortisol levels (which can be tested for, by the way) and typically manifests as increased belly fat.
In contrast, the weight gain for decreased thyroid function tends to be uniform over the entire body.
The distribution of weight gain in your body can sometimes provide valuable information about the status of your hormones.
The bottom line?
Because of the connection between cortisol, thyroid, and insulin resistance, you should always make sure to test your cortisol if you have any sort of thyroid problem.
Addressing stress and cortisol will allow you to influence your weight, thyroid, and blood sugar levels simultaneously.
The Impact of your Diet on Blood Sugar
Another area that is worth going into more detail is diet and its impact on blood sugar.
I touched on this in the very beginning but we will revisit it here.
When most people think about high blood sugar they often think immediately of the food that they put in their mouth (12).
It just makes sense that if you eat a lot of sugar, you will see that consumption of sugar is reflected in your blood and body.
Imagine consuming a 44-ounce big gulp of Coke or Pepsi loaded with high fructose corn syrup.
All of that sugar is going to be rapidly absorbed into your body and trigger the release of insulin, as we’ve discussed previously.
This example makes a lot of sense because we are talking about rapidly absorbed sugars in liquids.
But there are other foods that are high in sugar that can stimulate the same response.
Starchy foods, potatoes, fruits, etc. can all be absorbed and stimulate the insulin response as well.
The main difference between these foods and the big gulp example is the rate of absorption and how this rate impacts the rise of insulin levels from the pancreas (13).
Because of this, healthy whole foods are nowhere near as stimulatory to insulin as foods with added sugars such as those in the big gulp example.
Having said that, it is still possible to consume too much of a good thing even whole foods.
Excessive consumption of whole foods high in sugar, especially when combined with high fats, can exacerbate and contribute to insulin resistance.
I’ve found that it’s generally safe for most people to consume whole foods which are high in ‘sugar’ if they aren’t also consuming them with fatty foods (even healthy fats (14)).
Proteins have also been shown to stimulate the insulin response.
The only macromolecule which has the smallest impact on insulin by itself is fat.
Because of this, many doctors and providers have started recommending diets that are very high in fat as a treatment for high blood sugar and insulin resistance.
In fact, you’ve probably tried these diets before if you’ve been on the ketogenic diet or the carnivore diet which happen to be popular at the time of this writing.
Even though this approach makes logical sense, there’s one big problem:
It doesn’t always work!
There are plenty of people who go on ketogenic diets and high fat & low carbohydrate diets and yet they still struggle with high blood sugar and weight gain.
This just highlights the fact that we need to better understand the relationship between blood sugar and insulin.
The ketogenic diet, for instance, may have a suppressive effect on thyroid function which may counteract the benefits of this type of diet in some people.
My opinion is that there are other factors outside of just your diet that contribute to weight gain and insulin resistance such as subclinical thyroid dysfunction and cortisol dysregulation (as we’ve discussed above).
Treating Insulin Resistance if you have Hypothyroidism
So, what are you supposed to do if you have high blood sugar and hypothyroidism and you want to treat it?
What if you want to treat insulin resistance to help you lose weight?
There are several strategies that you can take and I’ve listed several below:
- Optimize your thyroid medication – What I mean here is that you need to make sure that your thyroid medication is optimized for your body. For most of you, that means you will probably need to take more medication than you are taking right now. For some that may mean lowering your dose. When optimizing your medication for blood sugar, you’ll want to focus less on the TSH and more on your free thyroid hormones (free T3 and free t4). As you optimize both of these numbers you will probably find that your blood sugar will drop naturally (as well as your weight). Avoid increasing these numbers outside of the reference range while trying to optimize them in the top percentile of the “normal” range. You can learn more about this concept here.
- Take insulin-sensitizing supplements – There are several supplements (which are available over the counter) that you can take in conjunction with all of the therapies I’ve listed here, that can help improve your blood sugar. Some of my favorites include Berberine, fish oil, Alpha lipoic acid, glucomannan, and chromium. These supplements all have scientific studies which show that they are effective at reducing both blood sugar and insulin resistance. And the best part is that they can be taken or used in conjunction with medications and other lifestyle modifications.
- Take insulin-sensitizing medications – If you really want to kick things up a notch you can also try the use of insulin-sensitizing medications. These medications are particularly useful if you are struggling with weight loss resistance which you believe is secondary to insulin resistance/high blood sugar. These medications can be used temporarily (to reverse the condition) and don’t necessarily have to be taken long-term for you to realize their benefits. Medications that fit into this category include Victoza, Saxenda, SGLT-2 inhibitors, and metformin. There are others, but these should serve as a good starting point. Victoza and Saxenda are quite expensive if insurance doesn’t cover them while metformin is incredibly cheap at around $4.00 per month. The downside to using Metformin is that it’s not quite as effective as the others, but it’s a great medication to use in many people. Metformin (and the others) can also be used in conjunction with supplements with may enhance their potency and effects!
- Exercise correctly – We didn’t talk much about exercise in this post, but it’s certainly an important aspect if you are trying to lower your blood sugar. Exercises that put a temporary high strain on the body over a short period of time tend to be best at improving insulin sensitivity. Exercises that fit into the high-intensity interval training spectrum are often ideal. The good news is that you don’t need to spend hours on a treadmill but the bad news is you will need to push yourself to get results.
- Clean up your diet – Another thing you’ll want to do no matter which therapies you use is adjust your diet. Taking all the supplements, medications, and thyroid hormones in the world will not be enough to counteract the negative effects of a bad diet. Most people know what ‘healthy’ foods are, they just have a hard time sticking to them. For those who aren’t sure where to start, look at diets that are high in real, whole foods. From there you can then start to tweak macromolecules such as protein, carbohydrates, and fats as needed.
- Consider other medications such as LDN – Lastly, some other medications can also be used to help sensitive your body to insulin. Medications like LDN (low dose naltrexone) can also potentially help autoimmune disease states such as Hashimoto’s thyroiditis (a major cause of hypothyroidism). These medications are often prescribed off-label though, so you may need a willing physician to help you out.
As you consider these therapies keep in mind that the more therapies you add on top of each other the more likely you are to see your desired results.
That means you’ll want to simultaneously change your diet, take the right supplements, adjust your thyroid medication, exercise with enough intensity, and consider the use of medications for the best results.
Final Thoughts
While it is true that hypothyroidism can lead to high blood sugar, the connection between the two is not just that simple.
There is a range of competing factors that can also contribute to high blood sugar in hypothyroid patients which should be evaluated and addressed.
The good news is that you can lower your blood sugar by taking several steps such as adjusting your thyroid medication, taking supplements, and improving your lifestyle.
Lastly, never forget the connection between stress, your thyroid, and your blood sugar.
Many people out there right now are probably suffering from a combination of all 3 while not even realizing it.
If you haven’t already, I would encourage you to look at adrenal adaptogens as a treatment for stress management.
These adaptogens have the potential to improve your energy levels, improve thyroid function, and help improve other hormone systems in your body.
I have yet to meet a thyroid patient that didn’t need them!
Now I want to hear from you:
Do you have hypothyroidism?
Do you also have high blood sugar?
What have you done to try and treat this problem? Did it work?
Do you feel that stress is contributing to your situation?
Are you planning on trying any of the treatments listed above?
Leave your comments or questions below!





When is the best time to do Lab draws? Take or do not take my thyroid (Amour) before the blood draw? How much time between blood draw and ingestion of thyroid meds? Thank you.
Hi Judy,
Typically you want to get your labs drawn right before you would normally take your medication in the morning.
If you are on T3 or Ndt you do your lab 12-17 hours after the last dose.
I would take a look at this post for more info on that topic: https://www.restartmed.com/thyroid-testing/
Hello Dr Childs,
I have Hashimotos disease (looking at my blood test results I think I have had an underactive thyroid for over 20 years)/ I started to put on weight when I turned 40 and have looked at my blood test results from that time and TSH was 3.8 (range then 0.3-5.0) and T4 was 11 (range then 9.0-24.0). It became Hashimoto’s when my mother and my husband died within 6 months of each other (although as antibodies were never tested, I will never know). It was extremely difficult time, battling the NHS for over 6 months for my mother who was profoundly deaf and also looking after my husband who died within 3 months of being told he had terminal bowel cancer.
I believed at that time that I have adrenal fatigue, but was dismissed by endos, who had no idea what I had been through and didn’t really want to know. I have been on levothyroxine for almost 7 years since the Hashi’s diagnosis. Over this past year HbA1c has now increased over this past year to 47 (1 point short of being diagnosed as T2 diabetic). My blood pressure has increased too, although my heart rate has always been in the 50s/60s (very occasionally in the 70s) and my basal temps are low too.
My TSH has always been low on levo and I’m always being told I’m over medicated – I’m most certainly not.TRH test was done with no response and I had an MRI scan of pituitary which they said was normal – they don’t know why TRH didn’t respond.
Earlier this year after being on 150mcgs of levo and still having extreme fatigue and difficulty losing weight, I was finally prescribed T3 to be added to my levo of 150mcgs (was told to reduce to 100mcgs). I did this and initially saw a slight improvement in fatigue, but in the meantime, I did the genetic test for DIO2 and found out I am heterozygous for DIO2. The endo said I could increase T3 to 30mcgs. I did this and immediately put on nearly 1 stone in weight in a month and started to experience edema (pitting of the skin).
I came off all meds for 10 days and had a blood test. My TSH raised to 9.7 (proving that there is no problem with my pituitary). I started on levo and gradually raised it back to 100mcgs and then added T3 in first 10mcgs and then raised to 20mcgs. Through following a very low calorie diet, I have managed to lose the extra weight I gained on the T3 increase, although it took me a month to do it. My endo said I could increase levo to 125mcgs and I have kept T3 at 20mcgs. He actually admitted that TSH is irrelevant when on T3 and that I am one of the 20% who still struggle when my bloods are in “normal” range and that I would probably feel better at the top end of range for T4 and T3 (I did manage to lose 3 stone when I was top end of normal), but I was left with no endo support for a year and as my thyroid continued to falter, my meds were not increased and so I gained all the weight back as well as becoming increasingly hypothyroid. At my last appointment in October, the endo suggested that I medicate to how I feel!! I do feel a little better on the newest dose, however, I am scared to raise the T3 as I’m worried about edema and weight gain again (which would of course increase my blood sugar and blood pressure).
No one seems concerned about my weight, my GP shrugs his shoulders and says it’s your thyroid. He’s admitted he doesn’t know how to treat hormones. I have resisted going on meds for my high blood pressure, but I’ve had a letter from my GP following my last blood test which shows HbA1c of 47 and I think they’re going to suggest medication.
I also have Thyroid Eye Disease(for almost 3 years) and have proptosis in right eye and lid lag in left eye. They were extremely concerned about my eye pressures but they have reduced a little with special overnight eye drops. The hospital say that TED is now inactive and that I can be scheduled to have an operation on lid lag eye.
Since my Hashi’s diagnosis in 2012, I have calculated that I have seen 14 endos/nurse practitioners (excluding GPs and eye specialists) and I seem to be collecting other issues along the way.
The upshot is I am about 4 stones overweight, have unmedicated high blood pressure and unmedicated pre-diabetes.
I have also been diagnosed with a small posterior fossa meningioma (discovered at the MRI for my TED) for which I amon watch and wait. I have Dupytren’s contracture following a broken wrist. The good news is that the osteopenia diagnosed from a DEXA scan at the end of 2015, has reversed at my last scan in May and I now no longer have osteopenia. My spine is normal and my hips are low, but normal.
I would add that I am post-menopausal.
My last bloods were TSH <0.05 (0.5-5.0), FT4 14.2 (10.0-22.0) FT3 5.3 (3.6-6.4).
I firmly believe that my hormones are severely unbalanced, and this is the reason for my continuing symptoms and issues but no-one seems interested in this and the medics seem unable to help me to balance them.
Any help you could offer would be much appreciated.
Thank you.
Hi Rita,
Your best bet is to find a physician who can really dig into your history to help figure out what is going on. My process, which typically takes about an hour, includes a comprehensive history and extensive lab testing. You can find resources on how to find a doctor to help you here: https://www.restartmed.com/thyroid-doctor/
Great article Doc yes both my wife and I are having huge struggle with weight since our thytoiddectomy hers cancer mine graves. She is also struggling with diabetes for me it’s high weight gain. I’m on nature Throid now 3 months it’s hard to find keep having to juggle the script for what’s available. Liked you idea of splitting the dose and that would help the availability nonsense. I am on 2.5 gr it’s easy to get the lower dose 1.5 gr evening and 1 gr in am. I am going to get your thyroid supplements keep the info coming. It’s hard coping without this amazing gland.
Hi Thomas,
It sounds like you are on the right track! Make sure you also do the other therapies listed in this article.
Hello. You mention over-exercising. What are the symtpoms, or how do I know if I’m over exercising? I’m a third-degree black belt in Shaolin kung-fu, and twice a week, I help teach a kid’s kung-fu class, then do tai-chi, then do black belt material. For two days following, I can barely move from muscle cramps and fatigue, and I’m exhausted. Two other days a week, I do yoga/mobility. Am I taxing my body too far? Background: I had a total thyroidectomy in 2009 (papillary cancer), and a recurrence of cancer in my lymph nodes in 2015. Current labs: TSH 3.43; T3 1.193; T4 .44. Thanks so much. Love your site, it’s very informative!
Hi Tara,
I would check out this article which goes into more detail about over exercising: https://www.restartmed.com/exercise-thyroid-problems/
Forgot to mention–I was diagnosed with insulin resistance 25 years ago, and currently have high blood sugars as well. Thanks.
Dr. Childs,
Thank you so much for the information that you share. I’m still learning and you are a wealth of knowledge on this subject.
I believe that I have been hypothyroid since birth, but wasn’t diagnosed until age 7, when the doctor said that about half of my thyroid gland did not function. I’m now 60 and currently taking NP thyroid, 4 grains (240 mg). (was on Armour for years before they went outrageously expensive). I’ve always had difficulty losing weight. I also have type 2 diabetes and am having trouble getting my blood sugar down, even when I went totally off of starches and sugars. I even had a bout of depression a few weeks ago, after about a week of eating good quality protein, non-starchy vegetables, and good oils. I was crying at work on and off one day at work, and didn’t know what was causing it. Is it possible that the lack of carbs was causing my thyroid to slow down, which caused the depression? I gave in that evening and ate something with sugar in it, and the depression stopped. It hasn’t come back since then when I started eating one fruit a day. This is a juggling act with me having both of these conditions. A ketogenic diet simply doesn’t work for me. I will stall if I eat too much fat, and get tired and depressed from eating too few carbs. Then I’m told…. don’t go too low on your calories, yet I lose very slow even on a 1200 calorie diet. The only time I’ve lost consistently was on a very low calorie diet, but was balanced. Can you give me any suggestions? Thanks for reading this.
Hi Catherine,
I’m not quite sure what your main question is, but if weight loss is your primary goal then I would urge you to check out these resources:
https://www.restartmed.com/hormone-mastery/
https://www.restartmed.com/lose-weight-hypothyroidism/
https://www.restartmed.com/calories-hypothyroidism/
There are many other resources available on my blog as well to help with that issue and others.
Thank you very much for this article. I have been experiencing very bad morning headaches as I have increased my T3 dose. My fasting blood sugar is 6.6 and I eat basically no sugar and very limited refined carbs. Your article provides a potential explanation and I’m very grateful for this. What I’m not totally sure of is how low cortisol can impact blood sugar? Is the effect the same as high cortisol???
I have been Type 1 for a little less than a year. My TSH levels are now starting to creep up. I am now 5.4 for my TSH and have gained 6-7 pounds. My doctor says he doesn’t treat TSH until it gets to 10. However, I now have changed my Lantus dose from 10 to 11 because, for some reason, my sugars have crept up (and I exercise daily and eat well). He said to come back next year. Should I get a second opinion? I’m training for a 10K next month and will be running a LOT and hiking, so I am thinking this will help a lot of my problems. What do you think?
I am 26 weeks pregnant and have been diagnosed with hypothyroidism since 3 months of pregnancy. The doc has since given me medications and now increased till 87.5 mg from 67.5mg as I had 3.87 TSH in my last test. Soon I started taking increased dose my blood sugar has spiked even if I eat healthy meal without carbs. The doc says I should not exercise and be on bed rest. Any suggestions what to do? How can I control my blood sugar as I am already cutting on foods and how to manage thyroid hormone. Help!! my baby is starving!
I love reading your information .You explain things in a clear way. I have hypothyroidism due to RAI treatment which wasn’t needed , I have hypoglycemia. I eat 3 meals carbohydrates and protein and also eat in between the meals. I have no weight problems so far. I have high cortisol all 4 points. I am on T3 only 33 mg (I cut the pills)I divide the dose to 3, take it every 4 or 4.5 hours I increase 2.5 mg each week not optimal due to high cortisol, chronic inflammation (ulcerative colitis),anemia of chronic inflammation. On my labs the T3 goes above the range. According to STTM protocol I am pooling. Do you believe in pooling? My T3 doesn’t get to the cells all my medical problems getting worse. I have sleeping problems as well. Can’t convert T4 it turns to Rt3. I am feeling real bad! I live in Huntington Beach, Ca. can’t find a good doctor.
I recently started NP Thyroid and iodine for subclinical hypothyroidism. My TSH is 2.82, T-4 is 6.7. T-3 is 2.52 and Thyroid Peroxidase AB is 5.76. Prior to starting the NP, I had lowered my A1C from 5.8 to 5.3 and fasting sugars of being in the 90’s. I am 4 pills in and my fasting levels are 120 to 130. This morning it was 120 and 45 minutes after taking the NP thyroid and not eating, my blood sugar went to 150. I am not looking to take diabetic drugs. I supplement with all the ones you listed. My current thoughts are to stop the NP thyroid and stick to exercise, diet and supplements to improve things.
Hi Dave,
Diet and lifestyle certainly work if done correctly, provided your pancreas can still produce insulin.
If your BS is jumping after the meds, your meds are too high.
I have Hashi’s also and with the naturethroid being recalled and pulled from the market, I was switched to NP. I’ve just discovered today I took too many meds(3 pills cause I missed the last 2 days of meds) because my blood sugar was over 200(NOT good for pregnancy!) When I take the correct dosage of NP however(2 pills), my blood sugar does not change. At all.
What are the optimal ranges for blood glucose, insulin and Hemoglobin A1c?
My daughter’s insulin is 18, her glucose is 84, A1c – 5.1. She’s been off sugar and carbs (gluten, as well as potatoes, rice and starchy vegs, and high fructose fruits) for a year, and yet her insulin rose from 11 to 18. Her ALT and AST are elevated (23 and 33 respectively). She’s been unable to lose weight on keto or protein diets, intermittent fasting, etc. Do you think she has insulin resistance? Oh, I forgot to mention her leptin is 22, but I suspect it is because of her weight (she’s 180lbs and 5.5 high).
Thank you!
HI, can fasting on Levo help improve T4/T3 conversion or do you recommend mostly T3 with fasting? Thanks
Curious re: medications that can alter TSH. Currently taking rosuvastatin, metformin, and adderall xr. Started adderall +/- around perimenopause when brain fog became worse. It certainly helped with no side effects. Added a statin and metformin in late-peri to early post-menopause when lipids and sugars became wonky. Now I’m 2 years post-meno and when I take metformin and adderall I get hyperthyroid-like symptoms. With neither I am 100% hypothyroid-like. I read that both dopamine agonists (adderall) and metformin can suppress thyroid. Also that statins can be dangerous with untreated hypothyroid (lower cholesterol too much…something like that). If you have time, and since statins and metformin are so commonly prescribed for the 50 yr. old + group, can you share how these can impact your thyroid. Interestingly, I wake up with high fasting or 120 and go to bed with 95. It’s as if it takes my body all day to shuttle glucose to cells. Athletic, always have been, with a predominantly healthy diet. High blood sugars should not (*yet*) be an issue, certainly not this much of one. Wondering if metformin, and adderall, have led to false negatives on labs, i.e. normal TSH. T3 and T4 are indeed on lower end of scale albeit not in the tank. Have not done an RT3. Exhausting having to educate PCP’s! Have become a medical researcher over the past 2 years to figure my health out. Not doing any HRT, FYI, in case that helps. Tried HRT and became jekyll and hyde (different mood and energy one day to next).
Hi Dr. Childs
I take an NDT as well as T3. My Ft3 and Ft4 had been stable for awhile. And although my PCP and endo are not overly concerned yet, my fasting blood sugar has been creeping up. Past 2 times tested at 107 with an A1c of 5.6. Eat well, thin, exercise. Started taking berberine and chromium picolinate but made no difference in my fasting #. However, my once stable Ft3 is now “in the toilet”. Any chance those supplements could have a negative affect as far as Ft3?
Maureen
Hi Maureen,
The only way I could see those supplements impacting your T3 level is if they are negatively impacting its absorption.
I am considering going off my thyroid medication? And switching to supplements ( yours) it is only now that I am taking thyroid medication that,I am having issues with sugar levels and added weight gain? I wear a sport watch. I am accountable for my workouts. I am burning calories but not losing weight? I gained 4 more pounds in the last month and I just increased my medication last month. Haven’t tried to add T3? I guess I was expecting my doctor to determine if I should add T3.
Can I just stop thyroid medication and switch to supplements?
Hi Carmen,
Supplements do not take the place of thyroid medications but it may be possible for you to get off. You can learn more about that here: https://www.restartmed.com/do-you-have-to-take-thyroid-medication-for-life/