If you have Graves’ disease then you should care a lot about the foods that you put into your mouth.
Why?
Because eating the right foods can increase your chance of putting your disease into remission.
Eating the wrong foods may prolong your disease state and increase your need for permanent thyroid treatments like radioactive iodine ablation and surgical removal of the thyroid gland.
If you want to do your best to prevent these treatments (which should be your goal), here’s what you need to know:
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Eating for those with Active Hyperthyroidism
If you are someone with what I call active hyperthyroidism then you should be very aggressive about making changes to your diet.
You’ll know if you are actively hyperthyroid because you will be taking anti-thyroid medication like methimazole.
This state should be differentiated from those who have had their thyroid removed or ablated.
If you fit into that category then you are functionally hypothyroid and you need to read this article.
If you are actively hyperthyroid then keep reading!
If you fit into this category then you are in a great position because you have the opportunity to potentially put your Graves’ disease into remission and prevent the need for these life-altering treatments.
Here’s what we know about Graves’ disease remission and diet:
Research indicates that roughly 20-50% of Graves’ disease patients will experience spontaneous remission of their disease (1) if they take methimazole for about 12-18 months.
This is actually fairly reasonable, but making changes to your diet can do two important things:
#1. Increase your odds of putting your disease into remission.
And #2. Reducing the rate at which methimazole treatment is needed.
There’s no concrete data to support these claims, but it’s been my experience that they are generally true.
And because there’s virtually no risk in eating more healthy foods, why wouldn’t you give it a try?
If that’s the case, here’s what I recommend:
Foods to Eat
While changing your diet for Graves’ you should focus on eating certain foods and avoiding others.
The healthiest foods are those that are nutrient-dense and are considered whole food.
Here’s a list:
Vegetables:
Get at least 3-5 servings of vegetables each day with at least 1 full serving of brassica veggies.
Brassica vegetables contain glucosinolates which are sulfur-containing compounds that provide support to your liver which is critical in thyroid hormone metabolism.
And other vegetables provide nutrients, fiber, antioxidants, and anti-inflammatory compounds that support immune function.
All veggies are good, but here are some of the best:
- Broccoli
- Arugula
- Cabbage
- Cauliflower
- Collard Greens
- Asparagus
- Bok Choy
- Brussels Sprouts
- Kale
Fruits:
Don’t be afraid to eat fruits if you have Graves’ disease.
They are loaded with antioxidants and fiber and they taste delicious.
Aim to get at least 3-5 servings of fruit each and every day.
Any fruit will work, but here are some of my favorites for Graves’ disease patients:
- Apples
- Apricots
- Bananas
- Blackberries
- Dates
- Blueberries
- Cherries
- Strawberries
- Raspberries
And don’t forget 100% whole fruit juices as well:
- Orange juice – Contains naringin and naringenin
- Pomegranate juice – Contains
- Watermelon juice
- Pineapple juice
Juices contain super concentrated amounts of bioactive compounds compared to their whole food counterparts but make sure they are not processed and that they do not contain any added sugars.
Freshly squeed juice or cold-pressed juices contain more nutrients compared to juices that are pasteurized and processed.
Juices do contain a concentrated source of calories, but research shows that they won’t cause weight gain if they are consumed with a meal.
Protein:
You should consume at least 100 grams of quality protein each day (yes, even for women!).
This is probably the most important thing you can do to prevent the dreaded weight gain that tends to accompany long-term methimazole use.
Eating enough proteins means that you will keep your muscle mass where it needs to be to power your metabolism and improve your caloric burn, even while blocking thyroid function.
Protein consumption also promotes immune health (from the amino acids) and bone health.

Animal protein contains the highest ratio of muscle-building amino acids out there, but you can and should work in some plant sources of protein and fill in any remaining gaps with protein powders.
Animal protein sources:
- Beef, chicken, turkey, fish, eggs, pork (get the highest quality meat you can afford)
Plant protein sources:
- Chia seeds, hemp hearts, quinoa, and green peas
*note: plant sources of protein are less efficient compared to animal sources and contain more calories and fat per serving, but they do provide additional benefits.
Protein powders:
- Plant-based protein powders like pea, hemp, chia, and pumpkin tend to be best, but you may also be able to get by using whey protein if you tolerate it.
Fats:
Fats provide a dense source of calories which can provide constant energy throughout the day and promote more stable blood sugar.
They also support hormones, influence inflammation through their omega 3 and omega 6 content, and provide a source of fat-soluble vitamins.
This only applies if you eat the right fats.
Unfortunately, most Americans consume the most unhealthy types of fat in the form of vegetable oils (soybean corn, canola, etc.).
Instead of eating these inflammation-promoting fats, focus on the combination of healthy oils like:
- Grass-fed butter
- Coconut oil
- Extra virgin olive oil
And real whole food sources of fat like:
- Nuts and seeds (almonds, walnuts, chia seeds, flaxseeds, macadamia nuts, brazil nuts, etc.)
- Avocados
- Coconuts
- Olives
- Nut butters (avoid peanut butter)
- Hard cheeses (avoid soft cheeses)
- Greek yogurt
- A-2 protein milk (organic)
- 100% cacao (unrefined and non-alkalized)
- 70% dark chocolate or higher
My recommendation is to start with protein and work backward:
Focus on getting your 100 grams of protein in each day and then backfill the remainder of your food choices while putting preference of carbohydrates before fats.
If you add fats to your diet as whole foods, you’re less likely to promote weight gain and accidentally consume more than you need.
Use cooking oils sparingly, especially if you are actively trying to prevent methimazole-related weight gain.
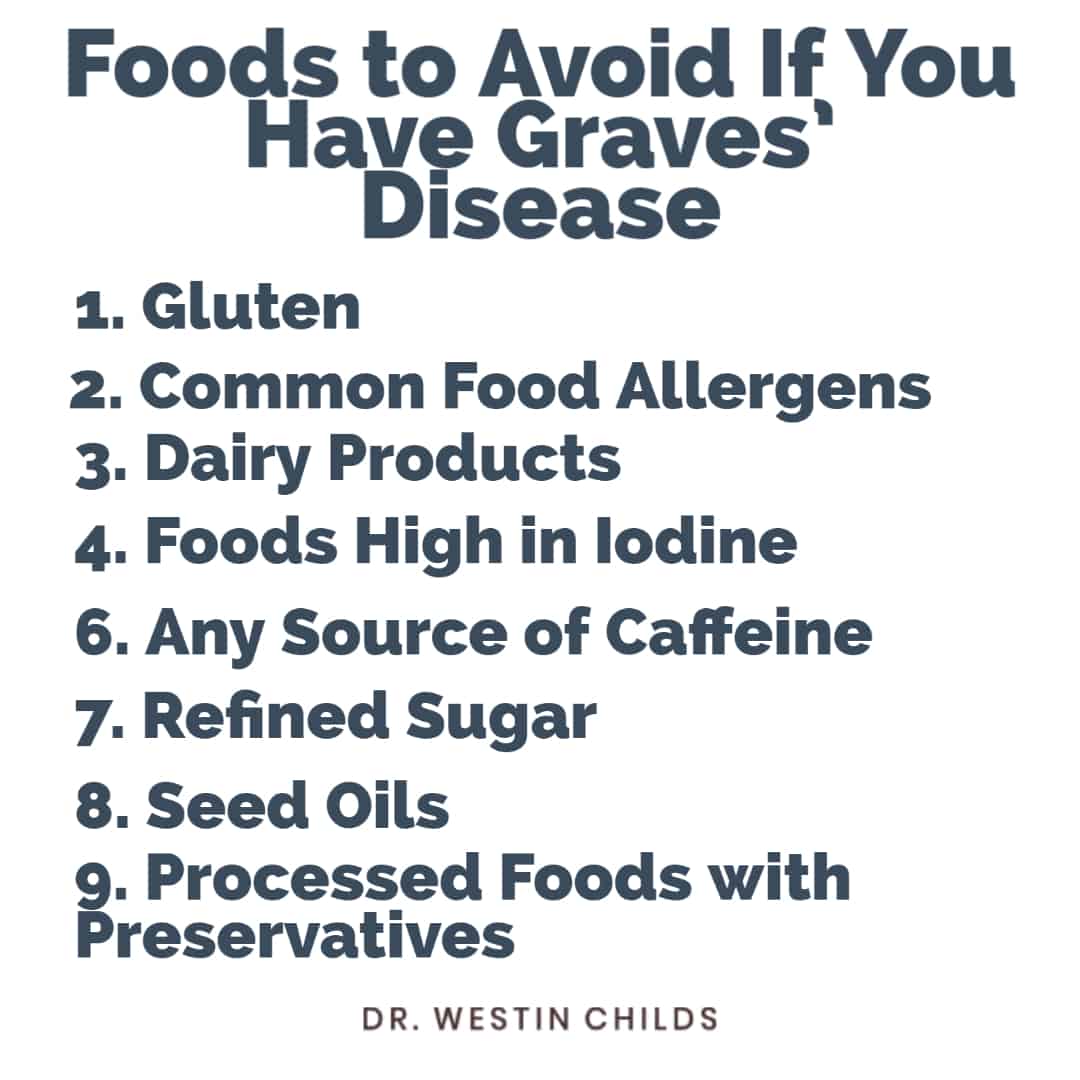
Foods to Avoid
The most unhealthy foods for someone who has Graves’ are those that promote inflammation, rev up the thyroid, and are devoid of nutrients.
Here’s the list:
Gluten
Gluten isn’t a must-avoid food group for everyone, but it is true that patients with Graves’ disease experience problems with gluten more frequently than the average population.
This is probably because there is some crossover between the HLA genes that promote Graves’ disease and those that promote Celiac disease.
Regardless of the exact cause, there’s no question that you are at higher risk of developing Celiac disease if you have Graves’ disease.
For this reason, it’s a good idea for most patients with Graves’ disease to at least give gluten-free a trial run.
Doing so may improve your gut health which will increase nutrient absorption, balance neurotransmitters, and reduce systemic inflammation.
Dairy products
This is one where we need to lean on the studies done in different thyroid conditions, but it’s a good exercise.
We know in the autoimmune disease Hashimoto’s thyroiditis that avoiding dairy can reduce thyroid gland inflammation and help reduce thyroid antibodies.
I know what you’re thinking:
I don’t have Hashimoto’s disease so why does it matter?
Well, it matters because Hashimoto’s and Graves’ disease are two sides of the same coin.
One causes hyperthyroidism and the other causes hypothyroidism, but their underlying triggers are very, very similar.
Knowing this, we can extrapolate that if a food group causes problems for one, it will very likely cause problems for another.
And that is exactly what we see here.
Dairy tends to be a problem for patients with autoimmune thyroid disease primarily because of milk proteins and milk sugars.
These proteins and sugars can be hard to break down in the gut which ultimately promotes inflammation.
Avoiding all forms of dairy isn’t always necessary, but limiting your exposure to lactose and casein is often a good idea.
Foods high in iodine
If you have Graves’ disease then you’ve probably been told to avoid iodine 100%.
This recommendation is made because iodine consumption triggers the creation of thyroid hormone.
And you don’t really want to make more thyroid hormone if you already have more than you need.
While this is theoretically true, this only really occurs if you are consuming way more iodine than you need because the reality is that iodine is a nutrient that every human requires, even those with hyperthyroidism.
But it is true that you shouldn’t go out of your way to hit
Part of doing this just means paying attention to foods that contain a high amount of iodine.
Aside from fish and sea vegetables, the iodine content of everyday foods like milk, dairy, and eggs is not sufficiently high enough to cause problems so you don’t really need to stress about those.
The biggest offenders will come from seaweed and iodine-containing supplements.
Sources of caffeine (including other stimulants)
If you have Graves’ disease then your body is already in a heightened state due to the impact thyroid hormone has on the body.
And if you put any extra pressure or stimulation onto your body, you will tip the balance in favor of even more stimulation.
This can trigger a cascade of events leading to things like insomnia, heart palpitations, excessive sweating, and even more thyroid hormone production.
Avoiding this means avoiding stimulants of all types including coffee, caffeinated beverages, stimulating medications, or anything else that revs the body up.
Common foods allergens
You don’t have to avoid all common food allergens (1), but you should be aware that Graves’ disease (and hyperthyroidism in general) promotes the production of histamine.
And histamine is a highly reactive compound that gets triggered when you consume certain foods.
If this happens then you may experience the symptoms of histamine excess including things like:
- Flushing
- Heat intolerance
- Skin irritation
- And dilation of blood vessels
Many of these symptoms not only overlap with hyperthyroid symptoms but may make them worse.
Not everyone with Graves’ disease will experience excess histamine release, but it’s worth paying attention to if you find that you are highly reactive to anything that you eat.
Common allergens that may cause this problem include:
- Milk
- Eggs
- Shellfish
- Tree nuts
- Peanuts
- Wheat
- And soybeans
Refined carbohydrates & processed sugars
It’s definitely in vogue to hate sugar right now, but that’s for good reason.
Refined carbohydrates and processed sugars contribute to obesity, insulin resistance, and inflammation.
But don’t confuse these types of sugars and carbohydrates with whole food sources of carbohydrates and sugar like fruit.
It’s perfectly health to consume fruit and 100% fruit juice.
The same isn’t true of any food that has EXTRA sugar added to it.
This may include sugar-sweetened beverages (coke, Pepsi, etc.), certain fruit juices, some fruits (cranberries), breads, pasta, and so on.
Industrial seed oils
Seed oils are heavily processed fats that have made their way into just about every food you can think of.
Well, not every food, because whole foods don’t contain them, but if you are eating anything that’s processed or anything from a restaurant there’s a good chance it’s there.
And that’s unfortunate because these oils are high in omega-6 fatty acids, they may promote inflammation and can contribute to thyroid dysfunction.
And because there’s much better alternatives available, there’s really no good reason to keep these in your diet.
Ultra-processed foods
Ultra-processed foods promote inflammation, and gut damage, disrupt hormones, lead to obesity, and are devoid of essential nutrients.
Their consumption is associated with just about every chronic disease you can think of and Americans consume them at astonishingly high rates.
It’s estimated that up to 70% of the average American’s diet consists of ultra-processed foods which tracks perfectly with the rise in many chronic medical conditions.
You don’t have to remove these foods from your diet 100%, but you should focus on something that approximates the 80/20 rule or the 90/10 rule.
In other words, at least 80-90% of your diet should consist of real whole foods which leaves 10-20% for processed foods.
In a perfect world, you’d be able to avoid them all the time, but that isn’t always possible.
Alcohol
There’s really no good reason to consume alcohol if you have Graves’ but there are two big reasons you should avoid it if you have hyperthyroidism:
The first is that it can trigger hyperthyroid symptoms such as heart palpitations, tremors, and anxiety.
And the second is that it must be metabolized through the liver which is the same place where methimazole is metabolized.
Because it’s considered a toxin to the body, just avoid it 100% and call it a day.
Will Changing Your Diet Cure Graves’ Disease?
Maybe, maybe not.
But given that your only other alternative is to sit around and wait while you take methimazole, changing your diet seems like a pretty good option.
You simply can’t go wrong by eating more fruits and veggies, no matter how you slice it.
And doing so can help reduce inflammation which may act to treat the underlying cause of Graves’ disease which is inflammation and autoimmunity.
If you can do this, then you are one step closer to curing your condition.
But let me be clear:
There is no guarantee that changing your diet will put your disease into remission.
But your #1 goal, if you have Graves’ disease, should be to do everything in your power to reduce your risk of undergoing radioactive iodine ablation and/or surgical removal of the thyroid gland.
While diet is certainly helpful, there are supplements that can help as well.
And if you want to see a list of the strongest, check out this article next.
Scientific References
#1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2111403/#__sec6title
#2. https://www.ncbi.nlm.nih.gov/pubmed/10931424
#3. https://www.ncbi.nlm.nih.gov/pubmed/11531931