Are you suffering from hot flashes, weight gain, depression, or other symptoms of low estrogen?
Have you considered using the medication estradiol to help reduce these symptoms?
If so, this is the article for you.
We are going to discuss the importance of estradiol in the female body, how it interacts with other important sex hormones, the symptoms associated with low estradiol, and how to supplement/medicate with this hormone:
What is Estradiol (The Hormone)?
As a woman, it is very likely that you’ve heard of the term estrogen before.
But do you know what the term “estrogen” actually refers to?
Estrogen is really a non-specific term used to describe a class of hormones that all act on the estrogen receptors in your cells which are located throughout your body.
Estradiol is the most abundant estrogen in your body and it’s considered to be the strongest out of all estrogens.
Estradiol is the sex hormone in the female body which is responsible for MANY of the changes that we associate with the female body.
Breast development, the texture, and glow of the skin, the placement and development of fat in certain areas of the body (2) (hips/butt/etc.), sex drive/libido (3), mood/temperament (4), body weight, etc.
These very important characteristics, displayed by women, are all felt to be the result of estradiol (and other estrogens) action on your cells.
Not only does estrogen play a critical role in the development of your body, but it also plays a very important role in your overall health.
The decline in estradiol after menopause is felt to be one of the major, and driving catalysts of heart disease (5), stroke, and cancer that women experience as they age.
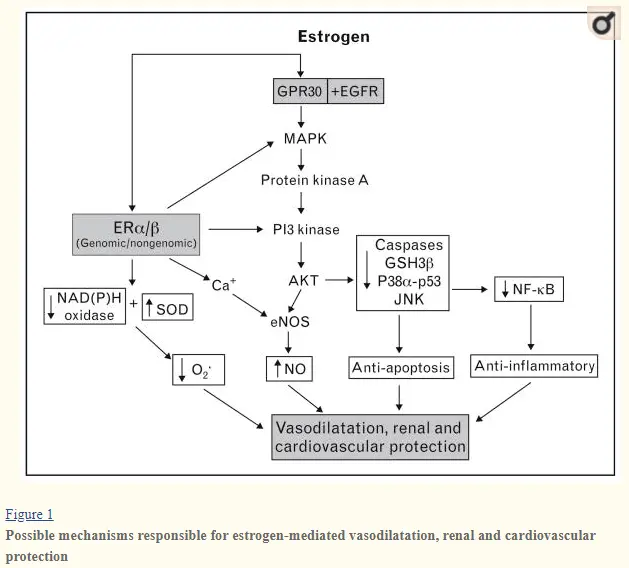
This has led to experimentation with estradiol replacement therapy to try and blunt the negative effects associated with the aging process.
This article will focus on how and when to use estradiol as a medication, but also how to use it safely.
There are many other estrogens in your body, including metabolites that are created as your body breaks down estradiol and other estrogens which your body creates intentionally (6), but none are as powerful as estradiol.
Whenever you hear Doctors or other patients, talk about estrogen you can bet that they are almost always referring to estradiol.
In fact, most Doctors aren’t familiar with or know how to interpret, other estrogens such as estrone and estriol.
Because of this, estradiol is almost always the topic of discussion when you heard someone talking about estrogen.
But estradiol is more than just a hormone, it’s also a medication and one that can be used in situations of low estrogen.
Using Estradiol for Menopause & HRT
Estradiol, as a hormone, is one of the best ways to treat women who are suffering from menopause.
Menopause is a condition that all women will eventually face as they age.
When women hit menopause they often suffer from very specific conditions such as hot flashes, depression, weight gain, brain fog, and low energy (7).
You probably intuitively realize that these symptoms are the result of the hormonal change which occurs in the body, and you would be right to think so.
What you may not realize is that the MAJORITY of these symptoms results from the dramatic drop in estradiol levels seen in menopausal women.
Menopause is the result of ovarian failure (the main place that estradiol is produced) which brings estradiol down from “normal” levels to almost near zero levels.
Imagine spending your entire life as a menstruating woman, with all of your cells recognizing and used to normal estrogen receptor activity when all of a sudden it basically drops to zero levels.
You can imagine how your body reacts to such a situation and this is one of the reasons that women have a very tough time during the menopause transition!
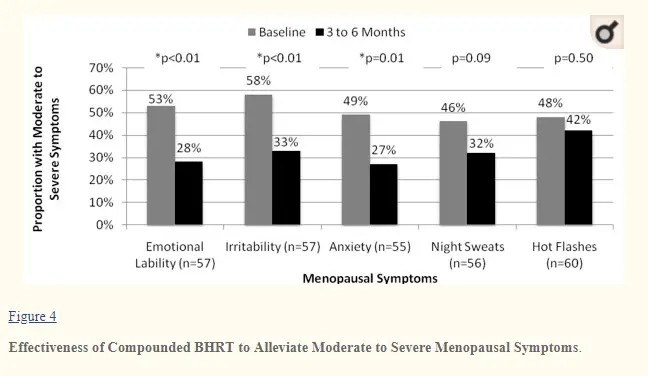
Because the majority of the symptoms associated with menopause are caused by the rapid drop in estradiol levels, it makes sense that using estradiol as a treatment would help reduce those symptoms.
And that’s exactly what we see happen when menopausal women use estradiol.
While it is true that estradiol therapy is an incredibly effective tool for menopause, it should be noted that it is not without its controversy.
Some Doctors believe that the use of estradiol may increase the rate of breast cancer and stroke.
Some studies show this to be the case, but there are ways to not only use estradiol without increasing your risk of these side effects but to also reduce your risk of developing dementia and other medical conditions (10).
The controversy surrounding HRT (hormone replacement therapy) has to do with the exact amount that is used.
When HRT was a relatively immature field and practice of medicine, Doctors would use very high doses of synthetic and bio-identical hormones simply because they didn’t understand how dosing worked in the female body.
The negative side effects associated with HRT stem from the overuse of estradiol and the use of synthetic estrogens (11) (not bio-identical estradiol).
As long as estradiol is used in low doses (only a sufficient amount to reduce your symptoms but without causing symptoms of excess) then the risk of these outcomes is reduced (12).
From a logical standpoint, why would the use of estradiol (in normal levels that your body has been used to for decades) cause breast cancer all of a sudden?
The use of estradiol as a hormone can scare people, but remember that you should only aim to use the exact amount that your body is used to.
Using this amount should NOT result in negative outcomes.
After all, if your body tolerated it for 40+ years why would it all of a sudden reject the exact same hormone now?
There are an art and a science to hormone replacement therapy, especially with estradiol, and you should never take estrogens unless you have a known and documented deficiency.
Testing for Low Estrogen/Estradiol (Test before you use!)
One of the best and most effective ways to identify low estrogen is to simply use a standard blood test.
Serum blood testing can be used to isolate and quantify the number of hormones that your body is able to produce.
Estradiol, along with progesterone, can be tested in your blood and should be tested before you decide to use this powerful hormone.
These basic hormones can be easily ordered by your physician and are covered by insurance (so it shouldn’t cost you any out-of-pocket money in most cases!).
Identifying and diagnosing low estradiol is actually much easier than high estrogen.
Low estrogen, including estradiol, is seen in loads of women who are post-menopausal.
Why?
Because the ovaries no longer produce the hormone!
So, classic blood tests in post-menopausal women look like this:
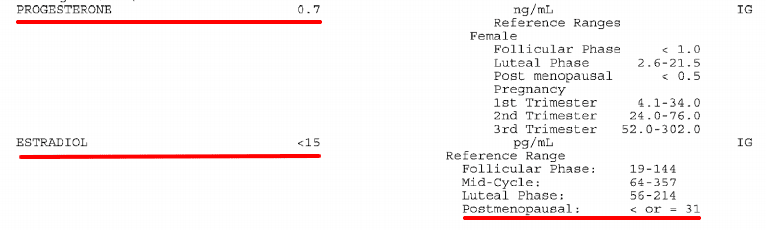
In this example, you can see that the estradiol level is less than 15 pg/mL which is the most sensitive range that this particular lab test can quantify.
This kind of presentation is classic among post-menopausal women.
Whenever you decide to test for estradiol, make sure that you also test for progesterone.
These hormones should not be evaluated in isolation, and instead should always be ordered in pairs.
Progesterone is the perfect counterbalance to estradiol, so using one without the other may cause imbalances in the body and further symptoms.
You can read more about progesterone testing in this article.
Just like estradiol, progesterone levels tend to be very low in menopausal women.
Dosing Estradiol & Other Estrogens
It would be nice if I could give you the exact guide to dosing estradiol but, unfortunately, it’s not quite that simple.
You have to realize that each person is slightly different in terms of what is “normal” for them and how well they will “tolerate” hormone replacement therapy.
What this means is that each person will probably need their own unique dose of estradiol which will need to be adjusted to over time.
The best way to get to that point is with frequent blood tests and with frequent symptom evaluations.
Dosing based on these two principles will help you achieve the optimal dose without increasing your risk of the negative side effects we discussed previously.
You will notice that most standard pharmaceutical estradiol preparations come in standardized doses which are not necessarily easy to titrate or adjust.
Because of this, it may be necessary to get your estradiol in a compounded cream or gel.
Compounded estradiol (especially if in the bi-est formulation), at low doses, is easier to titrate when compared to some standardized pharmaceutical formulations.
After all, it’s both safer and easier to increase your dose as opposed to reduce your dose.
When in doubt make sure to follow the outline below and always start low and go slow!
Do’s and Don’ts of Estradiol use:
DO’S
- Take enough to reduce your symptoms (hot flashes, etc.)
- Use estrogen via the transdermal route
- Check your serum estrogen and progesterone level frequently
- Use in conjunction with progesterone
- Take a “hormone holiday” either weekly or monthly
- Take only in the setting of documented deficiency of estrogen after evaluating your own personal risks (history of breast cancer, etc.)
DON’TS
- Don’t use enough estradiol to cause breast tenderness or menstrual bleeding
- Take estradiol orally
- Take hormones without assessing your serum levels over time
- Use estradiol by itself or without progesterone
- Use continuously, without taking hormone holidays or breaks for your body
- Take because of “suspected” low estrogen without testing your blood first (other imbalances can mimic low estrogen)
- Take if you are menstruating
It should be noted that HRT, of any kind but especially estradiol, should be done with the guidance and care of a knowledgeable physician.
There is simply no substitute for this kind of care which will dramatically increase the amount of time it takes for you to adjust your medication and find an optimal level for you.
Bi-est vs Estradiol vs Progesterone for HRT
As a medication, estradiol can be taken by itself or, more frequently, used in combination therapy with other hormones or even estrogens.
Among physicians who specialize in hormone replacement therapy, bi-est is rarely given by itself.
Instead, it is often compounded together with another estrogen known as estriol.
The combination hormone of estradiol + estriol is known as bi-est and this combination is usually further paired with progesterone.
The reason that estradiol is paired with estriol is that, by itself, estradiol is a very potent estrogen.
Remember, one of the main tenets of hormone replacement therapy is to provide only the exact amount of hormone necessary to the body (without providing excess hormone).
Estriol, a weaker estrogen, is felt to be protective of certain tissues (such as breast tissue) when combined with estradiol.
In this way, it’s possible to take estriol as an estrogen blocker of sorts (even though it is estrogen itself), to help combat the potency of estradiol.
Most formulations of bi-est contain around 80% estriol to 20% estradiol, so the dose of estradiol necessary is often much smaller than you realize.
The ratio and concentration of estrogens in bi-est can be further titrated or adjusted based on the needs of the individual (some women will simply need more estradiol compared to others).
In addition, bi-est is often paired with progesterone which also has antagonistic effects on the growth potential of estrogen.
Progesterone, from the perspective of the body, helps to balance estrogen (13).
When you undergo hormone replacement therapy, you will want to mimic this natural pattern to the best of your ability.
Doing so will help reduce unwanted and negative side effects.
Side Effects of Estradiol
Is Estradiol safe to take? Does it have side effects?
The short answer is yes, and the long answer is maybe.
Most of the side effects associated with estradiol stem from either over-use of the hormone (meaning your dose is too high) or the fillers/binders in the gel/cream preparation (meaning an inactive substance inside of the medication).
It’s very unusual for someone to be “allergic” to the active hormone ingredient of estradiol.
Your body should be used to this hormone because it has produced it naturally for decades.
Having said all of this, I’ve provided a list of some of the symptoms associated with estradiol use reported by women:
- Weight gain
- Bloating
- Hot flashes
- Breast tenderness
- Menstrual bleeding
- Irritability
- Mood changes
- Headaches
Many of these symptoms tend to subside by adjusting your dosing.
And this is where a knowledgeable physician can help you dramatically.
When you experience symptoms always do your best to determine if the symptoms you are experiencing are caused by excessive dosing (meaning too much) or by insufficient dosing (meaning too little).
It’s very possible to use estradiol and still exhibit symptoms such as hot flashes, but with a little bit of finer titration, the symptoms will subside.
Because estradiol is a potent estrogen it is not available over the counter (unlike progesterone which is available OTC).
This means you will need a prescription from your Doctor to get this hormone.
Final Thoughts
Estradiol is a powerful and potent hormone that can be used as part of hormone replacement therapy for women who suffer from low estrogen (or the symptoms of low estrogen).
The most common condition which causes low estrogen is menopause and this is something that ALL women will experience at some point in their life.
This doesn’t mean that all women necessarily have to take estradiol therapy, but it can, and should, be considered in women who suffer from quality-of-life symptoms associated with menopause.
Whenever you consider using estradiol ensure that you are using a small, but sufficient, dose that will take away your symptoms without overmedicating your body.
This strategy will help you reduce almost all of the negative and unwanted side effects associated with estradiol use.
For many reasons, it may be better to use the formulation bi-est instead of estradiol therapy.
In addition, you should always consider using progesterone along with estradiol to help combat the growth-enhancing effects of estradiol on endometrial and breast tissues.
Now I want to hear from you:
Do you have low estradiol levels?
Are you also in menopause?
Have you considered HRT before?
Are you using it now?
Is it working for you?
Leave your comments below!