Is having a suppressed TSH dangerous to your body?
Will it cause bone loss or damage to your heart?
Can the negative side effects be mitigated or avoided with other interventions?
In this post, we will discuss the pros and cons of having a suppressed TSH including what potential negative side effects it can cause, how to avoid them, and how you should dose your thyroid hormone.
Let’s jump in:
What Does it Mean to Have a Suppressed TSH and is it Dangerous?
A suppressed TSH is a way to refer to a condition in the body in which the TSH is lower than it should be under “normal” conditions.
TSH suppression occurs as a result of taking too much thyroid medication but is also secondary to certain medical conditions which cause hyperthyroidism (such as Graves’ disease).
In this article, I am going to be referring to TSH suppression secondary to the use of thyroid medication (meaning endogenous TSH suppression) because of its impact on patients who take thyroid medication.
It is estimated that anywhere from 25 to 40% of patients taking thyroid hormone may have a suppressed or “below normal” TSH.
The state of having a low TSH is considered to be a big problem and one that often results in Doctors altering (reducing) the dose of thyroid hormone a patient is taking.
This is often VERY confusing to patients, especially because usually when their TSH is low they often begin to feel better from a symptomatic standpoint.
So, from the patient perspective, why would a Doctor alter the dose of thyroid hormone if they are finally feeling better?
The answer has to do with the fact that TSH suppression is felt to lead to two potential negative side effects.
That of bone loss and heart problems (1).
But is this really a concern?
The answer may not be as clear-cut as you’d think.
In order to have a logical and coherent and honest discussion about TSH and its impact on your health we need to answer some basic questions:
Is causing TSH suppression with the use of medications the same thing as when it occurs from Graves’ disease?
In other words:
Is TSH suppression from exogenous hormone equivalent to TSH suppression from endogenous hormone?
How does the degree of TSH suppression impact the negative consequences?
In other words:
Is TSH suppression with T4 medication equivalent to TSH suppression from T3-only medications?
Is one worse than the other, are they the same?
There is evidence to believe that endogenous causes of hyperthyroidism may result in cellular hypersensitivity (2) (especially to tissues that are sensitive to catecholamines) which may not be seen in hyperthyroidism caused by excessive dosing.
What this means is that taking too much thyroid hormone by mouth may result in a suppressed TSH and high free T3, but this state may NOT be equivalent to the suppressed TSH and high free T3 seen in endogenous causes of hyperthyroidism such as Graves’ disease.
This phenomenon may explain why patients with endogenous causes of hyperthyroidism exhibit obvious signs of hyperthyroidism (such as weight loss, tremors, heart palpitations, and so on) while patients with a suppressed TSH secondary to medication use can, and often do, experience symptoms of hypothyroidism (weight gain, fatigue, cold intolerance, constipation and so on).
If these two conditions are the same then someone must explain how they can result in polar opposite symptoms in patients.
Does the benefit of TSH suppression outweigh the potential negative consequences of experiencing hypothyroid symptoms for an indefinite amount of time?
In other words:
Is it better for your health long term for you to be 40 pounds overweight or would you rather lose your weight and experience a risk of 1% bone loss per year due to a low TSH?
There isn’t a clear answer and the answer likely depends on the patient.
This should be a conversation that each person has with their Doctor to determine if the risk is potentially worth taking in their individual case.
Lastly, is there any risk of temporary TSH suppression for 3-9 months?
In other words:
Is there any harm that will occur if you temporarily suppress the TSH in an attempt to fix or reduce symptoms or help with weight loss?
If there is no short-term risk (and I would argue that most of the risk from using T3 isn’t realized until TSH suppression has been present for years) then what’s the harm in a trial of altering thyroid medication?
Suppressed TSH and Bone Loss (Osteoporosis)
One of the most cited concerns for TSH suppression is the potential loss of bone or the cause of osteoporosis.
The logic goes that suppressing your TSH will lead to an inevitable decline in bone health and an increased risk of fracture.
Bone cells have thyroid hormone receptors and therefore they react to changes in thyroid hormone (3).
In cases of endogenous hyperthyroidism (meaning your body produces too much thyroid hormone), patients do experience an increase in osteoporosis and fracture risk.
This logic has led physicians and patients to be scared of increasing thyroid dosing in fear that it may cause the same effects.
Doctors are worried that taking too much thyroid hormone (T4) will result in the same risk that hyperthyroid patients experience.
But is this actually observed in studies?
Sort of.
Some studies do show that TSH suppression does cause an increased risk of osteoporosis but with 2 very important points.
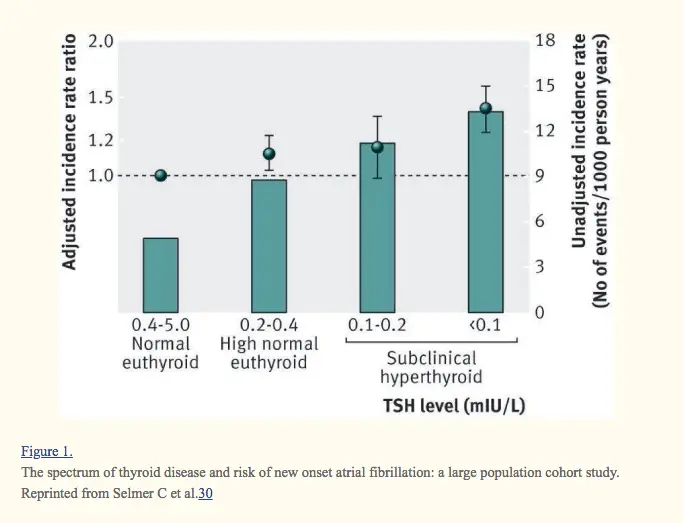
The absolute risk of osteoporosis and bone loss depends on the DEGREE of TSH suppression (4).
For instance:
If your TSH is less than 0.1 then you will experience more bone loss than someone with a TSH in the 0.2 to 0.5 range.
Second, this increase in risk is really only statistically relevant in women who are post-menopausal.
Pre-menopausal women do not see a statistically significant increase in bone loss presumably due to the beneficial effects of estrogen on bone maintenance.
But this begs a very important question:
Can the risk of bone loss be mitigated (reduced) in post-menopausal women with the use of bio-identical estrogen replacement therapy?
We don’t have an answer to this because the use of hormones isn’t widespread, but it may be worth considering on a case-by-case basis.
Is there a risk of bone loss in post-menopausal women who use thyroxine but have a normal TSH?
The answer is no.
The question is whether or not this TSH suppression is worth it (based on your case) and whether or not you can mitigate your risk based on other therapies.
In general:

If you are a menopausal woman (meaning you are menstruating regularly) then TSH suppression is likely not going to cause any significant risk to your bone health even if used long-term.
In the most severe cases, menopausal women with TSH suppression may realize a bone loss rate of 0.3% per year.
But what if you are a post-menopausal woman (meaning you no longer have menstrual cycles)?
It seems if you fall into this category then you will realize an increased risk of bone loss and osteoporosis based on how long your TSH is suppressed and how suppressed your TSH is.
Women who fall into this category may experience up to 1% bone loss per year, which after 10 years may increase their risk of fracture significantly.
What isn’t clear, however, is if this risk can be completely reduced with the use of bio-identical estradiol and progesterone with the idea to bring these hormones back to youthful levels.
This study highlights the importance of hormone control BEYOND thyroid hormone in all patients, and it highlights that physicians shouldn’t necessarily be scared of a slightly suppressed TSH in all patients.
What about the use of Calcium instead of estrogen?
Some studies do show that supplementation with calcium, even if your TSH is suppressed, may help prevent bone loss issues.
Does this mean that you should suppress your TSH?
Not necessarily, but it does mean that you should have a meaningful conversation about the risks vs the benefits with your current physician.
While bone health is important, there are other factors that should be considered with TSH suppression as well, and that includes heart health.
Suppressed TSH and Heart Problems (Atrial Fibrillation & Cardiac Enlargement)
There’s no question that thyroid hormone has an impact on cardiac function and cardiac size.
Studies have shown that thyroid hormone helps regulate the heart rate, and the size of the heart and has an impact on the pressure in various chambers in the heart (including the pulmonary arteries).
So why are Doctors and patients concerned about the heart when it comes to their thyroid?
It is then assumed that these complications would be seen in patients who take excessive doses of thyroid hormone by mouth for conditions such as hypothyroidism.
The problem with this thinking is that both conditions, hyperthyroidism caused by disease states and exogenous hyperthyroidism (caused by taking too much thyroid hormone), are considered to be equivalent and the same.
More studies are necessary to prove that this statement is in fact true.
In the meantime, it’s important to understand how thyroid hormone actually impacts the heart, especially if you are taking suppressive doses of thyroid hormone.
What’s interesting about the heart is that it only responds to T3 but it lacks the ability to alter T4 into T3 in its own tissues (9).
This means that your heart is particularly sensitive to T3-containing medications such as Cytomel/liothyronine and Natural Desiccated Thyroid hormone.
The heart is sensitive to T4 medications but only in patients who readily convert T4 into T3 (and we know that up to 15% of people may have an issue with this conversion).
What does this mean for you?
It means that you are more likely to experience cardiac effects when taking thyroid medications that contain T3.
It also means that we shouldn’t necessarily make general assumptions about the impact of thyroid hormone on the heart without differentiating between thyroid medications.
So, can we look at TSH suppression and the heart the same way that we view TSH suppression and your bones?
Not exactly, but there may be some similarities.
The impact of thyroid hormone on heart tissue depends on two important factors:
The first is the degree of TSH suppression.
The second is the length of time in which your TSH is suppressed.
Many of the complications of hyperthyroidism, aside from heart palpitations, may take years or decades to cause an issue.
It takes quite a bit of time for cardiac remodeling (hypertrophy) to cause gross or overt cardiac dysfunction.
Another very important point is that several studies have shown that reducing thyroid hormone (fixing the problem) causes a complete reversal in cardiac complications (heart problems).
What does this mean for you?
Several things:
It means that using TEMPORARY suppressive doses of thyroid hormone is not likely to cause any long-term cardiac complications.
It also means that, if you are taking suppressive doses of TSH, the use of a beta-blocker may be enough to completely PREVENT cardiac complications.
There may be situations in which suppressive doses of thyroid hormone may be beneficial, but you should always consult with your physician and determine if the benefits outweigh the risks.
It’s plausible that temporary TSH suppression, with the goal of weight loss in mind, may reduce your risk of cardiac issues long-term in exchange for a temporary (and reversible) risk of cardiac issues such as heart palpitations.
Should You Suppress your TSH?
Dosing based on the TSH is an interesting concept and not one that is used for other hormones in the body.
Take for instance the case of birth control pills.
Prescribed birth control pills, when taken by mouth, act to completely shut down FSH and LH from the pituitary.
Remember that TSH is a pituitary hormone, much like FSH and LH, but Doctors never bother to check FSH and LH when using birth control because they know that they will be suppressed.
Birth control pills come in a standardized dose and hardly any thought is given to the degree of FSH/LH suppression when they are being used.
Why then is the TSH given so much more weight when compared to FSH and LH? Even though BOTH hormones are secreted by the pituitary gland?
The answer isn’t clear, but this is something that should be evaluated in future studies.
We do know, as you might suspect, that there are instances when the TSH is not necessarily the best measurement of thyroid function in the body.
Even though this is the case, it doesn’t mean that the TSH should be ignored when dosing thyroid hormone.
But it does mean that other factors such as Free T3, Free T4, Reverse T3 and other thyroid tests should be evaluated in conjunction with the TSH.
Suppressive doses of thyroid hormone may be beneficial in some patients, but you should never adjust your thyroid dosing while dismissing the TSH entirely.
The bottom line?
Following your TSH is an important part of thyroid hormone management, but it shouldn’t be the only test you order.
There may be some risks associated with TSH suppression (from endogenous thyroid hormone) but some of these potentially negative side effects may be avoided.
If you are taking suppressive doses of thyroid hormone ensure that you are monitoring bone density and cardiac function.
You can evaluate bone density with a DEXA scan and you can evaluate cardiac function with an echocardiogram.
In some cases, bone loss may be prevented or avoided with the use of bio-identical hormones such as estrogen or with calcium supplementation.
In some cases, cardiac complications may be prevented or avoided with the use of beta-blockers (12).
Your goal should NEVER be to suppress the TSH, but it may not be a serious problem if it is done correctly and only for a short period of time.
Now I want to hear from you:
Are you currently taking suppressive doses of thyroid hormone?
Are you experiencing negative side effects associated with your TSH being low?
Do you have a low TSH but still experiencing the symptoms of hypothyroidism?
Leave your comments below!






Hi Dr. Childs, I’ve suppressed my TSH to .08 in order to get my FT3 up to 3.9 from the high 2s. I did this by converting from Synthroid to Naturethroid and from there titrated a lot. It’s a hard but now at 1.5 grains via 2 doses a day. The biggest issue is hair loss and severe scalp pain this has been going on for 1.5 years now and no one knows how to treat it. I thought going up in FT3 would stop but now I”m experiencing just as much hair loss as before. The scalp also itches a lot and has produced strong pungent odors. I really need help, I’ve gone up and down the eastern seaboard to doctors. I decided to cut back 1/4 grain today to see if the hair loss stops and hair growth occurs. My hair was thick and shiny but now is thin, limp and baby hairs that do grow fall out. Please let me know if you have any experience with this. I feel so trapped in a maze.
Hi Katherine,
There are many reasons for hair loss among thyroid patients including the type of medication you are taking, the dose and nutrient status. You can read more about all of these factors here: https://www.restartmed.com/thyroid-hair-loss/
Dr. Childs,
I was on 90 mcg of Armour a month ago and had the following lab results:
TSH: 0.245
Free T4: .79 (range .82-1.77)
T3 Uptake: 26 (range 24-39)
Reverse T3: 8.3 (range 9.2-24.1)
My doctor reduced my dose and had me alternate 60/90 on alternating days. Three weeks into this new regimen I began experiencing major brain fog, headaches, difficult swallowing. I feel awful, the brain fog being the worst symptom.
The kicker is I had more labs run on week 4 and my TSH tested at 0.07 and free T4 at .84. I don’t know what to do and am worried my doctor will reduce my dose further and I will feel worse. I also have hashimotos if that makes a difference. Please advise!
You’re T3 is not optimal at 3.9. The optimal range is 4.5-4.9. I had hair loss and a dry scalp with a T3 of 4.0. Reverse T3 also needs to be tested and is likely at play, lowering the amount of T3 available to your body. My TSH is at 0.01 and Free T3: 4.5-4.9. I feel amazing! I’ve never been here before with my health. The amount of Free T3 is not enough to cause health issues. Patients have had their thyroids removed, a TSH of 0.00, and do not have health issues. T3 is the active hormone used by your body.
Hi Dr. Childs
Yes is the answer to your question about anyone experiencing hypothyroid symptoms with 0.03 TSH levels. How can this be?
I listened to your post today which was excellent and very informative about suppressed TSH.
How can this be?
Diagnosed with Hashi’s Dec 2014. Had t4 starting Levothyroxine mcg per day 50,75,100,125,159,175, over the last 3 years with fluctuations in responses.
I am pre menopausal and tested strong oestrogen levels at dec 2017.
Three months ago I started a combo of 25mcg T3 liothyronine and 100mcg euthyroid t4 as I had debilitating brain fog.
Brain fog now is gone but hypothyroid symptoms back with a vengeance. I sleep till 2 pm every day, weight gain, no energy, zero libido, hair loss and dry skin and TSH not budging past 0.05.
I don’t know what to do?
Hi Genevieve,
The TSH means relatively little by itself unless it is also paired with free thyroid hormones in the serum. You can learn more about how they all interact here: https://www.restartmed.com/normal-thyroid-levels/
Hi Dr. Childs,
Thank you for all of your great info on your website. I just recently had my labs done and my TSH was too low at 0.091 UIU/ML but my T3 and free T4 were WNL at 1.1 NG/ML and 1.5 NG/DL respectively. I don’t feel bad, by I continued to have minor symptoms across the board including resistance to weight loss on a good routine. My doc has dropped my dose, and now I am worried that I may gain more weight! Any thoughts on why too much TSH didn’t help me lose weight and why my other levels are normal when my TSH was not? I am starting some of your supplements to see if they help!!!
Hi Amanda,
That’s great! Keep us updated on your progress over the next few months as you use the supplements. Thanks for stopping by and sharing your story.
Hi Dr. Childs,
For yrs, I’ve bounced from Dr to Dr trying to get someone to listen to me and my symptoms of hypothyroidism. All I ever heard was your TSH is normal. Diagnosed with depression having no energy and gaining so much weight I didn’t even notice myself. My TSH has always run between 1- 2.5 with my free T4 level decreasing every check last being 0.7
Still, endocrinologist says I’m within normal range.
I finally convinced my psychiatrist to wean my antidepressant and try me on Cytomel, which within 2 weeks I felt like I woke up and had energy and less depressed. I recently had my labs checked after being on Cytomel 25 for 2.5 months. My TSH was 0.5, free T4 .67 and T3 5.
The last two weeks I feel like my energy is dropping low again and depression is worsening. I’m not sure if I need to ask my psychiatrist to increase my Cytomel dose or if my dose could be too high causing these symptoms to reappear?
Thanks for your time,
Julie
Hi Julie,
Adjusting your Cytomel dose, if it’s being used primarily for depression, follows different guidelines than when it is used for hypothyroidism. It’s more about your symptoms, how you are feeling and if you are experiencing negative side effects of excessive thyroid dosing.
Dear Dr. Childs,
I’m a 54 yr old, postmenopausal woman, diagnosed with Hashimoto’s hypothyroidism, adrenal fatigue, insulin resistance and metabolic syndrome under the care of a functional medicine physician. However, she can’t tell me why my TSH continues to climb for a year from 4. to 8.to 12. to 24.to now 29., despite taking a regularly balanced dosage of T4 and T3 from a compounding pharmacy. This started a year ago when I began T4 and Cytomel. Currently, my T4 levels are within range, and my T3 is low. I am MISERABLE. I don’t know where to search, for an understanding of what is happening to me?
Hi Mary,
It’s pretty straightforward! Your demand for thyroid hormone changes as you age and as you are subjected to stressors. Normally your body can produce an increase (assuming it is functioning normally), but if it can’t then you may need to adjust your thyroid medication.
Hi
My TSH is 0.01 my T4 25 and T3 4.6
My GP has reduced my Levothyroxine and QI am now experiencing a temperature drop, foggy mind and a lot of muscle pain which is spoiling my sleep. I am annoyed because I was feeling well before.
Hi Sylvia,
That’s the age-old battle that patients play with their doctors when they chase the TSH. Your doctor may have changed your medication because of your suppressed TSH. You can read more about the potential dangers of that condition here: https://www.restartmed.com/suppressed-tsh/
Hi Dr.Childs
Thanks for the redirect to this article.Yes I’m still suffering from hypothyroidism even with a suppressed TSH and being told im hyper “sigh”. Do you have any information on thyroidectomy and tendon and muscle pains and why this occurs and how to fix it ? I’m pretty crippled up with severe feet, ankle and knee pains that I can only walk or stand 15 to 30 minutes at a time I use to run half marathons and reduced to walking 10 miles per day to hardly able to stand or walk. I can’t find real reasons for this, is it because of suppressed tsh or hypothyroidism or something else? Thanks Grace
Hi Grace,
You can learn more about chronic pain and thyroid disease here: https://www.restartmed.com/hypothyroidism-chronic-pain/
Hi Dr. Childs,
Thank you so much for all the very useful information.
I have just received my latest test results for tsh, ft4 and ft3. I have Hashimoto’s thyroiditis (TPO >1300) and am taking 58.3 mcg levothyroxine.
My latest blood test shows my TSH as being 0.29 (range 0.5-4.4), ft4 18.5 (10-20) and ft3 5 (3.5-6.5). I know my doctor will want to reduce my Levothyroxine due to the suppressed TSH but I have only just started to feel human again with some of my worst symptoms completely disappearing. What would you advise if you were my GP?
I am post menopausal and not on HRT.
Your comments would be greatly appreciated.
Best regards
Hi Caroline,
It may be best to look at other hormones to see if they could be contributing to your symptoms. Not all symptoms are related to thyroid imbalances so try to look at other hormones such as estrogen/progesterone/testosterone and cortisol.
If your TSH is in range while taking levothyroxine and you are still suffering with the symptoms of hypothyroidism then you are not compatible with the hypothyroidism paradigm. This paradigm says that levothyroxine works with adequate peripheral conversion to supply sufficient fT3 to mitigate your symptoms of hypothyroidism. Either by supplements or T3 therapy, you can then move on. However, since TSH is a function of peripheral conversion, logically from axiomatic statistics, TSH ranges are not applicable to you.
I am taking 2 grains of armour thyroid daily. My TSH is .008. Free T3 2.8
Free at 4 1.08. I clearly need more than 2 grains of armour thyroid per day. My dr. Is worried that my TSH is too suppressed so she wants me to take synthroid and cytomel instead of armour. Thoughts?
Hi Allie,
This entire article is pretty much all my thoughts on the topic of suppressing TSH 🙂
Even tho my tsh is suppressed, my free t3 isnt high enough so I need more thyroid medication. I’m trying nature-thyroid now. I found a fab endo that treats based on symptoms and labs and not tsh. A miracle, I know!
Dr M. Lee at Scripps Clinic Del Mar, CA.
Hi Dr. Childs
I’m one of those people who has been told for the past 16 months by 3 different Endocrinologist that I must have a suppressed TSH because I had Thyroid Cancer.
About 8 weeks ago my Endo called me in a panic because my TSH keeps falling along with my FT4 and FT3(Endo not concerned with FT3 or FT4 numbers) shes just focusing on the super low TSH number and the dexa scan I had 2 months prior that said I have osteopenia (mild). I was told I could “DIE” with my TSH numbers being so low,yes you read that right my Endocrinologist told me I could “DIE” from heart disease or my bones would “CRUMBLE” YUP you read that right too.
I don’t agree with her since I’ve had a life long battle with autoimmune disease that has over the course of my life forced me to use steroid injections, steroid skin preps and steroid pills in order to reduce the inflammation that consumes my body everyday and to add to this issue I was just diagnoised with Psoriatic Arthritis that has attacked the tendons in my feet and ankles and now Im on another biologic drug called (Cosyntex).
My question for you is can my 44 yrs of using steroids and now another biologic and losing my female organs 15yrs ago to cancer cause my osteopenia or could it in fact be because my TSH has been suppressed for the past 16 month? I never felt any ill effects from having suppressed TSH my biggest issue is I can not lose the 35 pounds I gained after thyroidectomy when I kept off 120 pounds for over 6 yrs prior.
Do you think I should run from this Endo she unwilling to see my other health issues and only blames my low tsh for my bone health and with each reduction of my T4 meds my P.S.A. goes nuts.
Sorry so long, Grace
Hi Grace, have you investigated going on a keto diet? Consuming less than 20 grams of carbs daily? It’s worked for me with a similar story.
Hi Carla,
Keto is hit or miss in those who have thyroid issues. Some people improve while others do worse on it.
Dear Dr. Childs,
My TSH is 0.01, I am on 81.25 mg of Nature Throid, my TSH before taking thyroid meds was 0.015. My numbers are all mixed up.
However, when I wake up I take my pulse, it is usually around 75 to 77, then I take about half of my thyroid dose and 20 minutes to a half hour later my pulse is 72.
I have tested this over and over throughout the month and it always comes out the same.
I would love to hear from you about whether it is possible that the thyroid meds I take are making my pulse more normal?
Thank you,
Dhyanna Goulet
Hi Dhyanna,
Thyroid hormone does influence your heart rate and blood pressure so it is possible.
Hi Dr. Childs,
On a very low tsh (.01), is it possible for my pituitary to be malfunctioning?
Some of the other clues I have that the pituitary is not working:
1. a high urine volume with inadequate antidiuretic (comes from the pituitary) hormone. I measured my urine output, should be 2.5 liters in 24 hours, mine was 1 gallon in 24 hours and I went to the bathroom 18 times. (not normal)
2. Low prolactin (produced by the anterior pituitary) The effects of altered levels of prolactin on sex hormones are profound, substantially increasing or decreasing estrogen levels. My estrogen is very high. I am 70 years old and post menopausal.
Prolactin is responsible for fluid, sodium, chloride and calcium transport and acts on the kidneys to promote sodium, potassium and water retention. (high urine output) (I use plenty of Real Salt and ‘have low blood sodium’ and naturally eat bananas every day)
I seem to have both high and low prolactin symptoms:
painful intercourse, excessive body and face hair, breast tenderness (I cannot wear a bra anymore due to pain at the lymphatic area), loss of sex drive, low energy levels, Hashimoto’s thyroiditis.
3. Pituitary problems are very common in Mercury Poisoning. I have had a provoked test for mercury, the reference range <3, mine was 75.
I believe my pituitary is damaged, if so, and the pituitary could not produce TSH, then it seems that my TSH would be non existent.
Do you think this is possible?
Thank you so much, Dhyanna Goulet
Dr. Childs,
I had a TT in 2017 for unmanageable/reoccurring Graves. I have had a very suppressed TSH ever since the surgery (currently 0.03). My T3/T4 are all in normal range (T3 is 3.2 and T4 1.25) and not even on the “high side”. It’s a constant “battle” between my conventional Endo who wants to lower my meds (Afib/Bone loss) and my functional med doc who wants to increase my Cytomel to raise my T3 and has NO concern about my TSH.
Symptomatic-wise, I tend to agree with the functional med doc. and realize taking Cytomel suppresses the TSH. However, I sometimes worry that I am not doing what’s best longterm?
I have gained 25 pounds since surgery & have a few classic hypo symptoms but also have heat intolerance (always have) and sometimes palpitations (but MUCH better since TT and they seem to be related to eating gluten or sugar).
Given all my Autoimmune issues including MTHFR, Iron-deficiency, Vitamin D deficiency, “low” cortisol + my age (42) and peri-menopause (estrogen dominance), etc. I think I am generally feeling pretty good!
Basically – I can’t keep being pulled between the two doctors and KNOW I feel better when my T3 is higher…do you see any issue with my TSH being 0.03 & possibly lower as my Cytomel gets increased?
I love your website and information – wish we had more doctors like you in the midwest, it’s a struggle & educating yourself becomes incredibly necessary. Thanks for all the work you do to educate people!!
Hi Kate,
I’m in a similar situation as you. Our labs are almost exactly the same and I’m on synthroid and cytomel. I was wondering how it worked out for you?
I have been on natural desiccated thyroid (NDT) for the past seven years, and feel great, after suffering on T4 only drugs for ten years before that. Diagnosed with Hashimoto’s 18 years ago.
I need 5 grains of NDT daily to feel completely normal and rid myself of all hypo symptoms. My FT4 levels consistently come back midrange, my FT3 levels in range but close to upper normal range, and my TSH has been completely suppressed (<0.01) since going on NDT. I have never given it another thought as I feel great on NDT and am back to my pre-thyroid failure weight. Bone loss has never been an issue to me and, even if it was, I'd gladly risk it to be able to continue to feel the way I do now. I never, ever want to go back on T4 only again only to have a so called "in range" TSH…!
Of course, most doctors only care about the TSH and freak out when they see mine. I see a doctor working with alternative methods, prescribing NDT and other bio-identical hormones rather than mainstream drugs, and he could not care less, but my family doctor is always telling me I need to go back on T4 only and get my TSH back in range.
Despite a so called normal TSH and high in range FT4 levels on T4 only (FT3 was never tested back then) I kept feeling lousy, gaining weight, looking puffy and always feeling tired. NDT has given me my life back, and I'll never go off it even if it means living with a suppressed TSH for the rest of my life!!!
Hi Anna,
I’m totally fine with patients making informed decisions about their health. If you are fine with the potential risks involved and you feel that the risk is worth it then that is certainly your choice to make! I’m just here to provide information about the topic 🙂
Anna, I completely agree with you. I found an endo that does too! Stuck to your guns girl 😉 I’m in the same boat.
I am in menopause using estrogen patches 2X a week and compounded progesterone cream nightly. I had a bone scan that indicated all was good, I do not supplement calcium. A few months later I broke both ankle bones (literally heard them snap) and when the doc did a EKG prior to surgery to fix it, he refused to give me general anesthesia because I have a left branch block. I have had a suppressed TSH for at least five years because that was the only way to get my FT3 above mid range on my labs. These are pretty normal results for me: TSH 0.010 FT3 3.7 FT4 1.03. My hair no longer falls out, my skin is not dry, not constipated but I take magnesium to tolerance. I am overweight and can’t lose the weight on a clean Paleo diet. My nails peel and break. I have constant fatigue and some depression/lack of motivation and brain fog/cognitive issues. Also my BP and pulse are high. So I think I AM experiencing side effects of low TSH but still hypo too. Do you have any suggestions for me? Thanks.
Hi Kay,
Yes, it does sound like you may have suppressed your TSH and are now dealing with the consequences of that. There’s no way for me to figure out what is wrong with you over this medium, but if you find a doctor to help look at your thyroid, help you manage your medication, and look for other causes of your symptoms then you will be heading in the right direction.
Hi Dr. Child’s,
I was diagnosed with Hashi’s in 2015 and was treated with just T4 until July of this year. My TSH was 0.6 and I was still symptomatic. I visited an endocrinologist and he allowed me to try liothyronine (10mcg) in addition to levothyroxine (dose dropped from 100-75mcg). The difference was like night and day. The ending swore it would not help with weight loss (but in 3 months, I’ve lost 25 pounds!), my outer eyebrow has filled back in and my face has lost its puffiness. The skin on my heels was painfully dry and cracked but that resolved as well. On top of those outward things, I’ve been way more effective in my job.
The problem is that a few weeks ago, my levels were retested and my TSH was 0.06. My T4 dose was reduced to 50mcg and I don’t feel as good… I haven’t lost anymore weight, I am way more tired and the brain fog is back.
I’m even more concerned because I had my tests redone yesterday and TSH is 0.1 (better but still suppressed) and I think he’s going to want to change something again. My FT4 is on the low end of normal which seemed strange to me, as well. I’d have thought it would be on the high end.
I feel like even if I had all the scholarly articles to back me up in the world, I’m destined to go back to being sick because of the suppressed TSH and there’s not really anything I can do about it. All I can do is hope that my doctor will listen and believe me and help me. But I don’t feel very hopeful about that.
HI Dr. Childs
I’m so confused why I haven’t lost weight. My TSH is suppressed and my T4 is around 0.7… My T3 is up around 2
Do I need to get my T4 up too in order to have normal labs?
Thanks!
Hi Nik,
Balancing your thyroid is only part of the weight loss equation! In fact, most people do not lose much weight even after optimizing their thyroid medication. You can learn more about how to lose weight here:
https://www.restartmed.com/lose-weight-hypothyroidism/
https://www.restartmed.com/thyroid-weight-loss/
https://www.restartmed.com/weight-loss-naturethroid/
Hi Dr Childs, thanks for the great information and I have been following your advice for about 8 months trying to optimize my health. I recently had tests and would like your opinion.
FT3 is 7.0 – optimal range is 5.6 (using your information on how to calculate)
FT4 is 16 – optimal range is 16
TSH is .03 – reference range is .20 – 4.00 mU/L (not sure what your optimal range is on this)
Testosterone is .9 – reference range is .5 – 2.0 nmol
Tests were done 12 hours after NDT
I split my dose 3 grains in the early morning and 1.5 grains at bedtime.
I have been on NDT for 3.5 years and in the last few months finally with a ND that is working with me. Main concern is weight gain ( I had been at a stable weight for over 10 years and since I was finally diagnosed gained 35 lbs)
My sleep has improved, energy is quite good, no sleep apnea, I exercise regularly (weight training, yoga, walking).
What are your thought son the low TSH and the high FT3? Or any other comments would be appreciated.
In response to your request for comments from those who’s thyroid stimulating hormone has been suppressed exogenously, based on my own experience, I believe there is an important component not considered in the research that may be of interest to you. For me, changes in Cytomel’s manufacturer from King Pharmaceutical to Pfizer and changes Pfizer made to Cytomel’s formulation from a corn starch filler to a wheat starch filler (gluten) adversely impacted my treatment outcome and my health. I started T3 only therapy in 2006 after my labs showed I was not converting T4 to T3 and to shrink a solid, hypoechoic thyroid nodule. I did very well for nearly 5 years taking 4 -25mcg tablets daily of King Pharmaceutical’s formulation of Cytomel. However, after Pfizer bought King Pharmaceutical and the rights to manufacture Cytomel, my treatment outcome changed dramatically and my health significantly declined throughout the next five years my endocrinologist prescribed it. Although I complained to both my endocrinologist and primary care physician that I thought Cytomel was making me sick, both dismissed my symptoms as nonspecific and told me it was not the Cytomel. My endocrinologist said he believed it was a sensor mutation. In 2016, a combination of adverse dental, skin, and digestive manifestations occurring simultaneously without either my endocrinologist or my primary care physician addressing them led to my own research and my discovery my symptoms were consistent with Celiac Disease, gluten intolerance or gluten sensitivity. About a month later, I read Dr. Izabella Wentz’s advocacy efforts had resulted in Pfizer’s disclosure that a wheat starch filler was indeed used in its Cytomel formulation. Although Pfizer agreed to reformulate Cytomel with a corn starch filler in response to Dr. Wentz and a petition with thyroid patient signatures, when my endocrinologist prescribed it again 18 months later, my reaction was so adverse, it nearly killed me. The only thing Pfizer had changed was the name Monarch, a subsidiary of Pfizer, on its label. Given osteoporosis is a feature of Celiac Disease and other gluten related health conditions, if a thyroid medication containing gluten is used to suppress TSH, I don’t know how researchers can point their finger at suppressed TSH as the sole cause of increased bone loss. Shouldn’t the thyroid medication itself used to suppress TSH be a consideration in research pertaining to TSH suppression outcomes? Thank you for all your dedicated work to help Hashimoto’s Thyoiditis sufferers achieve a better quality of life. I have found the information you’ve sent me invaluable.
Hi Judy,
Great comments! While it is very true that you (and many others) are quite sensitive to certain fillers found in medications, this doesn’t hold true for the vast majority of patients.
In my experience (treating hundreds) only a select few, perhaps 1-2%, are actually sensitive to the fillers you are talking about here. In addition, the actual amount of filler/binders found in these medications is minuscule and would likely NOT contribute enough damage to the intestinal lining to lead to osteoporosis (the way that Celiac disease leads to osteoporosis is most thought to be through malabsorption of nutrients which causes deficiencies). So you can say with some degree of certainty (although not 100%) that osteoporosis in the setting of a suppressed TSH is most likely due to increased bone turnover from thyroid medication.
Hi Dr. Childs I was diagnosed a few years back with Hashimoto’s. My labs were normal (except for TPO antibodies) but was having lots of hypothyroid symptoms. I was simply monitored for awhile, but as my TSH would go high, I was prescribed T4 only. Thought I was going to die of a heart attack one night after a few doses. Stopped taking and at another time when TSH had gotten to 9.0 they tried again. Same result. Switched doctors and was given Armour. It gave me progressively worsening headaches with each dose. Stopped taking after a week and that was 3 yrs. ago. I just gave up on going to the doctor…until a few weeks ago. Now my TSH is below normal at 0.06 (.45-4.5 range) and nurse practitioner seemed unconcerned. My free T3 and free T4 were normal. She could not explain the below normal TSH. I am not on any medications at all. Could you give me some insight as to how or why my TSH is now below normal? I still have symptoms of low thyroid. I am post-menopausal. Thank you.
Hi Dena,
The TSH fluctuates on a daily basis and lab results are not 100% accurate. If the lab seems out of place then it may very well be the case that it is just an anomalous result. You’d need to retest it to be sure.
What do you recommend for a patient who is taking a combo T3/T4 medication and in order to achieve an optimal FT3 levels and symptom control results in a suppressed TSH. Such that if the dose was lowered to prevent TSH suppression, it would also result in a suboptimal FT3 and return of symptoms?
Hi Carlotta,
The best answer is to find a variation of T4 + T3 which doesn’t suppress your TSH and cause symptoms which may require alterations in individual T4 and T3 doses.
Dear Dr. Child’s,
Do you think taking a Synthroid and Cytomel combo is better than NDT for preventing suppressed TSH?
Hi Allie,
100% because you have more individual control of T4 and T3 with Synthroid/Cytomel versus the static doses found in NDT.
Dr. Westin:
My husband is 66 yrs old; he had a total thyroidectomy in 2010. Cancer of the thyroid was found as an ‘incidental find’ after a dbl bypass surgery. we have a terrible time finding a good balance. A natural practitioner removed him off Synthroid and put him on Armour Thyroid. Within a couple of weeks, he came down with Scarlet fever.
His TSH is 0.07;
Free T3 is 3.0;
Free T4 is 2.1
He is now on 150mcg Levothyroxine; what else could we try …?
Thank you kindly
Bruni
Hi Bruni,
I would take a look at this article for more information on dosing: https://www.restartmed.com/normal-thyroid-levels/
Hi, dr Childs
I am having a really hard time trying to adjust my medication. I’m 31 now. In the country I live in we only have access to T4 medications only (We don’t have access to NDT or T3 medications).
My TSH is suppressed (0.13) but my free T3 is almost in the minimum range (2.7 – the range is 2.5-3.7). I am taking Synthroid 88 mcg. I felt better when taking Synthroid 125 mcg (free T3 and free T4 were in the upper range), but my endo asked me to lower the dose because I was in subclinical hyperthyroidism (TSH was 0.01).
I really feel confused and lost about this situation. Can I keep a suppressed TSH for life?
Hi L,
You can keep your TSH suppressed but you should understand that there are potential risks associated with that choice.
Thank you so much for your answer. I have been watching your videos on Youtube and reading your posts here and they are being very helpful.
However, I am still wondering if having a suppressed TSH is a ‘problem’? Maybe people think that a suppressed TSH necessarily means that you are in a hyperthyroid state (high levels of FT4 and FT3), but it does not necessarily happens when you take Levothyroxine, as you mentioned in your video on Youtube.
If I do have a suppressed TSH but normal or optimal levels of FT3 and FT4 would I still suffer from the potential risks (bone loss and heart problems)?
In fact, aiming to support my statment, I post a part of an article from Frontiers in Endocrinology:
“Many studies reported increased risks associated with suppressed TSH such as atrial fibrillation and osteoporosis but failed to properly classify the hormone status of patients into euthyroid versus hyperthyroid, and frequently did not even distinguish between treatment-induced TSH suppression and endogenous hyperthyroidism (94). Importantly, thyroid hormones, while suppressing pituitary TSH, have been reported to upregulate the locally produced osteoprotective TSHβv variant (95). Statistical associations with TSH cannot establish causality, as the opposing effects of low-TSH and low-FT3/TSHβv frequently occur together in LT4-treated patients.
However, it is equally appropriate to stress a caveat that not every patient on LT4 may require or tolerate a suppressed TSH. Unfortunately, conventional range considerations for TSH do not apply to the LT4-treated patient. There is no easy fix, but a paradigm shift could be a first step toward a solution. Until more personalized methods such as setpoint reconstruction have been evaluated (37), treatment adequacy must be judged on an individual basis by a combination of clinical and biochemical outcomes. The frequent overlapping and unspecific nature of hypothyroid symptoms presents yet another challenge (96–99). Unfortunately, reliable and readily accessible markers of the tissue effects are lacking.”
Reference: Recent Advances in Thyroid Hormone Regulation: Toward a New Paradigm for Optimal Diagnosis and Treatment
Rudolf Hoermann, John E. M. Midgley, Rolf Larisch, and Johannes W. Dietrich
Hi L,
Yes, I tend to agree with that information. Having a suppressed TSH is not always indicative of a hyperthyroid state (though it could be), nor is having a suppressed TSH ALWAYS dangerous (though it could be). So there is no cut or dry answer as to whether it’s safe in your particular case because it depends on so many factors. My general advice, though, is if you aren’t a doctor, or trained to look for the side effects or consequences, then the risks probably don’t outweigh the potential negative outcomes of keeping your TSH suppressed for long periods of time. For instance, you should have semi-frequent bone scans and echocardiograms to check for heart/bone-related issues.
Hi, dr. Childs
Thank you very much for your time and attention!
Can speak about suppressed TSH (0.08) with a low normal Free T4 (1.0) and low normal Free T3 (2.9) in a patient on Nature Throid? The picture is confusing, to say the least. No measure of reverse t3, yet.
Hi Amy,
You really need that reverse T3 to put the picture together.
Dr. Childs- In your experience does T3 medication suppress TSH? My TSH has been “too low” but my FT3 and FT4 are still low as well (last labs TSH .005, FT3 2.2, FT4 .8, RT3 14). My low TSH always causes the doctors to reduce thyroid medication which only makes me feel worse. I am waiting to see if I have the DIO1 a DIO2 variation that speaks to decreased ability to convert T4 to T3. I have NO hyper symptoms. In your practice, do you ever see a TSH that is low due to the T3 meds?
Hi Laura,
T3 has a suppressive effect on the TSH, as do all types of thyroid medications, and the suppressive effect is dose-dependent. It’s possible to have a high TSH on a low dose of T3 medication just like it’s possible to have a suppressed TSH on a high dose of T3 medication but taking T3 medication in any dose does not automatically suppress the TSH.
Hi Dr. Childs, I am currently on slow release T3 on a dose 135mg/day and having a TSH of 0.13. For the past 6 weeks, I reduced the dosage to 120mg/day and latest TSH is 0.3. I have also had my Hypothyroid symptoms return. This all disappeared after going back to the original dosage of 135mg/day. Can you explain why Hypothyroid symptoms returned at week 4 of the 6-week trial given the short half-life of T3, I would expect to see the symptoms within a week. The second question is with respect to seeing further TSH suppression with reduced dosage? My doctor has suggested optimizing dosage to the point of having no symptoms even if TSH is suppressed and compliment with Bone scan monitoring. Thank you for sharing all your valuable resources on the internet, I think you are the goto site for all patients with thyroid problems.
Hi Peter,
The changes that occur due to thyroid medication (T3 in particular) occur at the cellular level due to changes in genetic transcription. These changes are not reliant upon the serum levels which is why most people do not need multi-doses throughout the day and why your serum levels can drop but you still remain euthyroid. If you subscribe to the idea that serum levels are the only thing that matters when it comes to T3 then you lose sight of how T3 actually works in the body.
I am never a fan of dosing based on symptoms without regard to lab tests because I think it’s sloppy medicine. There are many other conditions which can contribute to hypothyroid symptoms which cannot be solved with brute force thyroid medication.
Hello, my labs are as follows:
FT3 is 90. Ref (71-180)
FT4 1.56. (.82-1.77)
TSH .410. (.450-4.500)
I am feeling run down, aching joints and muscles, I am cold and get short of breath doing even light exercise. My Temperature varies from 96.4 to 97.4
I am taking .88 Synthroid.
From what I have read here I should get more extensive testing done.
What tests do you recommend?
This is so confusing to me.
Thank you for all do.
Hi Diana,
You can find a complete list of thyroid lab tests and what they mean here: https://www.restartmed.com/normal-thyroid-levels/
I had thyroid removed in 2010, received radiation and was put on Levothyroxine at high dose to suppress 175mcg. Now 2019, I was experiencing major symptoms and was put on lower dosages (100mcg). My GYN has taken me off all hormones, I am post menopausal. The Levothyroxine dosage was reduced in increments. At 125mcg I began feeling human again with no body aches, no hair loss, no fatigue however my TSH was still below 0.01. Doctor lowered to 100mcg. Retested @ 6 weeks and still below 0.01. At 100mcg I am feeling body aches, fatigue, etc. I fear that going lower will result in more unpleasant symptoms. We cannot seem to get the TSH above 0.01. My T4 Free is 1.30. My parathyroids were damaged during my thyroid removal and have not worked since. I take calcitriol for that. Any thoughts as to why I cannot get my TSH above 0.01?
Hi Sandy,
The TSH drops based on the dose of thyroid medication that you take. If your doctor wanted to raise it they could simply reduce your dose down to 25mcg and it would certainly raise. The reason they aren’t doing that, and the reason you certainly don’t want them to, is because if they do you will feel terrible. And this is the reason that the TSH test falls short as a measure of thyroid function.
Hi Dr Child’s,
I have been struggling with a suppressed TSH following a TT in Dec 2017. My endo keeps dropping my meds which makes my T3 and T4 drop and has very little or no impact on my TSH. I just changed drs and he dropped me off the cytomel and it has come up a little .022 to .026. FT3 is 2.23 and FT4 is .97. He also tested my PTH which came back low as well as my vitamin D. Calcium (PTH) was in normal range. What are your thoughts? Is my pituitary just having a hard time waking up post surgery? Could there be something wrong with my pituitary gland. My endo said it is very uncommon for there to be something wrong with the pituitary causing my suppressed TSH. I’m gaining weight even though I have not changed eating habits and am very active and run half marathons regularly. My energy is sluggish, my hair is falling out still and brittle. I’m so tired of this. Would your supplements help? What would you recommend? I feel like my synthroid should be increased as per my hypothyroid symptoms but the drs won’t as my tsh is suppressed. I’m so puzzled!!! And so are my doctors.
Dr. Child’s
I was told that you can’t be hyper if you have no thyroid, is this true?
I had thyroidectomy for cancer 2016 and like a lot of TT people here my TSH no matter what dose I’m on is very low and so are my ft3,ft4,t3 but I’m also plagued by autoimmune disease and inject myself monthly with immunosuppressive treatment as well as a trial run with cymbalta for horrible joint and tendon pains that have been a problem since thyroid sx.
For 2 days after my injection it does make me feel hyper and then Im normal again.
Do you think immunosuppressive drugs could cause abnormally low TSH?
Hi Grace,
No, that isn’t true. You can become hyperthyroid by simply taking too much medication. This is referred to as iatrogenic hyperthyroidism.
Hi Dr. Childs,
In response to your question pertaining to those with a suppressed TSH… My TSH has been suppressed for 12 years due to treatment with T3 only, In my case, T3 had been prescribed to shrink a solid, hypoechoic thyroid module on my right thyroid gland; I didn’t convert T4 to T3; and I developed adverse reactions to every T4 medication on the market at that time. Although I do have osteoporosis of the spine and osteopenia of the hip, it started before my treatment with T3. Due to polycystic ovary disease, I had a complete hysterectomy in 1986 and began treatment with Del Estrogen injections. In 1992, I was diagnosed with hypothyroidism and started treatment with 100mcg of T4, Levothroid. After a breast cancer research study first linked estrogen to breast cancer in 2002, hormone replacement treatment with estrogen ceased. All my annual bone density tests results were normal until January 2006, when I was diagnosed with osteopenia of the spine and hip. I didn’t start treatment with T3 only until August of 2006. It was later disclosed that Premarin, a combination of estrogen and progesterone, had been linked to breast cancer, not estrogen alone, but estrogen treatment was still not available. By 2009, I had developed osteoporosis of the spine. In 2012, I resumed treatment with Del Estrogen injections and my bone density test showed dramatic improvement in 2013. Treatment with and without Estrogen has influenced my bone density outcome. A pharmacist told me that for women without ovaries to produce estrogen, calcium isn’t absorbed and retained in the bone. Is that true? Liver disease is one of the secondary causes of osteoporosis, so although the thyroid hormone itself may or may not contribute to osteoporosis, an adverse side effect to the filler in thyroid medications can impact liver function and health if it builds up to toxic levels in the blood. I know you disagree with me on this, but thousands of patients taking thyroid medications have reported very adverse reactions to certain fillers, particularly those with gluten sensitivity and issues with mannitol. I know it doesn’t sound logical but if you look at comments on Izabella Wentz’s blog, many have reported adverse side effects to Pfizer’s Cytomel formulation change. Hyperparathyroidism and other possible causes of a patient’s low bone density should be considered rather than assume a low TSH is the culprit. I often ask this question…why is a low TSH and too much thyroid medication any more dangerous and harmful to the body than a high TSH and a chronic, severe state of hypothyroidism? I know we should all strive to reach levels in optimal ranges, but not all physicians treating patients for thyroid disease should be. My daughter, my deceased father and I all consistently tested as very low TSH levels (.01-.06) but had clinical symptoms consistent with hypothyroidism. We weren’t diagnosed with Hashimoto’s and treated until after labs came back with very high levels of perioxidase antibodies. Research studies prove or disprove specific researcher hypothesis but most of what can be learned about disease is by talking to those suffering from the disease as you have done. You have greater understanding of thyroid disease because you have done the research and are also digging in the trenches every day asking questions. Sometimes there aren’t scientific explanations for what people experience but it doesn’t make them any less valid.
Hi Judy,
I think we probably agree on more things than we disagree and there’s a lot of information to unpack in your comment but here are a couple of thoughts:
#1. Bone density is certainly impacted by both estrogen and thyroid hormone. Probably more-so by estrogen, at least in my opinion. I say that because pre-menopausal women can have a suppressed TSH without any bone-loss which makes me believe that the protective effects of estrogen overpower the negative consequences of a suppressed TSH.
#2. I don’t doubt that patients have negative reactions to fillers but when you try to make the leap from negative reactions to liver damage that’s where things start to break down. If that were actually the case then it is easily testable with lab tests such as AST and ALT which correlate extremely well with liver function and damage. I seriously doubt the connection between fillers in medications and liver damage in patients as a cause for bone loss. While it’s theoretically possible it’s extremely unlikely.
#3. I don’t believe, necessarily, that a suppressed TSH is any more dangerous than a high TSH for patients. You either risk cardiovascular disease and bone loss with a suppressed TSH or high cholesterol, obesity, and metabolic dysfunction with a chronically high TSH. It’s a pick your poison type of thing and some states are probably more dangerous for certain people based on other factors such as genetics. I don’t advocate for a high or low TSH but instead, normal thyroid function which I do believe is achievable in most patients without suppressing the TSH.
#4. I also agree that discussing information with patients is incredibly valuable and the current research does not have all of the answers. But that doesn’t mean that research becomes any less valid. The clinical studies and research provide a language which we can all follow, one that is testable, one that is reproducible, and one that will help guide future treatment. Patient information is helpful to a point, but it’s fairly useless unless it is put in the right hands with the right information. This is why, at least in my opinion, that some patient thyroid advocacy groups do more harm than good. They are well-intentioned but they are trying to push forward ideas and therapies through the wrong avenue and they will be rejected by the scientific community and physicians unless they go through the proper channels.
Szia Dr. Childs,
Több mint 35 éve diagnosztizált Graves beteg vagyok, akinek 5 éve eltávolították a pajzsmirigyét. A műtét után t4-es gyógyszert kaptam, de hétről hétre rosszabbul voltam, maga volt a pokol, életemben még soha nem éreztem annyira rosszul magam. Állandó migrén, 2 hónap alatt 22 kg hízás, napi 14-16 óra alvás, agyi köd, állandó fázás, vizesedés, hajhullás, stb. A tsh mindig 0,0.. volt, még akkor is, amikor a t3 és t4 már referencia tartomány alatt volt. Lázasan kerestem, hogy mit tehetnék, mert az endokrinológusok nem segítettek. Sikerült t3 gyógyszert szereznem, amitől már az első napokban sokkal jobban lettem. Két hónap t3 szedés után természetes pajzsmirigy gyógyszerre váltottam, ami visszaadta az életem. Nagyon hálás vagyok Önnek és a stopthethyroidmaddnes.com-nak és nem érdekel, hogy mennyire alacsony a tsh, mert újra jól érzem magam.
Hi, Dr. Childs,
Thank you for your work! I have recently had a thyroidectomy (Hashimoto’s) and the right lobe contained a very small papillary carcinoma (low risk). I have not felt well since the surgery… the main symptom is brain/mood issues. I am on both T4 and T3 (was before surgery as well). My TSH is very suppressed (.0425) with T3 in the upper third and T 4 in the middle. My Integrative Endocrinologist wants to see the TSH come up (am reducing T3) and Integrative Doctor argues with this (believes there has been major improvement on combo and does not believe in heavy risks). I tend to want to place this safe since I have a family history of cardio issues and am mist concerned with alleviating brain/mood issues.
Thank you!
K
I seem to be having a suppressed TSH on Levo T4 only but not overmedicated my t4 top half of range my t3 top end of range why is that? I know you can have suppressed TSH in t3.
Hi Dr. Childs – Subj: Months long TSH suppression possibly leading to liver issue (now mostly cleared) and Atrial Flutter (still working on). I have Hashimotos and SIBO. During the months of suppression, my thyroid replacement dose of NP Thyroid was around 1,219 mg per week. It is currently 630 mg per week. June 2018 TSH 0.08, Rt3 9, Ft3 2.5 and Ft4 0.7 /// August 2018: TSH 0.01, Rt3 16, Ft3 3.7 and Ft4 1. /// November 2018: TSH 0.01, Rt3 116 (yes, you read that right; 116), Ft3 4.4 and Ft4 2.1 with ALT of 800 and yellow in the corners of my eyes. I am not obese, I don’t drink, liver disease tests were negative and my liver ultrasound was thankfully normal in spite of the 800 ALT. /// December 2018: TSH 0.03, Rt3 (not captured, in January 2019 it was 19), Ft3 2.3 and Ft4 0.8. /// January 2019: In ER with Atrial Flutter. The liver was a mystery until I found NIH’s Liver Tox website which indicates that high doses of thyroid replacement can cause elevated liver serum enzymes. So that may be what the liver issue was. Prior to the Atrial Flutter, my heart rate was 64-66 bpm. Now it is between 120 -130. I’m on Eliquis and Metoprolol (beta-blocker). I strongly dislike being on these meds! Am waiting for my TSH to stop bouncing around because I hope that my heart rate will normalize without needing cardioversion. In spite of dose lowering, my TSH stubbornly remained 0.01 until June 2019. June TSH 0.4, July TSH 9.3 August TSH 1.13 and September TSH 0.8. My ALT is now between 68-78, but Eliquis and Metoprolol can affect that enzyme, I believe. At least it is below 100! My Albumin/Globulin Ratio is now 1.1 which is good. I’m taking liver supplements including NAC, Curcumin, and milk thistle. This has been a frightening ride. I think I’m on the mend. Just wish my Flutter would normalize. Do you have any other supplements, thoughts or recommendations? Trish
I apologize for the length of this post! As with most thyroid patients, I think I am an anomaly! I am currently 66 yr old. Three children & 10 grands. Slender build (consistent 5’7 1/2” & hovering <140lb) . Not a regular exerciser but active. On a significant number of supplements. No meds other than thyroid.
The rapid-fire incidents that were preceded by a healthy existence were: 2001 – total hysterectomy due to a basketball-sized fibroid. Complication was that the surgeon nicked an artery. I needed blood transfusion & was reopened for repair & removal of one ovary. Recovery uneventful. 2002 – total thyroidectomy due to multinodular goiter with suspicious cells. Surgeon successfully removed whole, diseased gland. In one lobe, biopsy showed <2cm of papillary cancer. I did follow-ups with surgeon for 5 years. No RAI. I went on Armour. TSH was suppressed. Again, recovery uneventful. THEN, 2005 – partial bowel resection due to fatty lipomas blocking intestines. (Of which pictures were used for educational purposes!!!) About 10 inches of lg & sm intestines removed with ileocecal valve and appendix. Again, recovery uneventful! (Although, I find eating fermented foods to be quite uncomfortable & sometimes veg – especially raw or greens – don't digest thoroughly.)
There were always adjustments to thyroid med. After the 5 yr. mark, it was thought that I could allow the TSH to migrate to around 1. At one point, I changed to NatureThroid due to inability to get Armour. Then, at random times, my TSH would rise to 10+! It became hard to get NatureThroid, having to piece together from various pharmacies the dosage I needed. The only symptoms I ever had were the darned racing heart and an intolerance for being really hot or really cold! Never weight gain or loss, hair loss, depression, whatever!!! My current dr. suggested I might try going on Levothyroxine. We decided on Tirosint due to the possible inability to absorb the med due to the loss of that 10 inches of intestine. Initially, I started on 200mcg., which seemed to be the equivalent of NDT I was previously taking.
My TSH went from 10.79 (FT3=2.3; FT4=0.8; RT3=not taken)on NT to .03 on Tirosint (FT3=4.1; FT4=2.4; RT3=27). We decreased the Tirosint to 175mcg. TSH is now .07 (FT3= 3.2; FT4= 1.8; RT3= 18). Again, no symptoms (no weight gain, no hair loss, even racing heart has significantly decreased). I still have a limited tolerance to heat or cold. I seem to have a bit of a struggle with BP which has gone down since on Tirosint. My systolic is in mid 120s, diastolic is a challenge to get below mid 90s. Pulse rate is typically in the low 90s but used to be typically in the high 90s.
My dr. thinks it would be OK to stay where I am now. I am concerned about the effect on bone mass and even heart. From what I read, I am feeling that I should go down to 150mcg. I am thinking it would be better to have the TSH be around 1.0 and hopefully lower the RT3 (although, maintaining that Free T3 since it went down with the dosage change). My dr is thinking I shouldn't have bone or heart trouble with a TSH of 0.07. The most compelling reason to change the thyroid dose would be palpitations or agitation and sweating or a tremor. She thinks it would be ok to keep me at the current levels and that I wouldn't be at risk (no suggestions of dexa or echocardiogram follow up). Am I being too skeptical? Do you have any other things I may want to discuss with her? In relation to all the surgeries I mentioned above, I have a sneaky suspicion that all this is connected but not sure how!
Thank you for all your information! I find your site to be VERY informative and helpful!
Hey Dr. Childs,
I’m a 52-year-old male. I had graves disease and had a total thyroidectomy in 2010. After the thyroidectomy, they found a very very small cancer tumor in my thyroid. Since then I have been on a TSH suppression protocol. For the first 7 years, my TSH has fluctuated between .25 – .62 with multiply dosage changes. I was up to 300mcg for the last 6 years. In the last two years, I have been experiencing symptoms of Hyperthyroidism… weak legs(quads), cramping, palpitations, heat intolerance, etc. This has gotten progressively worse over the last 2 years. I have had several TSH test done and for the last 2 years, it has been between .008-.21 and my free T4 is over 2.0. Also, my calcium level is showing in the low normal range (barely). My endocrine doctor has recently (last week) backed me off to 275mcg. I’m starting to feel a little better, but it has not been long enough to affect my total TSH.
Do you think being in a suppressed state for so many years could have caused a thyrotoxic myopathy? I’m also on testosterone replacement .5cc IM once per week. Testosterone has hovered around 500. It is concerning to me because of the weakness and cramping. I feel a lot like I did when I had graves disease.
Any insight would be greatly appreciated!
Michael
Hi Dr Childs,
My last two tests show TSH < 0.02 or 0.03 (it has been there for a while) and my doctor says that is perfectly OK, since I don't have a thyroid and the nodules I had were suspicious enough to warrant a full thyroidectomy 9 years ago. My free T4 is 1.2 to 1.3 and my free T3 is 3.8 to 4. Do I need to worry about the long term effects of a suppressed TSH and if so, what needs to be done to raise it? I am on 165 mg of NP+ 10 mg of liothyronine, and going lower will likely cause the return of many hypo symptoms. I also have monthly periods and only this year have I managed to regulate them, thanks to reaching my optimal levels. Thank you!
Hi My Thyroid had been suppressed for some time now. I was Diagnosed with Graves in Feb 2019. I was taken off Levothyroxin a year and a half ago, which I was on for about 26 yrs. My labs are listed below with the range per the lab used.
T4 Free 0.82-1.77
1/14/2020 0.93
4/4/2019 T3 Uptake 20 24-39
3/1/2019 21
1/27/2019 21
1/21/2019 20
1/7/2019 21
11/22/2018 22
9/24/2018 23
6/23/2018 23
1/26/2018 26
TSH 0.450-4.500
1/14/2020 0.729
10/18/2019 0.127
4/4/2019 0.426
3/1/2019 0.192
1/27/2019 0.198
1/7/2019 0.122
1/16/2018 0.008
5/1/2018 0.007
11/30/2018 0.053
8/24/2017 0.016
12/8/2017 0.006
9/26/2017 <0.006
Thyroid Peroxidase (TPO) Ab 0-34
1/30/2019 93
Thryoid Stim Immuoglalobulin 0.00-0.55
1/30/2019 20.90
Free Throxine Indez 1.2-4.9
1/7/2019 1.1
1/16/2018 2.6
First Graves, then RAI treatment – only minute amount, not enough to kill off thyroid altogether. Within 6 months though I had Hypothyroidism. Cut to the chase: When my TSH is in the upper limits of normal I am dull, lethargic, and very depressed, even kidney function goes down as does heart rate and probably every other bodily function. When TSH within range of 0.4-1.5 I feel okay. I did try increasing T4 medication and put myself in the subclinical hyperthyroid state. However Reverse T3 increased to 10 times normal range and same with Leptin becoming Leptin Resistant. So I also tried reducing T4 medication and adding natural T3 however even very small dose T3 gave me heart palpitations. What I have found is dosing is a journey that is different for everyone. I am finding that I am good when range of TSH is between 0.5 and 2 with noraml upper limits of FT3 and FT4. Again, everyone is different – my suggestion – keep a diary of how you feel when you try different dosing.
I don’t feel comfortable with a suppressed TSH and the symptoms you experience depend on the reason behind it. Too much T3 on Natural desiccated suppressed my TSH down to .05 and every task seemed so difficult, like gardening, because I was so hot and dizzy. I couldn’t bend down and back up without getting light headed. I was also having vision disturbances.
On the other hand one time when my TSH suddenly dropped to .74 from 1.4 on T4 only, in conjunction with a low normal FT3 level, I started to experience debilitating symptoms like neck, back and toe pain, irritability and poor sleep.
Then another time on natural desiccated my TSH was .94 but my FT3 was 2.6 and FT4 was 1.0 so I was tired and had muscle aches. Oddly I sleep better and more soundly when underdosed.
I’m currently trying and in between dose but I can’t go up anymore because it’s too much T3 for me in the higher dose and I don’t want to suppress my TSH too low.
I don’t understand the ratios of T4 and T3 in natural desiccated. I wish the doses had more T4 and not so much T3. You can’t increase your T4 without getting too much T3, which super suppresses your TSH. I don’t like cytomel either. Just 2.5 mcg of that stuff makes me feel terrible. It’s not smooth at all. It feels like a drug that’s been around for decades and never improved upon.
Hello Dr. Childs-
I am a 50 y.o. post-menopausal female that has been on Synthroid and Cytomel for years. My TSH has been suppressed for the past 2 years (<.o1) and my FT3(3.2) and FT4 (1.28) are both in the normal range. Ever since last year when I did 2 rounds of the Prolon fast in April and May, I have gained weight and not been able to lose it despite exercising daily and doing intermittent fasting. My doctor says I'm hyper but I still have all the syptoms of being hypo (dry hair, skin, and nails, inability to lose weight, constipation, brain fog, etc). I am starting to get really depressed and don't feel very good about myself. I don't know what else to do but this weight won't come off no matter what. How would I know if there's something wrong with my pituitary gland? Could that be causing this weight gain/inability to lose weight? I also found out via an ultrasound that I have 2 nodules on my thyroid, for now doctor says to just watch them but could that be causing these problems? Any suggestions on how to best proceed and/or any supplements to help are greatly appreciated. Thank you
Does your information regarding suppressed thyroid directly relate to TT papillary cancer? My TSH has been suppressed for 10 years with my latest tests showing TSH at 0.029 Free T3 at 4.38 and Free T4 at 0.92.
I am aware of many of the cons of suppressing the TSH but I didn’t read anything in your post about thyroid cancer and the reasons for suppression.
Hi Rhonda,
This information applies to everyone regardless of the reason for their suppressed TSH.
Dr Childs,
My TSH is artificially suppressed due to having had a pituitary apoplexy and a very small thyroid gland due to antibody destruction.
My TSH does not respond as it should, and has been 0.0005 for many years. Last year my dexa scan showed I had excellent bone density.. so I’m confounding my Endo’s.
I’ve compiled my DNA data and believe that I have THRb, Tg and IYD gene issues.
Just recently I increased my T3 to 70 mcg and included 25 mcg of T4. TFT levels indicate my T3 is still low in the reference range, but hey diddly, the TSH has resurrected and is 0.19..
A final question for you: is it the suppressed TSH or high in the range T4 and T3 that causes bone damage and altered hearts?
In the future I shall add in a bit more T3 to go through the winter to cope with seasonal circadian stress.
Hi Linda,
If your endo’s are confused it just means they really don’t understand thyroid physiology. A suppressed TSH only increases your RISK of developing osteoporosis but doesn’t guarantee it by any means. In addition, premenopausal women are virtually immune to bone loss from a suppressed TSH so it’s largely irrelevant if you are menstruating. The only thyroid hormone to increase your heart size is T3 and heart enlargement is reversible if you normalize the T3 so even that isn’t really something to worry about.
Hello,
Can having suppressed TSH of <0.010 while taking combination of T4 and T3 be a cause of multiple chemical pregnancies (early miscarriage)?
Hi Karen,
It could be contributing, yes.
I just listened to your video, thanks very informative. I had a partial thyroidectomy 2 years ago, my doctor raised my dosage to suppress the other half of my thyroid. I am on 125mcg levothyroxine. I had my TSH levels checked in August it is at .26, thyroglobulin level is low at 1.0. I had Hashimoto’s enlarged, surgeon removed have of my thyroid, turned out to be a small cancer. Surgery was easy. For a year and a half, my doctor didn’t change my medication. Now he wants to suppress my thyroid. I had a Dexa scan and my left hip is osteopenia. Thyroglobulin Antibodies was normal at <1. I was just unsure if I should get a second opinion? Thank you for you input.
Hi Susan,
You can get a second opinion if you’d like but it’s a standard procedure to do what your doctor is recommending. Osteopenia is common in women, it’s osteoporosis that is worrisome.
I was diagnosed with Hashimoto’s in 1999. Initially treated with T4 and didn’t improve symptomatically at all. Eventually a doctor prescribed Armour thyroid which helped a lot but I still had symptoms of an overactive immune system, which caused lots of problems. First 60 mg, then 90 mg. About 10 years in I was put on 120 mg of Armour and started feeling GREAT. Immune activation went way down, energy good. I’ve been on 120 mg for 10 years now, with a suppressed TSH (<.03) but usually low or low normal T4 and T3, so no one has been enthusiastic about reducing thyroid hormones (and I felt well, and not hyper). I'm 57, menopause 6 years ago, and now have a rheumatoid arthritis diagnosis and have been on steroids for the last 9 months, as well as other immune suppressing meds. Recent bone scans show osteopenia that has increased in the last three years. Weirdly, TSH has gone back into the normal range for the first time in years (most recently 1.69), T4 normal, free T3 normal, total t3 low. I have been very fatigued, with no other explanation for fatigue, so functional medicine doc is increasing Armour by 15-30 mg, depending on how I feel. I'm worried about the bone loss but it seems that I really do need to be on more thyroid hormone and suppressed TSH may be necessary.
Hi Florence,
You can always keep an eye on your bones with a DEXA scan! And, if it becomes an issue, you can use other treatments such as bio-identical hormone replacement therapy.
With suppressed TSH <0.1 and low normal FT3/FT4 on NDT along with RT3 ~ 12-15 and many hypo sx, is it wise to try a dose reduction? I’m always thinking with my sx I need an increase but increasing the dose doesn’t seem to help.
Hi Molly,
It’s hard to say without a lot more information but, in general, if you are still feeling hypothyroid while using a suppressive dose of NDT then there’s probably some other factor or condition that is being overlooked.
Hi Doc!
I had a thyroidectomy almost a year ago and have been battling on the right level of levothyroxine to take. We introduced liothyronine 5mg about 6 months ago and my levels seemed to have started to get in the right spot. I was at 100 mg levothyroxine for about 3 months but I went and got my tsh level checked and it was below normal. My doctor was concerned about it being suppressed so she sent over a prescription for 75 mg. I was experiencing irritability, extreme fatigue, constipation, feeling hot but cold and clammy to the touch. Now I have been experiencing worse feelings of feeling over heated but super cold and sweaty to the touch to the point of feeling like I could pass out. Dizzy and nauseous. Headaches almost daily. And instead of being constipated it’s like my bowels did a 360 and it went the other way and has been like that now for over a week. I’m getting frustrated and I just want to start feeling normal (whatever that is)!
Hi Ashley,
By itself, a suppressed TSH isn’t necessarily concerning (though it can be). Doctors suppress the TSH of thyroid cancer patients that are post thyroidectomy all of the time which is why we know it’s at least somewhat safe. It does sound like your thyroid symptoms are not managed at your current dose, though, which is more of a problem than your TSH level.
Hello Dr. Childs,
I am a 73 yr old postmenopausal woman. I have been on armor thyroid for at least the last 10 years. Also taking bio identical hormones. I had a stroke last year and so I am off the hormones now. The Doctor who was regulating my thyroid and HRT retired and I am with an endocrinologist now. He changed me to levothyroxine. My thyroid has been suppressed for all these years. I didn’t know what that meant until I came to the endocrinologist. my TSH is .010 on the Armour and the levothyroxine. Yet my T4 is low but normal. he doesn’t test T3 because he says it fluctuates. He has lowered my dosage and the TSH has gone up .to 587 on 50 mcg of levothyroxine. I feel awful. Depressed, lethargic, can’ think clearly and have gained weight. In other words I’m hypo, yet my TSH is very suppressed. He says he’ll put me back on Armour Thyroid equivalent to the dosage of the level thyroxine as long as it doesn’t suppress my tsh. BTW, I never felt hyper. I am not optimistic this will help, but after reading your blog I am concerned that my TSH is so very suppressed. I don’t know where to turn. Any advice would be appreciated.
Hi Elaine,
Figuring out if you want to suppress your TSH is a game of pros and cons. There are many situations in which the potential risks of suppressing your TSH outweigh the potential negative side effects. This framework seems to work the best when thinking about whether or not to suppress the TSH.
Hello Dr.,
I am a 56 year old male and not on any prescription medications, but after reading many of your articles I truly think I may have hypothyroidism with suppressed TSH. (Low energy, brain fog, long injury recovery, cold intolerance, weight gain) My recent blood work came back with good numbers for most all checks except for suppressed TSH ( <0.005). Testosterone was about 700 which I believe is good for my age. Is this a Pituitary problem? I haven't yet checked FT4 & FT3 and will be soon. What else should I be asking my doctor about this. Wondering if this could be a Pituitary tumor. Do you have any thoughts or suggestions?
Hi James,
It’s hard to say without more information. The first thing you’d want to rule out, though, is hyperthyroidism or subclinical hyperthyroidism. You can do that by checking for thyroid-stimulating antibodies as well as other thyroid antibodies.
I have been hypo for 27 years following pregnancy. I have been on Armour for several years, previously on Synthroid too, but not now. The last few years I have experienced increased heart issues, but stress echo was normal. NONE of my doctors EVER linked my heart symptoms to my thyroid. Now I am realizing that the T3 may be causing them. My TSH has been suppressed for several years, although both my FT3 and FT4 are low. I just saw a new naturopath due to having just moved, so I will discuss this – I am so frustrated and scared that now I have heart damage. Should I go back to just T4 meds? I previously had trouble converting to T3 which is why I had added Armour in the first place.
Hi Dr. Childs,
I have been dealing with secondary or tertiary hypothyroidism for 5 decades over about 40 years. I am 54 and healthy. I have been fully dependent on Armour the majority of the time and still am today. I am being challenged by my current doctor and would like to find a new Doctor that is wise and knowledgeable in this area. Do you know of any you can recommend in the Bellevue, Seattle area? Are you ever available to have a conversation?
This has been my cross to bear in life starting at age 16. I would like to see if my TSH would kick in, but am terrified and can only do this under the supervision of a REALLY GOOD DOCTOR.
Thank you, Lori
Hi Lori,
I don’t know anyone in that area but you can use this resource to help you find someone local: https://www.restartmed.com/how-to-find-a-doctor-to-treat-your-thyroid/
Hi, I have recently been diagnosed with Graves Disease. My thyroid levels were found to be abnormal during a routine blood test. I have no symptoms so have declined to take any medication. My TSH level was below 0.008 my T4 16.8 and my T3 was 6.3.
A 24 hour heart monitor should nothing significant and my bones showed that I was slightly osteopoenic. I am a 65 year old post-menopausal woman. I have asked to be monitored annually for the time being and am taking calcium supplements. I would value your thoughts on my case.
Hi Dr. Childs
I am 35 years old, I have hashimoto’s, I have fixed some gut problems, like killing Blasto, my TSH is 2.5, I exercise every day on an empty stomach, I take probiotics, I have improved a lot the reduction of hair loss, I follow an anti-inflammatory diet but for the first time I am having a hard time losing a lot of weight. Should I consider starting thyroid medication?
Thank you very much.
Hi Cecilia,
It may be necessary but you’d want to get a complete set of thyroid labs first before determining if you need it. You can learn more here: https://www.restartmed.com/normal-thyroid-levels/
I was just diagnosed with Osteoporosis at 57. I have had Hashimotos for a very long time and have had a suppressed TSH for many years. I use over the counter thyroid supplements from New Zealand grass fed cows (Nutri-Meds) and they have done a wonderful job managing my symptoms. But now that I have Osteoporosis I am very concerned. I also have low vitamin D. My Dr. recently told me to get on D3 and Calcium supplements. I have started taking D3/K2 (5,000 IUs per day) along with Magnesium, but I have not added any calcium supplements yet because I have seen conflicting information about calcium supplements and thyroid meds/bone loss/heart issues, etc. I would really like your opinion on what supplements I should be taking and how much. Can you recommend a good combination of D3/K2/A/Magnesium and Calcium (if needed) and how/when they should be taken? Thank you! You are the only thyroid Dr. I trust to be honest.
I am 57 years old and I’ve had Hashimoto’s since I was diagnosed at 20 years old. I take brand only Synthroid 112 MCG every morning I was recently told my TSH is suppressed. Here are my most recent lab results. I am totally confused as to how I should be treated. Do you think I need a T3? Am I having trouble converting?
Free T3 = 3.10 range (2.40-4.80)
Free T4 = 1.49 range (0.60-1.60)
TSH = 0.247 range (0.450-5.330)
I have an appointment with my endocrinologist next week. And unfortunately, I have zero faith in her. Why is it so hard to find a good doctor to help us in the day and age you have to be your own advocate and it shouldn’t be.
Hi Shannon,
It has to do with entrenched dogma and the sole reliance upon TSH and levothyroxine monotherapy. It will likely change in the future, but it will probably take 10 years or longer.
You can learn more about how to find competent thyroid doctors here: https://www.restartmed.com/how-to-find-a-doctor-to-treat-your-thyroid/
And why I generally do not recommend seeing endocrinologists here: https://www.restartmed.com/endocrinologist-for-thyroid/
Dr. Childs,
Do you have an article about suppressed TSH and hypothyroidism after TT in 2010? My TSH has been suppressed since my surgery.
Hi Rhonda,
I don’t believe I have one specifically addressing post thyroidectomy, but the information only really changes if you’ve had your thyroid removed for cancer. And even then, it’s not by much.
Dr. Childs,
I’m so glad I found your website and all the information you have regarding thyroid stuff. My thyroid was completely removed 15 years ago due to cancer. My TSH has been suppressed since. I had a bone scan done 9/2021 and there was no sign of osteoporosis. I have started my menopause journey in the last 6 months. I was taking 180mg of Armour Thyroid and I felt great. My endocrinologist was concerned and basically threatened to not be my doctor if I didn’t get my TSH up and lower my dosage. My TSH has been <0.01. My T4 Free has been 1.1ng/dl – 1.3ng/dl consistently, My T3 has been 93ng/dl to 123ng/dl consistently, Thyroglobulin AB <0.4u/ml, Thyroglobulin <.10ng/ml. My Dr. has had me decrease my dose down to 150mg for 6 weeks, take labs, TSH still suppressed and then had me decrease down to 120mg and I am due to take labs next week. I would love to know your thoughts on the TSH being suppressed. Unfortunately my Dr. only looks at the TSH and is concerned about heart attack, although I have no history or family history of that, and bone loss. I had no heart palpitations either on that dosage.
Since the decrease of medication I am now experiencing symptoms of hypothyroid such as significant decrease in bowel movements, cold all the time, tired, weight gain, dry skin, more emotional. I was not experiencing any of those symptoms when I was on the higher dosage. And I was not experiencing hyperthyroid symptoms either. Please help.