Can you actually treat PCOS naturally?
The answer is a resounding yes, but you need to know where to start and how much attention you should put into each area.
This guide will walk you through the most important steps to treating PCOS as naturally as possible.
Including what kind of diet you need, how to supplement correctly, how to manage your exercise routine, how to reduce stress, and much more…
Managing PCOS & Your Symptoms
PCOS can be incredibly difficult to treat if you don’t have the right approach.
And the right approach means going after the root cause.
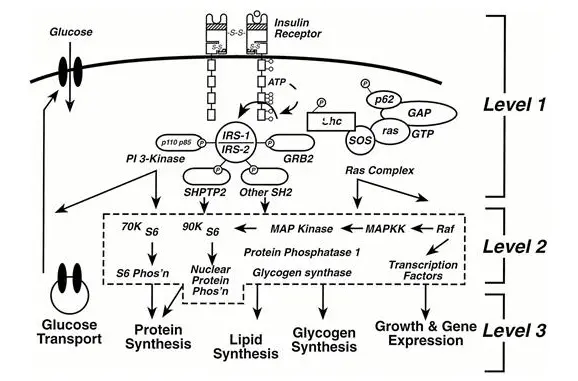
In most women PCOS, and the symptoms of PCOS, are caused by hormone imbalances that are often triggered by one hormone in particular – Insulin.
Insulin resistance sets off a chain reaction that leads to high testosterone, high estrogen, and low progesterone… and then the symptoms of PCOS soon follow.
These hormone imbalances are directly responsible for infertility, weight gain, acne, hair loss, and extreme fatigue.
The conventional approach to PCOS treatment is to cover up or mask these symptoms, but taking this approach rarely results in a lasting improvement (I’m talking to you about birth control pills and antidepressants).
Instead of masking your symptoms, you need to focus on the CAUSES of these imbalances.
Only then will you start feeling better.
So is treating PCOS naturally possible?
Yes, but you will need to take an aggressive approach and treat the following areas to the best of your ability.
Doing just 1 of the recommendations below will likely NOT result in the improvement you are looking for.
#1. Change and Optimize your diet
Probably the single most important thing you can do to help naturally heal your body is to focus on your diet.
Believe it or not, this is actually easier said than done.
Why?
Because most of you believe (wrongly, I might add) that simply changing your diet is enough to completely reverse the symptoms of PCOS.
This leads patients down a path where they constantly change their diet in hopes that they may find the mystical percentage of macros they need to lose weight or the elusive special diet that helps reduce their insulin levels as no other diet can.
While diet is critical for managing PCOS it is certainly NOT the only treatment, nor should it be your main focus.
You should put an equal amount of time and effort into other areas of your treatment including all of the areas below (with emphasis on stress management, exercise regimens, dietary guidelines, and sleeping patterns).
But we will talk about more of those in detail later, for now, we want to focus on your diet.

So what can you do in terms of diet to help naturally manage your PCOS?
You should live by these simple guidelines (regardless of the diet you choose):
- Eat whole organic-based foods
- Avoid ALL processed foods
- All carbs are not necessarily bad (certain people WILL need more than others even if you have insulin resistance but note this is an advanced concept)
- Sugar should be eliminated from your diet
- Special attention should be given to dairy and gluten-containing products though not all patients necessarily need to be gluten-free/dairy free
- You need to learn when to eat and when NOT to eat (again another advanced concept and you can learn more in my 60-day weight loss bundle & guide here)
So here’s the deal…
These guidelines should be applied to whichever diet you choose from the approved list below.
There isn’t one that is necessarily better than the others because they can all be used in certain situations (depending on your hormones and medical conditions).
Further tweaking and fine-tuning of your diet may be necessary, however, and this is why doing this part alone can be difficult.
Remember you will have to further micromanage your diet and macromolecules based on these factors:
- Special attention should be given to leptin and insulin – you may need to carb cycle and/or protein cycle
- Adrenal-related problems and extreme fatigue (higher amounts of healthy carbohydrates may be necessary initially)
- Other hormone imbalances like hypothyroidism
- Existing metabolic damage (meaning a lower-than-normal metabolism from a history of recurrent yo-yo dieting)
The presence of these conditions necessitates slight changes to your overall diet and may require changing your macromolecule ratio over time.
Once you’ve taken into account these changes you can fit them into a dietary structure like the ones listed below.
Diets that are considered “approved” for PCOS include:
- Strict paleo-type diet (including other less strict diets)
- Nutritional ketosis
- AIP (depending on the presence of autoimmune conditions)
- Low protein diets (based on the presence of leptin resistance)
- Gluten-free, dairy-free, soy-free (based on the presence of thyroid antibodies)
- Low FODMAPs and/or diets designed to treat intestinal bacterial or fungal overgrowth
You will have to use a combination of dietary guidelines, and macromolecule ratios and make changes specific to YOUR body.
I recommend that you do this with a health coach because it can be very difficult to manage on your own and does require some degree of trial and error.
#2. Exercise intelligently
Exercise is definitely up there in terms of importance (although not quite up to snuff with dietary changes) and most people do this wrong.
Traditionally you were taught that you need to sit on the treadmill for hours and hours to burn calories and lose weight.
It turns out that as many as 20% of people will get very little benefit from this type of exercise (meaning no weight loss or hormonal changes).
Instead, you should be focusing on exercises that actually impact your hormones and lean skeletal muscle.
So which types of exercises am I referring to?
Your focus should be on two main areas:
First:
Shorter and more intense exercises.
Second:
The building up of lean muscle mass.
You probably already know about high-intensity interval training, but what you may not realize is WHY it is so helpful.
This type of exercise causes rapid glycogen depletion of your body by bringing your muscles to exhaustion and it is THIS trigger that we are interested in.
Why?
Because as muscle glycogen levels are cleaved due to high demand your body must reuptake that glucose and it is this process that sensitizes your body to insulin.
And the sensitization of your cells (especially muscle cells) to insulin is what REVERSES one of the main causes of PCOS.
This is WELL known in the literature and there are studies that recommend every woman with PCOS should be treated for insulin resistance regardless of blood sugar and insulin levels.
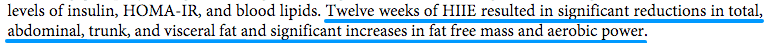
Treating insulin results in a drop in circulating androgens (lowers your testosterone) and helps you lose weight.
Building up muscle mass is obviously important because the more muscle mass you have the higher your resting metabolic rate will be (1).
Lean muscle requires tons of energy to sustain (just to move your body around and function all day long) and is one of the few ways that we can actually heal a damaged metabolism.
Having said all that, a few words of caution:
You need to make sure you manage your exercise level with your current energy levels.
If you overexercise you risk damaging your body further.
Remember that exercise IS a stressful condition on your body and that’s why it can help improve your overall physiology.
But, it’s a ‘controlled’ stress in the sense that we only want to cause damage if we KNOW you can tolerate it and recover from it.
Excessive exercise (which is all too common nowadays) can harm your body long-term and make healing difficult.
Too much exercise results in high and/or low cortisol levels and the manifestation of fatigue throughout the day (especially post-exercise).
Another tip worth mentioning is that you can try to cycle-sync your workout to match your hormones throughout your cycle:
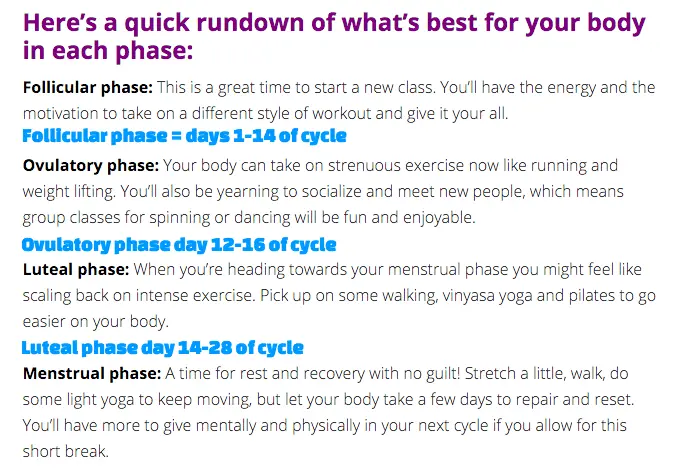
During days 1-14 of your cycle (assuming it’s normal) women tend to have more energy and can tolerate more high-intensity-based exercises.
Towards the end of your cycle (the last two weeks) you might find more benefit to slowing down your workouts to include exercises like yoga or pilates.
#3. Supplement Wisely (and for your hormones)
Just like diet and exercise I consider supplements to be a cornerstone of PCOS treatment.
Let me be clear about something though:
While most women will benefit from using supplements, some women with more advanced PCOS symptoms may also need medications in addition to supplements.
If you do decide to use supplements (I recommend that you do) you want to make sure you focus your supplementation wisely.
Nowadays pretty much everyone is trying to convince you that they sell the best supplements on the market.
Instead of focusing on hype, focus instead on the physiology and WHY certain supplements may be beneficial.
At the root of PCOS is the concept of hormone imbalance and that is where you should focus your supplement strategy.
Hormone imbalances are responsible for almost ALL the symptoms of PCOS (I’ve written about this before in this post).
You already know about insulin levels, but there are more hormones you will want to manage as well and I’ve included them below.
Focus your supplementation on the following areas:
- Reduces and reverses insulin levels
- Improving the elimination of estrogens and estrogen metabolites
- Lowering androgens and testosterone
- Lowering leptin levels
- Lowering inflammation
I could write entire articles about each one of these topics and why they are important so for the purpose of this article I will only briefly focus on targeted supplements and provide links to other articles if you want to expand on the subject.
Supplements designed to help insulin levels:
- Alpha lipoic acid: ALA helps sensitize your body to insulin and can help lower blood sugar levels. Use up to 1,800mg per day in a sustained release form for best results. Use up to 6 months for best results. You can read more about how ALA helps with weight loss here.
- Berberine: Berberine can help lower hemoglobin A1c as much as metformin and has also been shown to help with weight loss in patients with insulin resistance. Use up to 2,000mg per day for best results and for at least 3 months. Read more about how to use berberine for weight loss here.
- Glucomannan: This viscous fiber helps reduce the absorption of carbohydrates into the bloodstream, helps fill you up faster and can help with weight loss. Use 4 tablets 15 minutes before a meal with a large glass of water for best results.
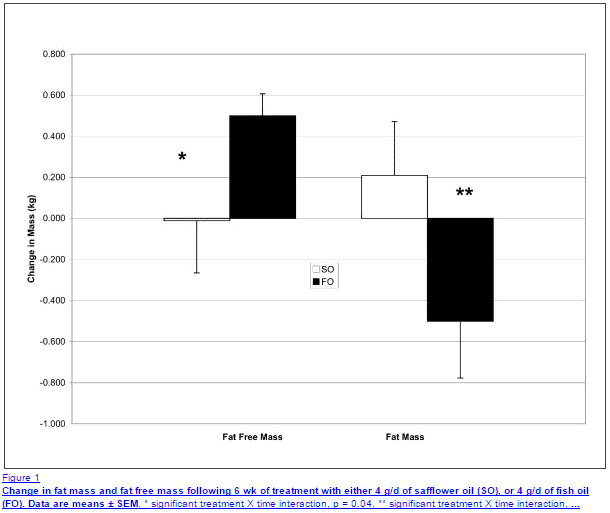
- Fish oil: Fish oil can lower insulin resistance by lowering inflammation and directly lead to weight loss and an increase in lean muscle mass if used at high enough dosages. You will want to use 2-4 GRAMS per day to get this benefit.
For best results, you will need at least 2 of the listed supplements used for several months and at high enough dosages.
Read this article for more information on managing insulin levels.
Supplements designed to lower estrogen and estrogen metabolites:
- DIM & Indole 3 carbinol: DIM and indole 3 carbinol both help reduce the influence of estrogen on the body by helping your body eliminate estrogen into less estrogenic metabolites. DIM is the active ingredient in brassica vegetables and is one of the reasons why broccoli can help women with PCOS. Take up to 300mg per day for at least 3 months.
- Calcium D Glucarate: Calcium d glucarate helps your body eliminate estrogens and androgens by increasing liver metabolism and elimination. This supplement can also help to improve liver function more generally and increase the elimination of endocrine disruptors. Use up to 3,000mg per day for best results.
Read this article for tips on how to manage estrogen levels.
Supplements designed for lowering testosterone:
- Zinc + Saw Palmetto: Zinc and saw palmetto help reduce the EFFECT of testosterone by reducing the conversion of testosterone to DHT. This reduces androgenic activity and can help reduce acne, hair loss, and mood swings. Use both in combination with one another: 60mg of zinc per day and 600mg of saw palmetto for best results.
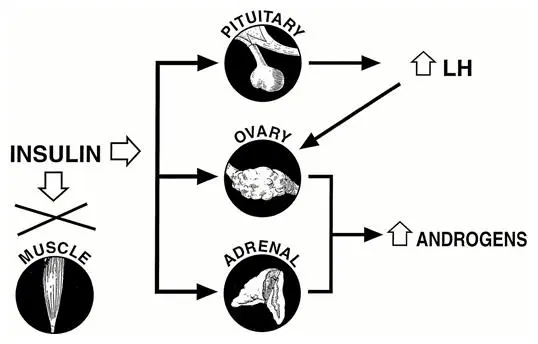
(Image shows how insulin directly stimulates ovarian tissue and adrenal tissue leading to high testosterone and DHEA levels.)
Read this article for more tips on how to reduce testosterone and androgen levels.
#4. Reduce and Manage your Stress
Another very important aspect of managing PCOS is the management of stress.
This is probably one of the most difficult aspects of your life to manage simply because people don’t tend to appreciate the negative effects that stress has on your body.
And when I’m talking about stress I am not just talking about huge disasters like moving, losing a job, or getting a divorce.
I’m talking about the day-to-day stresses that build up over time, things like getting stuck in traffic, fighting with your spouse, your children getting sick, paying bills, etc.
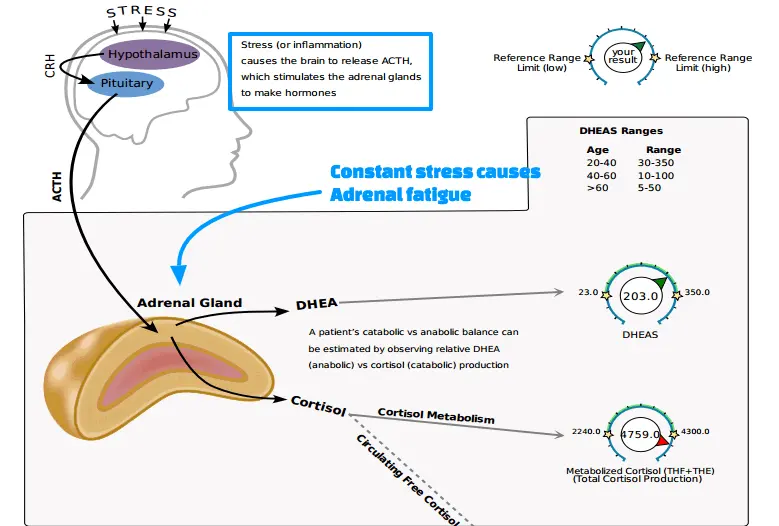
All of these small stressors stack up in your body and manifest as changes in serum cortisol levels.
Stress has even been associated with weight gain (2), hormonal imbalance (3), the triggering of autoimmune diseases (4), and leading to premature death (5).
Make sure you make managing stress a PRIORITY.
That means making a conscious and concerted effort to do one or more of the following therapies:
- Listening to music that activates delta waves prior to sleep
- Getting 8 hours of quality sleep EACH night
- Making an effort to eliminate toxic relationships or people from your life
- 20-30 minutes of yoga or meditation each and every day
- 1-3 days per week of quality exercise
- 30 minutes per day of activities that you find relaxing and enjoyable (horseback riding, hiking, swimming, etc. – something that YOU love)
- Signing up to work with a health coach or life coach
- Mentally changing how you manage stress, how you internalize stress, and how long your thoughts stick with you each day
As you can tell some of these things are much easier than others and that’s by design.
Some therapies will necessitate a coach or some kind of tutor to help you while others you can do starting today.
The bottom line?
Pick 1-2 therapies on the list and do them EACH and EVERY day.
You will start to notice a difference within 3-4 weeks.
#5. Be mindful of other Hormones
When you have a medical condition like PCOS it’s easy to get caught up in thinking that every problem you may be experiencing is directly related to PCOS.
It’s easy to think that because your PCOS caused or lead to weight gain that it must be causing the extra weight you are currently gaining.
Instead, you need to consider that your body is a complex connection of hormones and when one system is out of place the others will soon follow.
This means that you likely have a combination of hormonal problems contributing to your current symptoms.
Avoid getting tunnel vision and focusing on estrogen/progesterone and instead make an effort to look at other hormones and treat those with the same attention as you give to others.
Other hormone imbalances commonly seen in PCOS include:
- Leptin resistance – Check fasting serum leptin level. Fasting leptin should be less than 12. If you are overweight and your leptin level is greater than 12 you have leptin resistance. Leptin resistance greatly contributes to weight gain and makes weight loss very difficult if not managed correctly.
- Insulin resistance – Check fasting insulin levels which should be less than 5 in the optimal state (12 hours fasting). High fasting insulin levels indicate insulin resistance and should become your #1 or #2 priority in terms of treatment. Lowering insulin levels will help lower testosterone and balance sex hormones like estrogen/progesterone. It will also lead to weight loss.
- High testosterone – Check both free and total testosterone levels. Optimal ranges vary but should fall within the middle of the reference range. Most women with PCOS have high free testosterone and normal-ish total testosterone.
- High cortisol (and low cortisol sometimes) – Check an 8 am serum cortisol level. Optimal levels should be between 14-16. Anything outside of this range of cortisol issues may be contributing to your current energy levels.
- Hypothyroidism – This one is complex, especially because PCOS and hypothyroidism are linked, but make sure to get the following lab tests: TSH, free t3, free t4, thyroid antibodies, sex hormone binding globulin, and reverse t3.
- Low progesterone – Most women with PCOS will have a postmenopausal level of progesterone (even if they are menstruating!) so it’s not hard to miss. Levels less than 1-2 are fairly normal and should be treated.
This can actually be more difficult than you think because the current treatment paradigm of PCOS focuses only on estrogen/progesterone levels and on insulin levels.
This means you may be in a situation where you have to ask for certain lab tests or do some digging on your own.
Because this may fall into your lap I’ve included some information on how to assess these hormones via lab testing above.
#6. Avoid medications that only mask symptoms
Because most providers aren’t good at reversing the symptoms associated with PCOS the conventional approach has been to basically cover up the symptoms whenever possible.
This is usually done by using birth control medications or antidepressants.
The idea is something like this:
Well if your cycle is abnormal, heavy or you are bleeding too much we can just prevent the cycle from happening to you don’t experience those symptoms.
When in reality the presence of those symptoms is an indication that SOMETHING is off.
In this particular situation, you are basically covering up the warning signs from estrogen/progesterone imbalances and preventing them from occurring.
What you are not doing is actually treating the primary problem.
The same thing is true with anti-depressants…
The logic is if you are having issues with PMS and mood changes, then let’s just prevent large swings up or down with the use of antidepressants so you experience more flat emotions.
This is the recommended treatment over simply altering your hormone levels to try and alleviate the influence these hormones have on your mood.
The bottom line?
Try to avoid any treatment that is simply masking the current problem.
Hiding the problem does nothing for your long-term treatment and may, in fact, cause further issues down the line.
For instance:
The use of synthetic hormones like in birth control pills has been associated with a higher risk of breast cancer long term (6).
#7. Know when to use prescription medications
And finally…
Knowing when to take medication is just as important as knowing when you should avoid certain medications.
It’s worth pointing out that not all patients have the same “flavor” of PCOS.
Meaning some people may fall on the “difficult to treat” spectrum indicating a deeper level of hormonal disruption.
In some patients following all of these recommendations won’t be enough to completely reverse your symptoms in which case the use of medication may be necessary or helpful.
Pretty much no matter what, if you are able to follow these recommendations then you will notice SOME improvement.
But the degree of improvement will depend largely on your body and your hormones (and it’s difficult to predict).
In situations where lifestyle modifications and natural treatments are insufficient, you may need to look to medications to help lower both insulin and leptin levels.
You might also want to consider the use of bio-identical hormones such as progesterone to combat high estrogen levels – but this should be evaluated on a case-by-case basis.
#8. Manage inflammation
Another important factor when treating PCOS is the management of inflammation.
Inflammation plays a very important role in hormone function, which is why I’ve included it here.
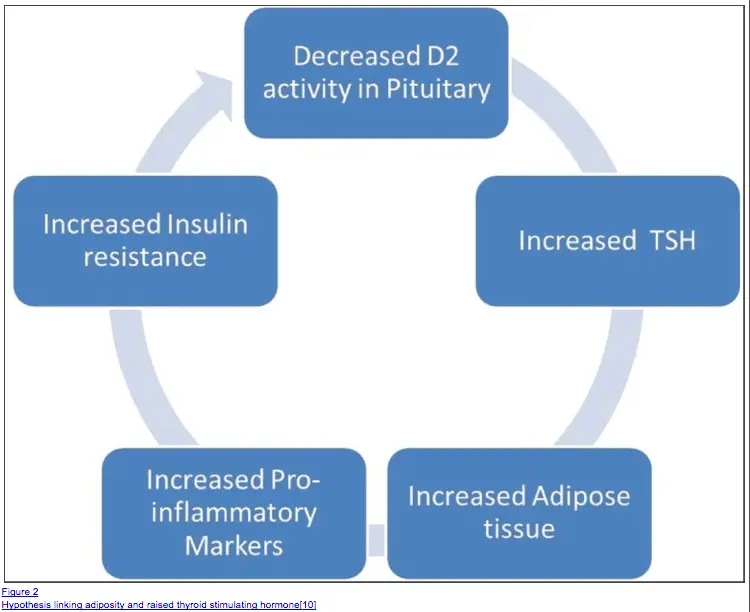
High levels of inflammation promote hypothyroid-like states (7) through the conversion of T4 to reverse T3.
Inflammation also leads to weight gain, insulin resistance, leptin resistance, and cortisol receptor resistance (8).
What’s even more interesting is that there is strong evidence pointing to the fact that PCOS is an inflammatory condition.
Meaning that the hormone imbalances that lead to PCOS lead to inflammation (9) in the body which can further worsen hormone imbalances in a vicious cycle.
Unfortunately, inflammation is a rather broad term and doesn’t necessarily mean anything by itself.
But we do know that you don’t want inflammation in your body if you have PCOS.
What does this mean for you?
It means you should check your inflammatory markers (CRP and ESR) and if elevated then go on a hunt to find what might be causing inflammation in your body.
If you can find the culprit and eliminate it, then you will directly help balance your hormones.
But finding the source of inflammation can be difficult.
Below I’ve included some common places where inflammation can hide:
- Hidden or low-grade food intolerances – you will need food testing to determine if this is the cause
- Overgrowth syndromes like small intestinal bacterial overgrowth or small intestinal fungal overgrowth
- Chronic infections like H. pylori, CMV, EBV, or other viral infections
- Hormone imbalances themselves like insulin resistance
- Poor diet, or a diet high in processed foods
- Autoimmune conditions like Hashimoto’s thyroiditis
- Bottom line: Check for inflammation and treat aggressively if present. Inflammation can worsen existing hormone imbalances and lead to weight gain.
#9. Treat your Thyroid
Another very important aspect of treating PCOS is identifying if hypothyroidism or Hashimoto’s is ALSO present.
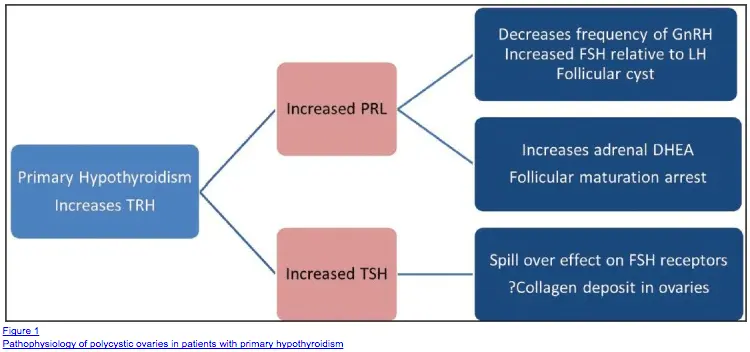
In some ways, hypothyroidism and PCOS are really on the same disease spectrum (10).
In fact, hypothyroidism can lead to many of the symptoms associated with PCOS such as infertility, ovarian cysts, susceptibility to insulin resistance, and so on.
If someone suspects the presence of PCOS then it’s necessary to rule out hypothyroidism as the cause of those symptoms.
In my opinion, many cases of hypothyroidism are really misdiagnosed as PCOS leading to the wrong treatment for that given patient.
The reason for this misdiagnosis is the heavy reliance upon TSH as the marker for assessing thyroid status in the body.
Even suboptimal thyroid levels (or iodine levels) can lead to suboptimal thyroid status in the body which initiates a cascade of symptoms that closely mimic PCOS-like symptoms.
So why don’t all hypothyroid patients have PCOS symptoms?
You have to consider that EACH of you is an individual and therefore may react slightly differently than someone else, even under the same hormone imbalances.
You don’t look like your neighbor, you don’t smell like your neighbor (good or bad!), you don’t have the same eye color or hair color, and you don’t even like the same foods, so why would you have the exact same symptoms or present in the same way?
You wouldn’t…
This genetic variability leads to various symptomatic presentations for individuals and may be part of the problem in treating and diagnosing PCOS.
If you want to be evaluated correctly you will need to find someone who understands a more nuanced approach to thyroid diagnosis and management.
You can read more about this subject here.
Essential oils for PCOS
Do essential oils have any place in treating PCOS?
While I don’t believe that you should use an approach to treating PCOS which focuses solely on the use of essential oils, it might not be a bad idea to include them in conjunction with the other therapies listed above.
One essential oil stands out above the rest: Lavender oil.
Lavender oil has been shown to help reduce stress, lower cortisol levels, and may help reduce anxiety (11).
Using lavender oil may be helpful provided you use it as an aromatic therapy delivered through diffusion.
Placing a diffuser by your bed at night, if used while listening to music designed to activate delta waves, can be a powerful stimulus to reduce stress and help calm your mind.
Essential oils won’t have a direct effect on your hormones necessarily, but they can indirectly help you manage them by reducing your stress.
Wrapping it up
Remember that PCOS can be treated with or without medications, provided you have the right approach.
If you are sick of dealing with the symptoms associated with PCOS then consider taking advantage of the recommendations listed above.
I have personally helped many patients with PCOS or on the PCOS spectrum reverse their symptoms using many of these strategies.
Now it’s your turn:
Do you have PCOS?
What treatments have worked for you? Which treatments haven’t?
Leave your comments below!








Hi Dr. Childs,
I’m 26 years old, and was recently told by my doctor that I may have PCOS – my primary symptoms are: high testosterone, hypoglycemia, mild acne, and frequent mood swings. However, I haven’t really gained weight, and have always been slender and healthy. I’m going to get a pelvic ultrasound to see if any cysts have developed, which should give a definitive answer as to whether or not I have PCOS.
My question is – have you come across patients that are young, healthy, active, etc. and are still diagnosed w/PCOS? Or could it be something else that’s causing the high Testosterone?
Hi Meg,
Yes, young women who are fit and healthy (lean even) can still have PCOS.
Meg, thx for asking this question. I’m 23 & was diagnosed w/ the very same stats as you & I’m scheduling an ultrasound to confirm. I’ve always been super lean & find it hard to gain weight. The primary concern for my testing is infertility.
Hi Dr. Child’s,
I am 40 years old and have been told I have PCOS. The only symptoms I have are high DHEA, low progesterone (at day 18 of my cycle) and weight. I am 5’2″ and weigh 150. 30 lbs of what I weigh is muscle 70 lbs of what I weigh is water and the remainder is fat. I am considered 20 lbs over weight. No matter what I do I can’t budge in weight. I am not tired, have not been on the pill for 7+ years and have a regular 28 day cycle. My cycles are. It painful, and they are regular. According to other tests I have had, I am boaderline iron deficient, T4 is not converting to T3 at the rate it should and my D3 is at around 38. I feel great and exercise 4-5 days a week. 45 min HIIT training, meditate, and eat well, but I have noticed I have had 4 injuries in the last 1.5 years-which is what prompted the blood work. All injuries are muscle and tendon related…tennis elbow, sprained wrist, stained calf and now strained quad. I can’t catch a break. I eat really well, as I have an intolerance to wheat. Do you have any suggestions on what direction I should go??
Hi Tracy,
If you feel like you have the basics down then you might be interested in learning more about advanced therapies for weight loss: https://www.restartmed.com/hormone-mastery/
Can you take all these supplement together? DIM & Indole 3 carbinol, Calcium D Glucarate, Zinc Saw Palmetto, Berberine
Alpha-Lipo, etc… In recommended doses of course.
At 27 I was recently diagnosed with PCOS after several years of being told I was simply irregular by several doctors. After having some substantial issues develop at 26 I has all of my concerns brushed under the rug by two doctors and finally found one who believed that there was something wrong. I was placed on metformin to try to help and suffered a pretty severe reaction and have now been researching natural ways to combat it. Other than here everything I’ve read says I can’t have gluten or even natural sugars. This gives me hope that I may be able to eat some things still as I have the pallet of a two-year-old and am a picky eater.
Hello, Love this!
I was recently told by my doctor that I have uterine fibroids. ( are these fibroids linked to PCOS?) I went in thinking I had hypothyroidism but my lab tests all clean… now checking for PCOS. I have cleaned my diet no gluten vegan. Any suggestions would be greatly appreciated. I love your articles. And again many thanks!
Hi Jess,
The fibroids are probably linked to an estrogen/progesterone imbalance, but may not necessarily be from PCOS. You should have all of your sex hormones evaluated to see what the main problem is.
Hi doctor,
I’m 29 years old, and was diagnosed with PCOS over 5 years ago. I have hormonal imbalance, and doctors prescribed me hormonal medicines like Diane35, and Yasmin supplemented with other drugs. Now my hormonal imbalance was improved, I have no more hormonal imbalance, but I still do not have menstrual cycles.
Now I stopped any medicine healing, and trying to heal with healthy food and exercises.
Is it possible after many years of medication?
Hi Amalya,
Yes, it’s always a possibility but I don’t know for sure if it is possible for each and every person.
Hey!
I was diagnosed with PCOS awhile ago but I basically had it for more than half my life.
I have struggled with food and many of the symptoms. I crave carbs and sugar so much. I have stopped in the past but that isn’t working anymore and I am having trouble controlling my diet. Is there something I can eat more to stop craving sugar so much?
Hi Jen,
I would take a look at this list of appetite suppressants for more info! https://www.restartmed.com/appetite-suppressants/
Hi!
I was diagnosed with PCOS when I was about twelve but have honestly kind of forgotten about it until recently. I’m 19 now, and was diagnosed with type one diabetes when I was 17. After being hospitalized twice for excruciatingly painful periods in the past five months and noticing a striking increase in certain symptoms (weight gain, acne, mood swings, unwanted hair, etc), I have since remembered my PCOS diagnosis from what seems like a million years ago. Do you have any thoughts about 1) if the type one diagnosis could at all be related to my PCOS (especially because my A1C is consistently 5.9-6.1 despite my being pretty irresponsible about handling my diabetes/insulin/pump) and 2) how I can effectively change my diet/supplement while still making sure my insulin levels won’t cause my blood sugar drop too low?
I was diagnosed with PCOS recently and have all the symptoms like hair loss, unwanted hair, weight gain except that there were no cysts on ovaries. I was prescribed with Metformin but I didn’t take because of side effects.
I am a vegetarian since birth but I crave carbs and sugar too much. I am trying to fix my diet but it’s getting difficult.I did try keto but not sustainable for a long time. What supplements should I take for my issues? Is Myo inositol good for PCOS?
Blood work details:
DHEA SULFATE: 469 – High
SEX HORM BIND GLOBULIN : 21.4 – Low
Insulin: 29 – High
Hb1ac: 5.6
TSH: 4.26