There are at least 6 different types of PCOS that are recognized.
Each type of PCOS has a unique cause and though there is some overlap between conditions, they are NOT all the same.
Knowing the type of PCOS that you have is critical if you want to get serious about treatment.
The various types of PCOS include insulin-resistant PCOS, adrenal PCOS, non-insulin resistance PCOS, mixed PCOS, post-birth control PCOS, and secondary PCOS.
You are going to learn the differences between each of these and how it impacts treatment.
Let’s dive in:
Diagnosing PCOS is Easy (Typing PCOS is more difficult)
I think it’s more helpful to think of PCOS as a hormone imbalance or a hormone problem.
Once you start to think of PCOS in these terms you can better understand how you want to focus treatment.
If your hormones are out of balance then bringing them back into balance may dramatically improve your symptoms or even reverse them.
But, before we talk about the types of PCOS, we do need to go over the basics including how PCOS is diagnosed.
Diagnosing PCOS:
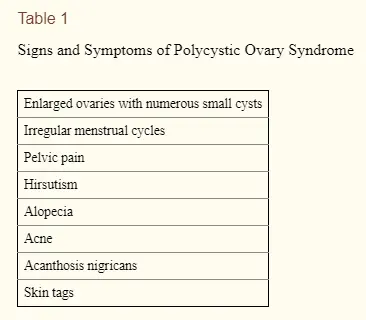
- Symptoms of EXCESS androgens – Symptoms may include hirsutism (abnormal hair growth), acne, male pattern baldness, and a deepening voice.
- Infrequent or absent menstrual cycle – Often referred to as oligomenorrhea which is the medical definition of longer than normal periods. You may also have no periods (amenorrhea), infertility, or ovulatory dysfunction (meaning you do not ovulate normally).
- +/- Polycystic ovaries (NOT required for diagnosis) – Contrary to popular belief, polycystic ovaries are NOT required for the diagnosis of PCOS. In fact, they aren’t even seen in many women who have PCOS.
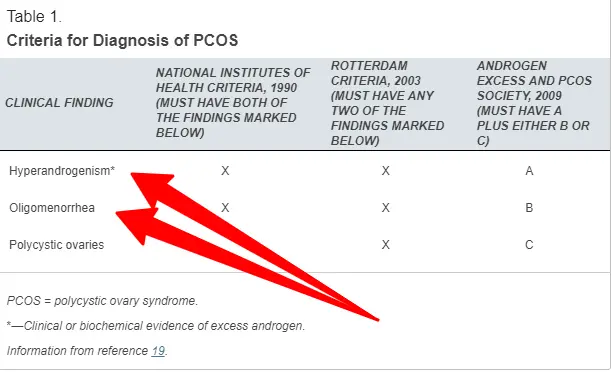
You should notice right away that the diagnostic criteria have nothing to do with your hormone levels.
PCOS is predominately a clinical diagnosis (1) (meaning it is diagnosed based on your clinical presentation) and it is confirmed with lab studies.
What does the diagnosis of PCOS tell you?
It only tells you that you have the SYMPTOMS and CONDITIONS listed above.
It does NOT tell you why you have it, how you should treat it, or what other problems you may be suffering from.
In fact, just knowing you have PCOS is really not that helpful at all.
It isn’t until you understand the type of your PCOS that you can discern the cause.
Once you have discerned the cause and type you can then start to focus your treatment.
What may surprise you is that the treatments for the various types of PCOS can vary dramatically.
And some therapies for certain types of PCOS can actually make other types of PCOS worse.
This is the main reason why you should not go for a one-size-fits-all approach to PCOS management!
Even though you don’t technically need additional tests to diagnose PCOS, I still recommend that you look at a variety of hormones and other markers to help you understand what is going on in your body.
We are going to be referring to some of these markers, so I want to at least touch on them.
Markers that you should be aware of if you have or suspect you might have PCOS:
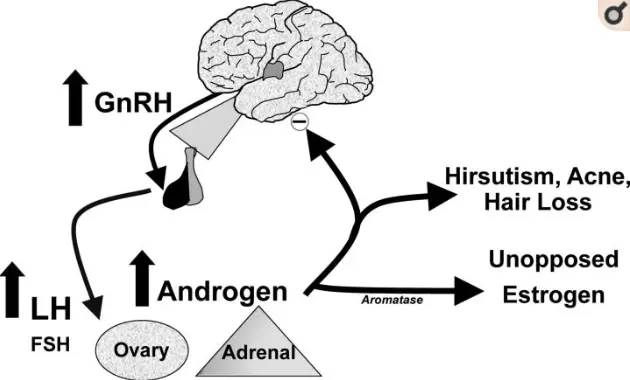
- LH (luteinizing hormone) and FSH (follicle-stimulating hormone) – These are hormones produced by your pituitary gland (in your brain) and are part of the hypothalamic-pituitary-ovarian axis (2). You may need to test for these to see how your brain fits into your condition.
- Estradiol – Estradiol is the most powerful estrogen in your body though it is not the only estrogen. Women with PCOS tend to have higher levels of estradiol compared to progesterone.
- Progesterone – Progesterone is primarily produced by your ovaries and is necessary for ovulation! Women with PCOS often suffer from low progesterone and do not ovulate normally. Progesterone protects against the release of cortisol.
- Cortisol – Cortisol is produced in response to stress from your adrenal glands. Excess cortisol can lead to insulin resistance, aging of the skin, and increased fat accumulation (weight gain).
- DHEA – DHEA is a protective hormone produced by your adrenal glands which also has androgenic activity. High levels of DHEA can lead to problems in women with PCOS.
- Insulin – Insulin, produced by your pancreas, helps manage blood sugar. High levels of insulin, known as insulin resistance, is a problem for some women with PCOS.
- Fasting glucose – Glucose is another name for blood sugar. You can test for your blood sugar through the blood. High levels of blood sugar, especially in the fasted state, may be an early indicator of insulin resistance.
- Hgb A1c – Hgb A1c is a measure of how much sugar is stuck to your red blood cells. The higher your Hgb A1c the higher your blood sugar is. The Hgb A1c is a good marker of your average blood sugar over the lifetime of your red blood cells.
- Free and total testosterone – Free and total testosterone can tell you how much testosterone is either produced or available for use by your body. Women with certain types of PCOS often have high testosterone levels.
You don’t need to have these things memorized but you should have a basic working understanding of what they are and how they work.
Doing so will help you understand the various types of PCOS and how to actually treat them!
Below you will find 6 types of PCOS.
Each can be diagnosed by using some of the lab tests mentioned above and some other factors such as your personal history.
You should go through each of these and find which category you fit into best.
Once you find that category you can then personalize your treatment.
6 Types of PCOS
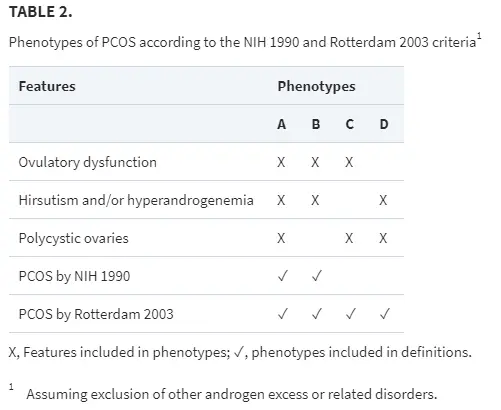
Before we jump in you should know that these types of PCOS are not all 100% recognized in the scientific literature.
Researchers and doctors all agree that there are many drivers which result in the symptoms that PCOS patients experience.
But what is not known is why certain patients with PCOS present differently than others.
The types below attempt to stratify patients based on symptoms and the differences found among PCOS patients.
But you should be aware that these causes or presentations represent more of a clinical picture and findings associated with PCOS.
These types are different from the phenotypes expressed in the Rotterdam criteria (3) which really only discuss various symptoms and presentations of PCOS.
It turns out, though, that the type of androgens that you have and how they stimulate your cells may help differentiate the various types of PCOS (4).
This information is also based on my own personal experience in treating patients who don’t fit the ‘standard mold’ but who clearly still have PCOS.
#1. Insulin Resistance PCOS
Perhaps the most well-known cause (and perhaps even the most common cause of PCOS) is insulin resistance.
The connection between PCOS and insulin resistance is so strong that some people have suggested that ALL women with PCOS be treated for insulin resistance (5).
Does this actually make sense? There is some logic to it, but following that idea will certainly not treat every case of PCOS.
We will talk more about that later and why it is so important to understand the cause of your PCOS in a bit.
For now, let’s focus on insulin resistance.
Insulin is another hormone in your body and it is secreted by your pancreas (another tissue/organ in your body) in response to the foods that you eat.
Sugar, but also protein, cause a dramatic rise in insulin levels in your body.
This rise of insulin is designed to help your body absorb the sugar/protein-rich meal that you just consumed to get it into your cells.
But what happens when you constantly put more and more sugars into your body?
The system goes haywire and you develop a condition known as insulin resistance.
Insulin resistance occurs when your cells become resistant to the normal effects of insulin.
In effect, they don’t recognize that insulin is there.
This causes insulin levels to rise and as insulin levels get higher and higher they start to cause other issues and problems.
Among these problems include an imbalance in your sex hormone (including estrogen, progesterone, and testosterone) and the signs and symptoms of PCOS.
High levels of insulin have been shown to result in high levels of testosterone (6) (both free and total) which is the hallmark of PCOS.
But that’s not all.
Insulin can also directly interact with cells in your skin including hair follicles and melanocytes.
This stimulation may result in hair growth in places you don’t normally want it (7) (including your upper lip and jaw), hair loss in places you do (male pattern baldness), discoloration of your skin (8) in places you don’t want (underarms, neck, and groin), and pimples or acne around the jawline.
Do any of these symptoms found familiar? They are all associated with excess ANDROGENS which are felt to be directly linked to high insulin levels.
When doctors talk about PCOS they most likely think of insulin resistance as the PRIMARY cause of your condition.
Because of this, most of the therapies are directed at reducing insulin levels and improving blood sugar.
This is why medications such as metformin are often prescribed to women with PCOS.
Metformin is a diabetic medication that helps reverse insulin resistance.
This is also why your doctor will want you to lose weight, change your diet, and exercise.
All of these conditions can and do help with insulin resistance.
It may sound counterintuitive but if you address insulin levels (at least in insulin resistance PCOS) you will also be treating the PCOS (9).
The good news is that diagnosing insulin resistance type PCOS is actually quite easy and you can do it with the following tests:
How to test for insulin resistance PCOS:
- Free and total testosterone
- Fasting blood glucose
- Hgb A1c (which stands for hemoglobin A1c)
- Fasting insulin
What type of lab test results do women have?
- Typically elevated free OR total testosterone (or high normal)
- Elevated fasting glucose
- Elevated Hgb A1c, typically higher than 5.7%
- Elevated fasting insulin
- Normal DHEA
The goal when treating this type of PCOS is somewhat counterintuitively to focus on the insulin resistance aspect.
We have many studies that state that focusing on this aspect is enough to normalize hormone imbalances in both androgens and sex hormones such as estrogen and progesterone.
The key here is to focus on those therapies which actually REVERSE insulin resistance and help improve blood sugar.
Therapies listed in this category include things like intermittent fasting, prolonged fasting, low carbohydrate diets, ketogenic diet, paleo-type diet, high-intensity interval training, insulin-sensitizing supplements, and insulin-sensitizing medications.
Cleaning up your diet is probably the first step to take if you have insulin-resistant type PCOS.
Doing this may be enough for you to see significant improvement.
If changing your diet doesn’t work alone, then you can start to layer additional therapies on top of dietary changes for an even greater effect.
This may include using many or all of the therapies I listed above.
But please realize that not ALL types of PCOS have an insulin-resistant component and some of the therapies listed above may actually make other forms of PCOS worse.
#2. Adrenal PCOS
Women with adrenal PCOS have the same symptoms as women with PCOS but their history and lab tests are slightly different.
The main difference is that these women typically do NOT have elevated free and total testosterone.
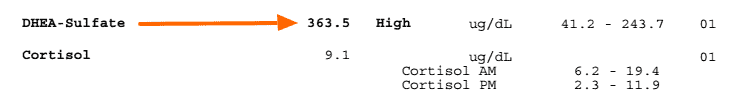
These women do, however, have elevated levels of DHEA which is another androgen predominately produced by the adrenals.
This is predominately felt to be stress-induced and, indeed, I tend to see certain patients who fit this category with very specific symptoms.
These are patients are typically type-A personalities, like everything to be in order, may suffer from anxiety, may be lean (though not always), and typically have higher-stress jobs or suffer from stress in their day-to-day social lives.
How to test for adrenal PCOS:
- Check free and total testosterone
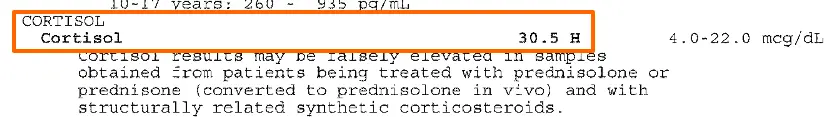
- Check 8 am serum cortisol (I don’t recommend salivary or urinary cortisol levels)
- Check serum DHEA
- Check measures of insulin resistance (fasting glucose, Hgb A1c, and fasting insulin)
What do women with adrenal PCOS typically present with?
- Normal free and total testosterone
- High or normal serum cortisol (may also be borderline high)
- Elevated serum DHEA levels
- Normal insulin resistance and blood sugar studies
Treating adrenal PCOS is much different than other types of PCOS due to the influence of your adrenals on your levels of both DHEA and cortisol.
When treating adrenal PCOS you want to avoid any excess stimulation to your adrenal glands which may ultimately cause the release of more DHEA and/or cortisol.
DHEA and cortisol are both released in response to stressors.
The more stress you are under the more cortisol and DHEA your body will produce.
Certain types of diets, especially calorie restriction and fasting, can INCREASE cortisol which may exacerbate this type of PCOS.
Low-carb diets, such as the ketogenic diet or Atkin’s diet, can also do the same thing.
The foods that you consume when you have adrenal PCOS are, therefore, much different than when you have insulin resistance PCOS.
Women with adrenal PCOS often do better on higher carbohydrate diets (of course, we are talking about the good type of carbs here).
If you don’t differentiate between these conditions then you may inadvertently cause more problems as you alter your diet for the wrong condition.
Along that same vein is the fact that excess exercise can also increase cortisol levels.
Excess exercise, especially high-intensity exercise, may be counterproductive for adrenal PCOS.
High-intensity interval training (HIIT) is great if you have insulin resistance type PCOS but not for women with elevated DHEA.
Instead, more low to moderate type of exercises can be beneficial because they are not as stimulating to your adrenals.
Of course, you should also practice therapies which help the body ADJUST and MANAGE the stress that you are under.
Therapies such as yoga, meditation, and mindfulness can all help you manage the stress that you are under day to day.
Furthermore, some supplements, especially adrenal adaptogens like ashwagandha, may also help regulate cortisol and DHEA.
Some studies even show that these supplements can bring balance to cortisol and DHEA.
Be cautious of using supplements that contain pregnenolone as pregnenolone is a precursor for DHEA.
If you provide your body with the substrate pregnenolone then it may metabolize it into more DHEA and thus exacerbate your condition.
#3. Non-insulin resistant PCOS (Lean PCOS/Inflammatory PCOS)
This type of PCOS is probably more difficult to diagnose and treat because it requires some work in figuring out what is triggering the condition.
Non-insulin-resistant PCOS sometimes referred to as lean PCOS (10), is a form of PCOS which can occur in women who are not necessarily overweight or who have obvious signs of insulin resistance.
Thus the name “lean” PCOS after the fact that women with this condition have a normal body weight compared to the prototypical PCOS patients.
If you feel that you might fit into this category it’s very important that you differentiate your condition from hypothalamic amenorrhea (11).
This condition blocks your body’s ability to have a menstrual cycle or period (thus the name amenorrhea).
The hypothalamic component comes from the brain because the hypothalamus is the tissue responsible for triggering the menstrual cycle by stimulating the pituitary.
Hypothalamic amenorrhea is a condition that results in DECREASED LH and FSH due to hypothalamic suppression (another portion of your brain).
It can look a lot like PCOS and you may even be incorrectly diagnosed with PCOS if you have this condition, but it is not the same thing as PCOS.
Hypothalamic amenorrhea typically occurs from calorie restriction, extreme dieting, extreme exercise, or extreme stress.
Long-distance athletes, runners, cyclists, gymnasts, etc. can all develop this condition (12).
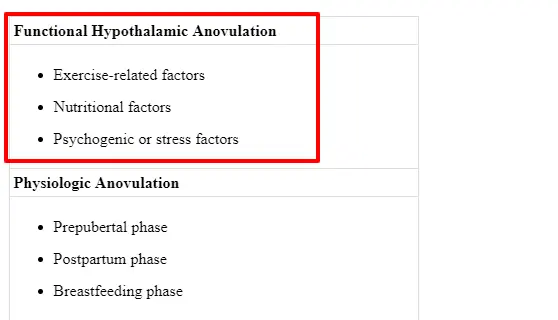
Hypothalamic amenorrhea can be differentiated from true PCOS by looking at LH levels which are much higher in true PCOS (13).
Once you have determined you do indeed have this form of PCOS, you now need to do some digging to figure out what is triggering your hormone imbalance.
It’s not as easy as other forms of PCOS such as adrenal PCOS and insulin-resistant PCOS because in those conditions we know exactly what is causing the imbalance.
Women with lean PCOS have obvious signs and symptoms of PCOS but their lab tests are largely “normal”.
This can obviously cause some confusion, especially for patients, as doctors try to find the cause.
While they don’t show signs of elevated DHEA or insulin resistance, some of these women do have elevated inflammatory markers.
And we know that inflammation is a key component in the development of PCOS (14) in all women who have it.
If your workup has been negative (meaning you don’t show signs of insulin resistance) then you need to be sure to check for the following markers:
- CRP (C-reactive protein)
- ESR (erythrocyte sedimentation rate)
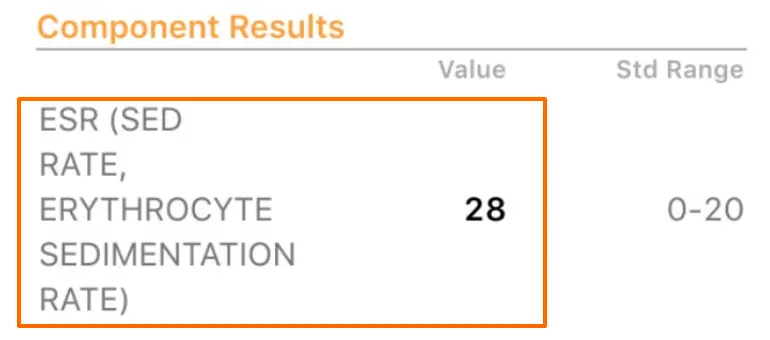
Both of these labs are indicators of inflammation in the body and may be the underlying cause or trigger of PCOS in your body.
For this reason, I sometimes refer to this subset of PCOS as inflammatory PCOS because it may be that inflammation is the primary driver.
Another interesting point worth mentioning is that even though women who have this type of PCOS do not show signs of insulin resistance via lab markers, they do seem to respond to therapies targeted at insulin resistance.
So even if your lab tests for insulin resistance are largely negative it may still be worth a trial to see if you respond.
You should do this in addition to addressing inflammation.
Some important triggers of inflammation may include the foods that you are eating, exposure to endocrine disruptors, lifestyle factors (lack of exercise or poor sleep), and so on.
You can also try certain supplements to help reduce inflammation and promote hormone balance:
- Magnesium
- Berberine
- Curcumin
- Fish oil
- Probiotics
#4. Post Birth Control PCOS (Temporary PCOS)
This type of PCOS is not really recognized by conventional providers such as ob/GYN or endocrinologists but coming off of birth control does appear to cause a temporary PCOS-like state in some women.
This doesn’t mean that you will get this condition if you go off of birth control but it does mean you should be aware of it if you are considering using birth control.
I’ve discussed the potential downsides of using birth control and the side effects associated with it here.
How do you know if you have this type of PCOS?
In order for your PCOS to be caused or related to birth control, you must have had normal periods BEFORE you started the pill.
If you had abnormal cycles before you started the pill then you could have easily had PCOS before birth control in which case your type of PCOS is probably not related to the pill at all.
But if you had normal periods before taking the pill and now you have abnormal periods OFF of the pill then that may be an indicator.
Again, women in this position should be careful to avoid a diagnosis of PCOS without first looking at LH and FSH levels.
The pill can cause suppression of your FSH and LH levels and lead to hypothalamic amenorrhea after you discontinue taking it (because it suppresses these hormones while you are on it).
Women who have a PCOS-like syndrome after stopping the pill have abnormally elevated LH levels which would differentiate this condition from hypothalamic amenorrhea.
In addition, they may also see a high normal level of prolactin.
The good news is that this form of PCOS is easier to treat and tends to be reversible given some time and targeted therapies at the HPO system (hypothalamic ovarian axis).
Your body will naturally improve its ability to produce LH, FSH, and prolactin over time but you can use certain herbs (15) to help accelerate this process.
Herbs that may help include:
#5. Mixed PCOS
What if you have findings of several of these types of PCOS but don’t fit into one box nicely?
If you fit into this category then you have a mixed presentation otherwise known as mixed PCOS.
As much as we would like to think that everything is simple, this is rarely the case in the real world.
While many of you reading this will probably mostly fit into one category over another, there’s also a possibility that you have characteristics from multiple types of PCOS.
Consider this example:
Imagine you have the signs and symptoms of PCOS with normal free and total testosterone but with an elevated PCOS.
In addition to your high DHEA, your lab tests also show some signs of insulin resistance.
In this picture, you are really displaying some signs of both adrenal PCOS (from the high DHEA) and insulin resistance PCOS (from the high blood sugar and high fasting insulin).
What do you do in this type of situation?
My recommendation is to try a comprehensive approach that includes the therapies designed to treat both conditions.
This will help you separate the real cause of your PCOS from what may be confounding variables.
For instance:
It’s absolutely possible for you to have insulin resistance which is not necessarily contributing to your symptoms of PCOS.
It could have been a secondary development from poor diet or other lifestyle choices or even genetics.
In this case, it may be that you are one of the ‘lucky’ 50% of people who will develop insulin resistance in your lifetime.
This condition would really be classified as adrenal PCOS with unrelated insulin resistance.
But there are also situations where you might find that both an elevated DHEA and insulin resistance may be contributing to your symptoms.
In this situation, you would truly have a mixed type of PCOS.
Mixed PCOS can be difficult to treat because it may be hard to pinpoint what your exact issue is.
But just because it’s difficult does not mean it’s impossible.
#6. Secondary Causes of PCOS & PCOS-like syndromes
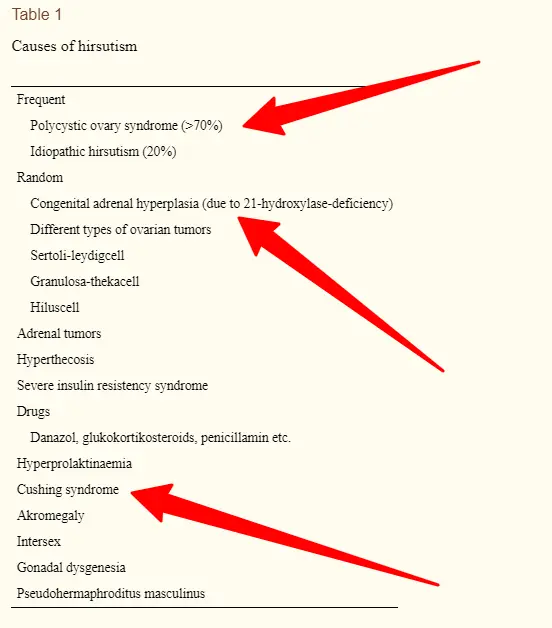
There are also several other conditions that can cause a PCOS-like state, some of which are reversible, and conditions that can mimic PCOS and must be ruled out if you suspect you have PCOS.
Conditions that fit into this category include:
- Hypothyroidism/Hashimoto’s (16) -> reversible cause of PCOS-like syndrome that can be treated with thyroid medication (or natural therapies)
- Adrenal hyperplasia (17) -> must be ruled out if you suspect you have PCOS
- Iodine deficiency -> reversible cause of hypothyroidism and PCOS-like syndrome, can be treated with iodine supplementation
- Elevated prolactin (18) -> must be ruled out if you suspect you have PCOS (check prolactin level)
- Cushing’s syndrome (19) -> must be ruled out if you suspect you have PCOS (check serum cortisol)
The thyroid is probably the most underdiagnosed condition that I see playing a role in “PCOS” in many women.
The hypothyroid state is enough to cause full-blown symptoms of PCOS and yet it is completely treatable for most women.
Thyroid medication and thyroid supplementation can help improve your thyroid function and may also improve your other sex hormones in the process.
There are a number of women out there who have thyroid disease who may not be aware of it.
Because of this, you should absolutely have your thyroid tested if you are showing signs of PCOS.
If you find, after a complete thyroid lab panel, that you have thyroid disease (or Hashimoto’s) then you should first target that condition.
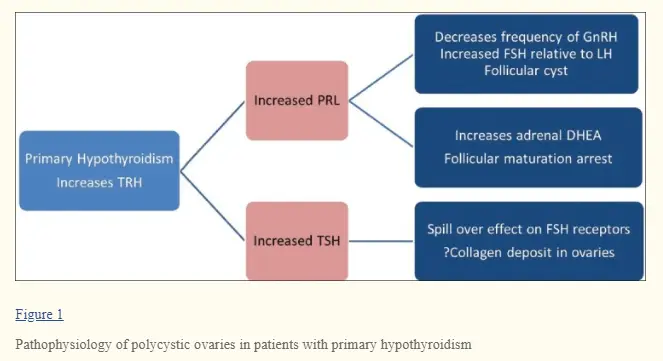
Doing so may clear up your PCOS symptoms.
Some women already know they have thyroid disease and may even be on thyroid medication but still have symptoms of PCOS.
I have found in my practice that many thyroid patients are undertreated or are currently using the wrong type of medication.
If you fit into this category be sure to explore thyroid medications that contain T3 medications (such as NDT, or Cytomel) which may have a more dramatic effect on your thyroid compared to levothyroxine and Synthroid.
Another common issue is iodine deficiency which can create a state of hypothyroidism that is completely reversible.
Iodine is also utilized by the ovaries and has an anti-estrogen effect (20) as well so a deficiency can affect both your thyroid gland directly and your sex hormones independently of one another.
Your doctor should know to check for these conditions but you should also be aware of them so you can be an advocate for yourself!
Conclusion
I’ve outlined what I believe to be 6 types of PCOS that I’ve seen in my own practice.
While not all of these types have clinical studies to support that they exist, it’s been my experience (and the experience of many other patients and providers) that they do.
What unites all of these conditions is that they share the symptoms of infrequent periods (or missing periods) and high androgen levels (or signs of high androgen levels in the body).
It makes logical sense, knowing what we know about various hormone systems, that there are many different ways for you to experience these symptoms and not all of them are the same.
If you are struggling from PCOS the best advice I can give you is to try and “type” your PCOS which can then help you extend your therapies beyond the traditional therapies of metformin.
Utilizing this approach should help you yield better results and help treat the underlying cause of your condition and symptoms.
Now I want to hear from you:
Do you suffer from PCOS?
What type do you fit into?
Have you not had success with traditional therapies?
Have some of the more traditional therapies worked for you?
Let me know which ones have worked and what other therapies you have tried in the comments below!