SIBO, short for small intestinal bacterial overgrowth, may be one of the most common gastrointestinal issues you’ve never heard about.
SIBO refers to an overgrowth of bacteria (often accompanied by fungal overgrowth as well) that causes a multitude of both intestinal and extraintestinal symptoms.
Symptoms range from depression to weight gain and fatigue – they all may be associated with changes to the microflora of your intestinal tract.
But is it common? Take a look at these studies…
SIBO has been detected in as many as 50% of patients taking acid-blocking drugs (1).
It is estimated that up to 50% of hypothyroid patients deal with SIBO in some form (2).
Somewhere between 4% and 78% (depending on the study) (3) of patients with IBS actually have SIBO.
Bottom line?
We aren’t talking about a small number of people here, we are talking about a huge portion of the population.
If you are struggling with any GI-related symptoms then read this list of SIBO symptoms to help you determine if you need further testing.
The Complete List of SIBO Symptoms
The hallmark of SIBO is the overgrowth of bacteria that occurs in the small intestines.
Let’s reflect on basic gastrointestinal anatomy:
Your small intestines consist of the duodenum, the ileum, and the jejunum. These sections of the small intestines are primarily responsible for the breakdown and absorption of nutrients, foods, and supplements/hormones that you are taking by mouth.
This should be compared to the large intestine which consists of the cecum, ascending colon, transverse colon, descending colon, sigmoid and rectum.
The primary function of the large intestines is to absorb water and nutrients (Biotin, Vitamin K, etc.) which are created by colonic bacteria from the fermentation of food.
Under normal circumstances, your large intestines should have significantly more bacteria than your small intestines.
So what’s the big deal with SIBO?
As the name implies, this condition results in excessive bacteria (both good and bad forms) in the small intestines.
This change in bacterial concentration causes several issues and symptoms as the bacterial concentration interfere with immune function, fermentation of food, absorption of nutrients, and inflammation locally (4).
All of the changes listed above result in various symptoms that can be assessed clinically (and you can test for it as well, but more on that later).
So let’s dive into what kind of symptoms you may present with if you have small intestinal bacterial overgrowth in your body.
#1. Severe Gas and Bloating – Especially after meals
The first and probably the most prominent symptom is extreme gas and bloating.
This gas and bloating is often associated with abdominal distention (your belly protruding) and seems to occur around 30-60 minutes after you consume a meal.
Why?
Well, it takes about 30-60 minutes for your food to enter from your stomach into the small intestines.
Once that food hits the overgrowth of bacteria in the small intestines, these bacteria cause excessive fermentation and breakdown of the food which results in the production of various gases.
Gases such as methane and hydrogen in high amounts can cause significant problems with the movement and kinetics of your bowels.
For instance:
Methane gas has been shown to reduce the kinetics of your small intestines and bowels which may cause severe constipation.
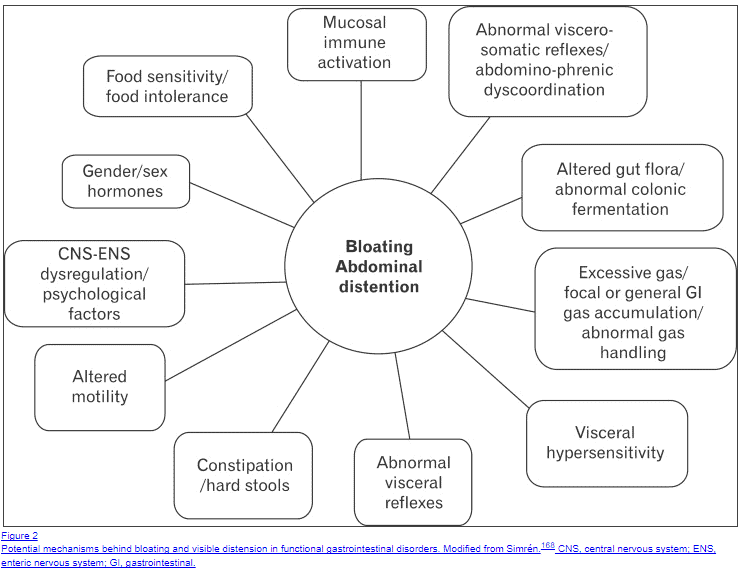
The gas production is only part of the reason why patients with SIBO present with gas/bloating and distention, however.
In fact, some studies have shown that there are no fewer than 11 reasons why patients with SIBO may have gas and bloating:
- Excessive gas production or general GI gas accumulation
- Visceral Hypersensitivity
- Abnormal Visceral reflexes
- Constipation/hard stools
- Altered motility
- CNS-ENS dysregulation and psychological factors
- Gender and/or sex hormones
- Food sensitivities and food intolerance
- Mucosal immune activation
- Abnormal visceral-somatic reflexes
- Altered gut flora or abnormal colonic fermentation
The point here is that there might be MANY reasons for your gas and bloating, but the common denominator is that they are all caused by the changes that occur secondary to small intestinal bacterial overgrowth.
Luckily, these symptoms tend to subside with proper eradication of bacteria (and usually fungal overgrowth which often accompanies SIBO).
#2. Constipation or Diarrhea
It is never normal to have constipation or diarrhea, especially if these occur on a frequent basis (weekly or even monthly).
Changes in your stool often reflect changes to your hormone levels (thyroid hormone), stress levels, autonomic nervous system activity, and colonic/intestinal bacterial concentrations.
The point is this:
If you are dealing with chronic constipation or diarrhea you need further assessment to figure out what is causing it.
That’s where SIBO enters the game.
SIBO most commonly presents with chronic, extreme, and persistent constipation (usually Bristol Type I stools).
We know that the consistency of stool is influenced heavily by the transit time (or time your stool spends in the GI tract) of your intestinal tract.
This refers to the automatic and rhythmic peristalsis that occurs in your GI tract at all times.
If your GI tract is moving slower than normal then you will have constipation.
If your GI tract is moving quickly then you will have diarrhea. It’s fairly simple.
The problem with SIBO is that the intestinal bacteria excessively produce methane gas, and methanogenic bacteria have been linked to chronic constipation in both IBS and SIBO patients.
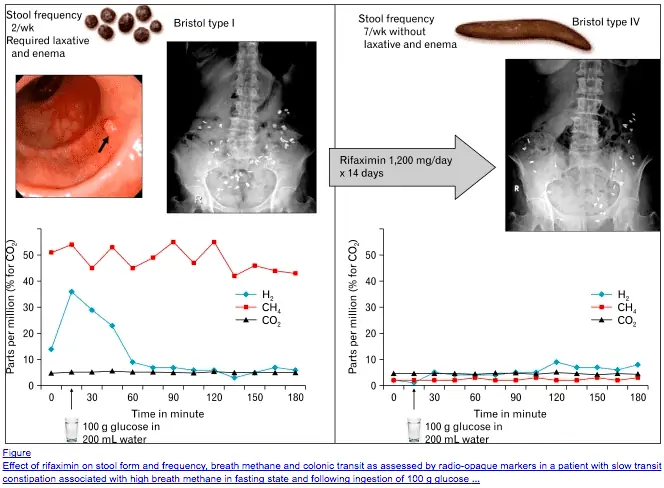
Methane gas seems to have a paralytic effect on your intestinal tract which acts to seriously slow down transit time.
The good news is that treating bacterial overgrowth may result in significant improvement and normalization of stooling patterns over time.
Case studies (and indeed this is true of my practice) suggest that eliminating bacterial overgrowth will increase stool transit time and significantly reduce constipation (5).
It’s also worth mentioning that not all forms of SIBO are created equal in how they interfere with GI function.
Some hydrogen predominant forms of SIBO may actually cause significant diarrhea, instead of constipation.
The point is still the same:
Treating the overgrowth will improve stooling patterns.
However, your treatment should consist of much more than just antibiotics to reduce bacterial concentration.
You can also use certain supplements to reduce constipation and improve the elimination of bacterial load from your colon and intestines:
- Magnesium Citrate – Magnesium citrate will help reduce constipation while simultaneously replacing any magnesium deficiency in your body. To treat constipation you may need anywhere from 200mg to 2,000mg per day.
- Vitamin C (Sodium Ascorbate) – Higher doses of Vitamin C can be combined with magnesium citrate to empty your bowels in a hurry. Use anywhere from 2,000mg to 5,000mg per day.
- Prokinetics like Iberogast – Iberogast is a combination of 9 herbs that promote gastric emptying and improve intestinal transit time which can help treat constipation (but in a different way than magnesium and vitamin C).
For best results, you will want to combine at least 2 of the 3 supplements together.
#3. Autoimmune Disease
Believe it or not, autoimmune disease may be a direct result of dysbiosis in the gut, and that includes dysbiosis from SIBO.
Studies have elaborated on the etiology of autoimmune disease and while it is complicated, there seems to be a significant connection between the development of autoimmune disease and intestinal dysfunction (6).
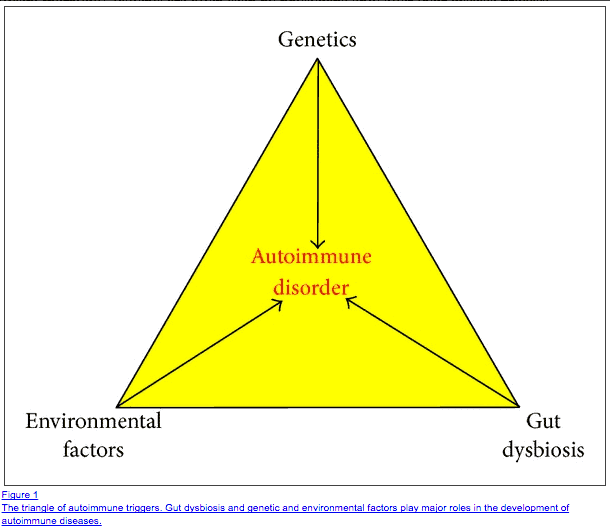
Autoimmune disease may result from GI dysfunction in several ways:
- Molecular Mimicry (7) – Absorption of various products including undigested food products and bacteria may look similar enough to target tissues in your body which your immune system may react to and trigger autoimmune disease.
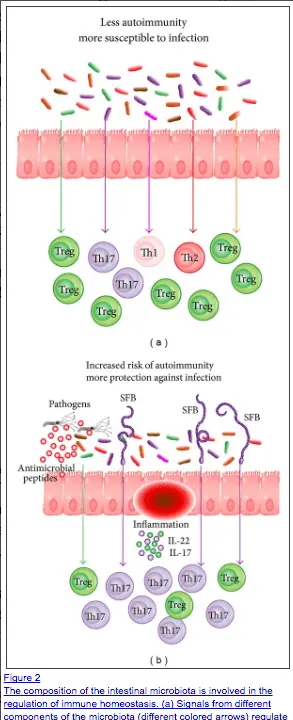
- Intestinal inflammation and increased intestinal permeability – Local inflammation in the GI tract (like that caused by SIBO) can weaken the intestinal lining and fidelity of the intestinal lining leading to increased intestinal permeability. This cascade of symptoms is known as “Leaky gut” (8) and may be the first step in developing and triggering autoimmune disease.
- Changes to immune function mediated through mucosal immunity (9) – The epithelial cells of the GI tract have a specialized function that act to promote, change and influence immune function in the body. Changes to the epithelial cells may reduce the function that mucosal immunity plays in the entire body, thus leading to an increase in autoimmunity.
Not every case of autoimmune disease starts in the gut, but if you have a history of autoimmune disease AND you have GI symptoms then it’s a very good idea to be evaluated for SIBO or other GI-related issues.
It’s also worth pointing out that most cases of autoimmune disease are caused by a combination of GI dysfunction (intestinal dysbiosis), and environmental factors which occur in the setting of certain and specific genetic patterns.
Usually, you need to have 2 or 3 of these factors all occurring simultaneously to trigger autoimmune disease.
The following list of autoimmune diseases that may be triggered through changes in GI function and dysbiosis:
- Hashimoto’s Thyroiditis
- Graves’ Disease
- Type I Diabetes
- Crohn’s Disease
- Multiple Sclerosis
- Rheumatoid Arthritis
So what do you do if you think SIBO is playing a role in your autoimmune disease?
Obviously, this is a complex topic but there are several simple steps you should take as soon as possible:
- Assess your Vitamin D level and treat if low – Vitamin D plays an important role in immune function and low levels have been linked with the development of autoimmune disease. Replacing Vitamin D levels may help but you need to make sure you use vitamin D3 (not D2). Aim to get your levels to the mid-range of the reference range (too much may increase your risk of cardiovascular disease). I have yet to find a person with “normal” Vitamin D levels in their serum, so this deficiency is VERY common.
- Take immune-boosting supplements like zinc – Zinc also plays an important role in immunity. In addition, and probably more importantly, many patients even in the US are zinc deficient. Taking zinc if you are deficient will improve immunity, but taking zinc if you have normal levels already will not.
- Consider using Beta glucans – Beta-glucans are naturally occurring sugars from pathogenic bacteria in your GI tract. The use of beta-glucans is meant to stimulate your immune system to help it “remember” the bad guys and differentiate them from the “good” guys. Studies have shown that taking beta-glucans stimulates the complement system (10) (part of your immune system) which may help improve overall immune function.
#4. Nausea
Many, but not all, patients with SIBO present with some degree of nausea.
The mechanism for this symptom seems to be related to the paralytic effect that SIBO has on your bowels, including your stomach.
When your stomach slows down emptying this is known as delayed gastric emptying.
Delayed gastric emptying leads to the filling of your stomach with stomach acid which may cause your stomach to expand and trigger the nausea reflex through the vagus nerve.
In addition to that delayed gastric emptying may lead to and exacerbate gastroesophageal reflux disease (GERD) or heartburn.
The main way to reduce the symptom of nausea is to increase gastric emptying with the use of prokinetics (see Iberogast above).
#5. Acid Reflux
The presence of gastric esophageal reflux is never a normal symptom, but more importantly, the treatment with acid-reducing drugs may actually CAUSE or WORSEN SIBO.
If you recall the study I cited above you will remember that approximately 50% of patients taking acid-blocking medications test positive for SIBO.
Why does this happen?
The creation of acid is actually required (and healthy) for the assimilation and breakdown of food products to properly absorb nutrients.
Acid produced in the stomach also enters the duodenum and helps set the pH at which certain bacteria thrive.
Lowering the production of stomach acid causes an increase in the pH of the upper intestines which changes the environment and may allow for certain species of bacteria to grow in abundance.
Patients taking acid-blocking drugs have been shown to have a higher risk of developing osteoporosis (11), developing a different kind of colonic dysbiosis known as Clostridium difficile colitis (12), and developing nutrient deficiencies (13) from the reduction in stomach acid production.
Moral of the story?
Not only can SIBO cause acid reflux, but taking drugs to reduce stomach acid can also trigger and promote the development of SIBO.
Acid-blocking drugs that may cause and/or exacerbate SIBO include:
- Prilosec (over-the-counter)
- Nexium
- Protonix
- Zegerid
- Aciphex
- Dexilant
If you are taking any medication that blocks stomach acid (proton pump inhibitors or H2 blockers) then stopping this medication and treating the root cause of your acid reflux should be your next step.
#6. Symptoms Consistent with IBS
I mentioned previously that anywhere from 4% to 78% of patients with diagnosed IBS also have existing small intestinal bacterial overgrowth.
Why the large disparity between percentages in the studies?
In many cases, it seems that the IBS is actually caused by SIBO (14) and has simply been misdiagnosed as IBS.
This is really important because there really isn’t a good treatment for IBS aside from treating the underlying cause of the irritable bowel.
SIBO provides an accurate diagnosis and a legitimate cause of many of the symptoms of IBS.
What’s more interesting is that many of the symptoms of IBS coincide exactly with SIBO, further solidifying the idea that many cases of IBS are actually SIBO in disguise.
See a list of SIBO symptoms and IBS symptoms side by side:
- Bloating
- Gas
- Constipation
- Diarrhea
- Alternating Constipation/Diarrhea
- Bowel movements that are uncontrollably urgent, difficult to pass, or incomplete
- Clear or white mucus in the stool
- Bowel movements that relieve pain or discomfort
- Change in stool frequency or consistency day to day
- Visual change in stool over time
- Gas
- Bloating
- Diarrhea
- Abdominal pain or cramping
- Constipation
- Existing diagnosis of IBS or IBD
- Coexisting food intolerance
- Existing chronic illnesses such as fibromyalgia or chronic fatigue syndrome
- B12 or iron deficiency
- Fat malabsorption
As you will notice the symptoms don’t match up perfectly, and that’s okay.
This just indicates that SOME cases (not all) of IBS may be related to or caused by SIBO.
The bottom line is that if you have the symptoms of IBS or a known diagnosis of IBS then you should certainly be evaluated for SIBO.
Why?
Because correctly diagnosing and treating your condition may actually relieve or eliminate the symptoms of IBS (17).
#7. Abdominal Pain and/or Abdominal Cramps
Abdominal pain in SIBO likely stems from the combination of cramping, gas, bloating, and constipation.
As your intestines fill with gas they begin to cramp which presents as abdominal pain.
And this pain can be quite severe.
The same mechanism occurs with chronic constipation.
As your bowels distend, cramping can become very severe, which may land the occasional patient in the emergency department (this happens probably more than you think).
Not all patients present with abdominal pain, but instead with general discomfort.
This discomfort may be felt after meals, while eating, or generally throughout the day.
Sometimes, when abdominal pain is severe, patients may be diagnosed with a condition known as “functional abdominal pain”.
Generally, this condition is meant to imply that the gastrointestinal system is technically “working” but patients still have pain of unknown origin.
If you suffer from abdominal pain or have a known diagnosis of functional abdominal pain then you should be tested for SIBO.
#8. Digestive Issues
Digestive issues in patients with SIBO usually result from the change in the environment in the GI tract related to the changes in bacterial concentration.
In addition, patients with SIBO may suffer from low stomach acid which further worsens digestive capacity and efficiency in the body.
Digestive issues may present in the following ways:
- Acid reflux
- Delayed gastric emptying
- Malabsorption of fat
- Malabsorption of nutrients
- Upper abdominal pain (epigastric pain)
Improving digestive capacity in SIBO may be accomplished by treating the bacterial overgrowth and by supplementing with pepsin/HCl or other digestive enzymes.
Digestive enzymes can assist pancreatic enzymes in the breakdown of food products and reduce the “digestive load” that your body must take care of with meals.
In addition, another approach to reducing this digestive load is to mechanically break down your food prior to ingestion.
You can do this by juicing or by blending your food prior to consumption.
This mechanical change alters cell walls and improves absorption time and eases the burden of your body to break down food.
This can be done for a period of time (30-60 days) during the treatment of SIBO.
I recommend using this digestive enzyme 15 minutes prior to each meal and again in between meals.
In addition, you may want to consider a juicer to mechanically help break down the cell walls of fruits/vegetables to ease absorption (1 juice per day).
#9. Malabsorption of Nutrients & Minerals
Nutrient deficiencies are CAUSED by SIBO, but they aren’t necessarily a “symptom”.
Instead, each deficiency that you have may cause various symptoms relating to the function of that nutrient/mineral.
Nutrient deficiencies, in general, are quite common among SIBO patients (18) (some more than others depending on the severity of the overgrowth).
If you have a known diagnosis of SIBO, or if you have known nutrient deficiencies of unknown cause, then you should be evaluated/treated for SIBO.
I’ve included the most common deficiencies that SIBO can cause below:
- Vitamin B12 deficiency -> B12 deficiency is common among the general population of the US with some estimates putting it as high as 40%. Taking sublingual or oral preparations of B12 may be insufficient to replace cellular B12 levels unless bacterial levels are normalized. Instead, taking B12 injections/shots may be superior to oral formulations of B12.
- Iron deficiency -> Most cases of iron deficiency in SIBO patients are NOT accompanied by anemia. Instead, you may simply have suboptimal iron and ferritin levels which can contribute to symptoms such as hair loss, exercise intolerance, and low energy. Check your serum ferritin (which should be > 50) and use liquid iron for the best absorption.
- Vitamin A (fat-soluble) -> Vitamin A is a fat-soluble vitamin that may become deficient in your body if you experience changes to bile function and/or pancreatic lipase function. Vitamin A deficiency may cause acne (common among SIBO patients) and other skin issues. Replacement with liquid Vitamin A should rapidly improve symptoms. Use up to 5 drops per day of liquid Vitamin A for 30-60 days.
- Vitamin D (fat-soluble) -> We’ve already discussed the benefits of replacing Vitamin D previously so I won’t go over it here again, please see the dosing recommendations above.
- Mineral deficiencies -> The most common minerals in the body include magnesium, phosphorus, potassium, sodium, and calcium. In SIBO magnesium deficiency is bar far the most common mineral deficiency that I see among patients. You can check serum magnesium levels and RBC magnesium to assess the magnesium status in your body. When in doubt replacement with magnesium is generally very safe and effective. Put preference on magnesium citrate (if you have constipation) or magnesium glycinate for superior absorption. 200-400mg per day is generally sufficient to see improvement.
#10. Gut Inflammation and Systemic Inflammation
Gut inflammation is a consequence of local changes to bacterial concentration (the hallmark of SIBO).
Gut inflammation results in increased intestinal permeability, reduction in the integrity of the mucosal lining, changes to immune function, nutrient deficiencies, and malabsorption of fat.
We’ve discussed the consequences of such inflammation in previous sections of this post.
But what about systemic inflammation?
Systemic inflammation refers to inflammation that is present in your entire body and inflammation that can be measured using serum systemic markers such as CRP and ESR.
Systemic inflammation is generally a consequence of LPS (19) (lipopolysaccharide) that is absorbed into the systemic circulation.
LPS is an endotoxin and outer portion of certain bacteria which exists in your GI tract. When absorbed LPS has potent effects inside the body and can stimulate your immune system.
Normally LPS should not be absorbed, so absorption of LPS indicates a structural problem in the GI tract.
SIBO causes local intestinal inflammation which may weaken the integrity of the intestinal lining and allow for LPS absorption into the body.
The problem with systemic inflammation is that it may lead to various systemic issues such as fatigue, weight gain, and other hormone imbalances.
#11. Weight Gain (Sometimes Weight Loss)
Weight changes in SIBO come in two varieties:
- Weight gain (generally due to hormonal changes as a consequence of systemic inflammation)
- Weight loss (generally caused by damage to the intestinal lining which results in decreased absorption of food and nutrients)
If you experience weight gain as a consequence of SIBO will treating SIBO help normalize your weight?
In some cases, it may help with weight reduction, but in most cases treating SIBO will be insufficient to completely normalize your weight.
The main issue is that hormone imbalances created as a consequence of SIBO usually do not completely normalize after treatment, instead, they may require additional treatment and/or management.
Weight gain, on the other hand, usually does occur once the intestinal concentration of bacteria has been improved.
#12. Acne, Rosacea, Eczema, and Other Skin Issues
It is well-known and established that changes in the gastrointestinal tract are associated with skin changes – most notably acne.
This connection has been named the gut-brain-skin axis (20) and was proposed over 70 years ago when scientists found that many patients with mood disorders also exhibited co-existent skin conditions.
This connection is also frequently documented in patients with SIBO.
The exact mechanism behind why this is the case is not entirely clear but is felt to work something like this:
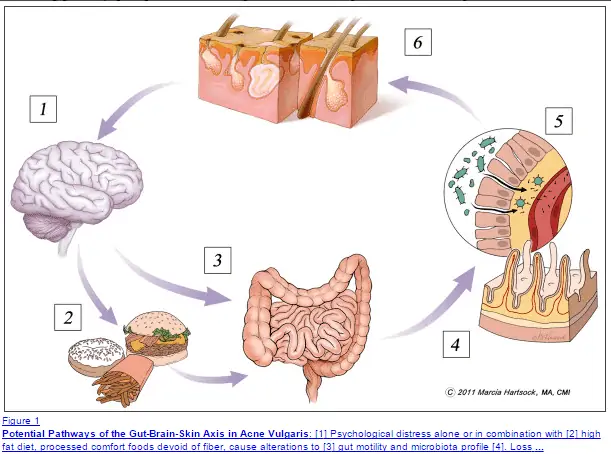
- Altered mood causes changes in appetite, neurotransmitter levels, and motility of the GI tract.
- Refined and processed foods cause direct damage to the intestinal lining. Meanwhile, changes in neurotransmitter levels change the kinetics of the bowel (predisposing to SIBO and fungal overgrowth).
- Damage to the intestinal lining occurs from these changes resulting in a burden of local and systemic inflammation, substance P from endotoxemia.
- Genetically susceptible patients then experience an increase in sebum production resulting in skin inflammation, acne, and/or rosacea.
- Changes to skin and aesthetics then trigger anxiety, depression, and other mood changes which start the cycle all over again.
So how do you break this cycle?
Studies have shown that taking antibiotics (herbal or prescription) when combined with probiotics can help improve intestinal integrity while reducing skin conditions and acne.
These changes may not be sufficient for everyone, however, especially considering that acne is often multifactorial.
You can learn more about treating hormonal acne in my complete guide here.
#13. Fatigue or Low Energy
The exact mechanism behind how and why SIBO results in fatigue or changes to energy levels is not well understood.
In my practice and treatment of SIBO I’ve narrowed it down to 3 main areas:
- Reduction in energy production and efficiency in mitochondria (likely LPS-induced damage (21))
- Nutrient deficiencies, specifically vitamin B12 deficiency (or simply suboptimal B12 levels)
- Hormone imbalances, specifically stress-related cortisol changes
The bottom line is that treating SIBO with antibiotics, prebiotics, and probiotics tends to partially improve energy levels but not back to normal levels.
The other half of the equation seems to be related to hormone imbalances and nutrient deficiencies that must also be addressed.
If you still experience fatigue after treatment or eradication of SIBO make sure to evaluate your serum cortisol and thyroid levels which can both contribute to energy production.
In addition, you might find the benefit of using supplements designed to improve mitochondrial function and efficiency (CoQ10 and Alpha lipoic acid work well).
#14. Mood Changes (Depression, Anxiety, Irritability)
Lastly, many patients with SIBO seem to present with neurological, mood, or behavioral symptoms.
Depression, anxiety, and panic attacks are particularly common among patients with SIBO and IBS.
We know that the connection between the brain and the gut not only exists but is bi-directional.
Put in simple terms:
Changes to your gut may cause changes to your brain and vice versa.
It has also been shown that microbes (bacteria) in the GI tract play an important role in the metabolism of both tryptophan and serotonin (22).
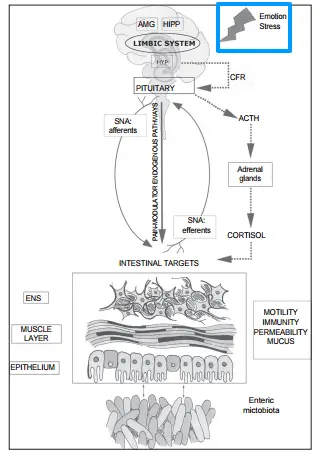
Changes to either or both of these neurotransmitters play a role in the development (or potentiation) of mood disorders seen in patients with SIBO and other GI issues.
This organic cause of behavioral changes needs to be differentiated from circumstantial depression that may be caused by the constant stress and reduction in the quality of life that SIBO patients tend to experience.
In the latter setting, symptomatic improvement may result in the complete resolution of mood changes.
In the former, treatment with supplements and/or medications may be necessary in addition to the eradication and normalization of intestinal bacteria.
Your Next Steps
Hopefully, this guide and symptom list serve as a solid starting point in helping you manage your GI symptoms.
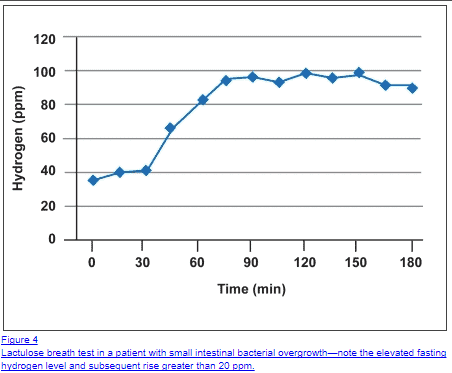
If you experience at least 3 of the symptoms listed above then your next step should be proper evaluation via a SIBO breath test.
This test isn’t perfect, but it will serve as a starting point to get you on the right track.
If you have a known diagnosis of hypothyroidism (meaning you are being treated with thyroid hormone) and you have 3+ symptoms listed above, then I generally recommend a trial of treatment prior to testing.
But the diagnosis is really just the beginning…
Treating SIBO may range from easy (about 30% of the time) to extremely difficult to eradicate (about 20-25% of the time).
Because of the difficulty and variability in the treatment of SIBO I have put together an 8-step comprehensive guide to get you started.
You can see the entire guide here.
I will also provide a general outline of what is necessary below:
- #1. Dietary changes
- #2. Probiotics
- #3. Antibiotics
- #4. Herbal antibiotics and supplements
- #5. Prokinetics
- #6. Fermented foods
- #7. Prebiotics
- #8. Intermittent Fasting
Now I want to hear from you:
Are you suffering from the symptoms of SIBO? Have you been able to get proper testing?
Have you been able to see improvement in your symptoms with treatment?
Leave your comments below!