It’s become more and more common for hypothyroid patients to experience symptoms despite having so-called “normal” labs.
But why is this?
There are actually a number of reasons why this is the case and each one is important.
In this article, I will go over 12 major reasons why you may be experiencing hypothyroid symptoms.
Each section will also include further information and help for you to utilize to solve/test for that issue.
The Meaning of Hypothyroid Symptoms
Experiencing persistent hypothyroid symptoms is a major problem.
Not only does it lead to quality of life issues such as fatigue, weight gain, and hair loss but it can also lead to more serious issues such as high cholesterol.
But what exactly does it mean if you have these symptoms?
It’s actually quite simple:
If you are experiencing true hypothyroid symptoms it means that your cells are NOT getting enough thyroid hormone.
This could be because you are taking the wrong type of medication, your dose isn’t high enough, your body can’t activate the hormone, the hormone isn’t getting into your body, and so on.
All of these problems manifest in the same way:
Low thyroid hormone and cellular stimulation.
With this in mind, we are going to talk about what you should be doing if you fit into this category.
And, by the way, you are in good company if you consider that there are literally millions of people in a similar situation as you.
And no, these symptoms are not caused by your mental state (depression).
Most of what I do for patients is simply figuring out which things are preventing them from feeling better.
This is actually not that complex (although it may seem this way at first) once you have an idea of what things you should be looking for.
Below you will find what I believe are the most common reasons that patients on thyroid medication (or not) experience persistent hypothyroid symptoms.
These are relevant to you whether you take thyroid medication, whether you have a thyroid or not, whether you have Hashimoto’s or not, and so on.
They matter to ALL thyroid patients (just some more than others depending on your situation).
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
#1. You are not on the right Thyroid Medication
This one is pretty simple and is probably the first place you should look.
Most patients are led to believe that there is really only one thyroid medication available and that is levothyroxine/Synthroid.
But, this is far from the truth.
There are actually at least 3 different classes of thyroid medications available and each class contains various brands.
These classes include:
- T4-only thyroid medications (which include medications such as levothyroxine, Synthroid, Tirosint, Tirosint-Sol, and Levoxyl)
- T4 + T3 thyroid combinations (which include compounded thyroid medications and NDT such as Armour thyroid, NP thyroid, Nature-throid, etc.)
- T3-only thyroid medications (which include sustained release T3, immediate release T3 formulations such as liothyronine and Cytomel)
Most doctors (probably close to 98% of them) will prescribe levothyroxine/Synthroid and never even attempt to use these other medications.
This can be a huge problem because simply switching medications may be sufficient for you to feel a noticeable improvement.
The reason for this positive response is due to the type of thyroid hormone that each medication contains and also other important elements such as the inactive fillers/binders found within pharmaceutical medications.
Sensitivities to these binders/fillers (such as lactose which Synthroid contains) can reduce the absorption and cause intestinal distress.
If you are feeling poorly, despite altering your dose, then swapping medications is a potential option available for you.
It’s not as easy as it sounds, due to conversion calculates between thyroid medications, so be prepared for that, but it will definitely be worth it if you can find a winning combination for you.
#2. You are not taking Enough Thyroid Medication
The next most obvious reason for persistent hypothyroid symptoms has to do with your dose (assuming you are taking thyroid medication).
Your dose refers to the actual amount of thyroid medication that you are taking.
You might be thinking that taking the right dose is easy given how many doctors approach dosing, but that couldn’t be farther from the truth.
Dosing thyroid medication is an incredibly complex situation that requires evaluation of more than just the TSH (thyroid stimulating hormone) lab test.
We will touch on some of the important points related to thyroid testing in other sections here, so I won’t go into it now, but you should understand that your dose plays an important role in how you feel.
If your dose is insufficient (meaning it’s too low) then you are simply not taking enough thyroid medication to have any lasting impact on your symptoms.
And, in my experience, I find that doctors do tend to underdose patients more than they overdose on them.
But why is that?
It’s actually quite simple.
The reason is multi-factorial but the main reason has to do with the potential risk of side effects and symptoms.

The closer you are to your “ideal” dose the closer you are to taking too much medication.
Imagine this scenario to help you grasp this concept:
Imagine your ideal dose is 75mcg of Synthroid.
Taking anything less than 75mcg may cause hypothyroid symptoms (fatigue, weight gain, etc.) while on the flip side taking anything more than 75mcg may cause symptoms of excess thyroid hormone (palpitations, hot flashes, heat intolerance, etc.).
Your doctor would rather give you a dose of Synthroid which is 10-15% lower than this amount because they want to stay as far away as possible from accidentally overdosing.
Why?
Because overdosing results in symptoms, medication adjustments, and, theoretically, more risk of litigation on the side of the physician.
This same concept is applied to people who take insulin (another hormone in the body).
Doctors would much rather give you less insulin than you need because they are afraid of giving you too much which may trigger hypoglycemic episodes and increase the risk that you (and they) could get into trouble.
There’s only one problem with this approach.
It means that as a patient you are probably going to feel poorly because you simply aren’t taking enough medication.
This approach would make sense if the risks of taking too much medication outweighed the benefits of taking enough thyroid medication but this isn’t really what is seen in clinical practice.
Instead of patients becoming overmedication with any dose over 75mcg, there is more of a range of acceptable medication which can be tolerated above the amount that you need.
Increasing beyond this amount (in our case 75mcg) will probably not cause immediate negative symptoms but instead, you may start to feel slightly and slowly unwell compared to previous dosages.
This means that you can effectively mitigate negative symptoms associated with overdosing while attempting to obtain that “optimal” dose for yourself.
Just remember:
Optimizing your dose is incredibly important and don’t let your doctor underdose you for fear of negative side effects.
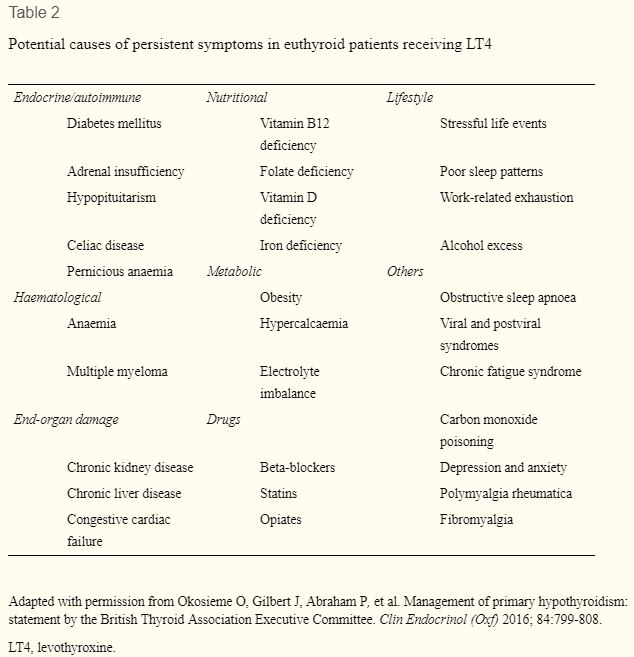
#3. Your ‘Thyroid Symptoms’ are not thyroid symptoms after all
It’s also possible, indeed probable, that your thyroid symptoms are not thyroid symptoms after all (or at least not 100% related to your thyroid).
What do I mean?
I’m talking about other medical conditions which can cause symptoms that are similar to those experienced by hypothyroid patients but the cause of which is entirely different.
And I find this to be incredibly common, especially among thyroid patients.
The reason this occurs is complex and has to do with the fact that your thyroid influences and regulates many other hormones and systems in your body.
But, if you have persistent thyroid symptoms, you want to make sure that you avoid something which I commonly refer to as thyroid tunnel vision.
Thyroid tunnel vision is an obsessive focus on your thyroid to the exclusion of all other conditions or problems.
People who suffer from thyroid tunnel vision believe that all of their problems are 100% related to their thyroid and the only way to fix those problems is to address their thyroid.
You want to make sure that you avoid this condition as it may lead to a situation where you never actually feel 100%.
Why?
Because there are actually some very important medical conditions that can cause symptoms that are nearly identical to those found in hypothyroid patients.
I’ve included a list below of these conditions:
- Obstructive sleep apnea (1)
- Chronic fatigue syndrome (2)
- Fibromyalgia (3)
- Viral syndromes (4)
- Obesity (5) (more on this below)
- Anemia
- Adrenal insufficiency (6)
- Side effects from medications
- Exposure to stressful life events (more on this below)
- Burn out syndrome
- Other autoimmune diseases
If you are someone who has thyroid disease AND you suspect that you have one or more of these other conditions then these conditions should be addressed (or at least diagnosed) first.
Failing to do so will mean that you may perpetually feel poorly and continue to suffer from “hypothyroid symptoms”.
There is certainly some cross-talk between these conditions and your thyroid may suffer directly from these conditions, but they can also mask other thyroid-related symptoms as well.
Consider it ‘good medicine’ to have yourself checked for and evaluated for these conditions if you have thyroid disease.
This is something both you and your doctor should be aware of.
#4. You have autoimmune thyroiditis
Autoimmune thyroiditis is another common reason for hypothyroid symptoms in the setting of so-called “normal” thyroid lab tests.
And this is actually a well-known and well-documented problem (7).
Before we talk about that, though, let’s quickly recap what Hashimoto’s thyroiditis is.
Hashimoto’s is an autoimmune disease that primarily affects your thyroid gland in that your own immune system slowly destroys your thyroid gland.
Over time this will lead to the complete destruction of your gland and reliance upon thyroid medication for life.
Hashimoto’s (otherwise known as autoimmune thyroiditis) is important to this conversation because it is incredibly common.
In fact, it is estimated that up to 70-80% of all people with hypothyroidism in the United States have thyroid-related issues due to this disease.
And many patients who have it aren’t aware that they do.
This complication sets up a common scenario that I see frequently on this blog:
Imagine that you are someone who feels poorly and all of your symptoms match up with hypothyroidism.
You have fatigue, weight gain, muscle aches/pains, hair loss, and so on.
All of your clinical symptoms point to hypothyroidism so you go to your doctor to get checked.
Your doctor checks the standard TSH test which comes back normal and he/she proceeds to tell you that your thyroid is fine.
This is a fairly standard scene among thyroid patients so what is the problem here?
The problem is that your doctor didn’t check you for thyroid antibodies which are an indicator of Hashimoto’s thyroiditis and autoimmune thyroiditis.
And these antibody levels can be ELEVATED even in the face of normal thyroid lab tests which includes a normal TSH.
So even though you were right that you have a thyroid problem, it will go unnoticed unless the CORRECT tests were ordered.
It is also very possible (and, again, well-documented) that patients with Hashimoto’s thyroiditis experience hypothyroid symptoms with normal thyroid lab tests.
This phenomenon has led researchers (and even some more progressive doctors) to recommend treatment of Hashimoto’s even if all thyroid lab tests are “normal” but if the patient is experiencing symptoms of hypothyroidism.
The big takeaway here is that Hashimoto’s thyroiditis is a very common disease that affects a large portion of the population and it’s a disease that doctors are not conditioned to check for automatically.
You may need to ask specifically for thyroid antibody tests including anti-TPO (thyroid peroxidase antibodies) and anti-TgAb (thyroglobulin antibodies).
If you find that they are elevated then you can initiate treatment with a combination of natural and conventional treatments to help restore thyroid function.
#5. You are not absorbing your medication
It’s possible for you to take your thyroid medication faithfully each and every day, even if it’s at the right dose, and still experience thyroid symptoms.
One reason for this has to do with the absorption of thyroid medication in the intestinal tract.
You can take all of the thyroid medication in the world but if it isn’t being absorbed into your body then it won’t do any good for you.
And this problem is actually quite common, especially among thyroid patients who have a very high incidence of intestinal issues.
Hypothyroidism (the state of low thyroid function in the body) slows down intestinal function and alters the population/concentration of healthy bacteria in your gut.
These factors can all influence medication absorption of both thyroid hormone and other medications.
People who have issues with thyroid absorption remain symptomatic despite taking their thyroid medication each and every day.
Several factors can influence how well you do (or do not) absorb your medication and I’ve listed several below:
- The time of day that you take your medication – It’s typically recommended that you take your medication in the morning but newer studies have suggested that taking it at night may be better for some people.
- Whether or not you have existing intestinal dysfunction – Existing intestinal issues such as acid reflux, SIBO, and IBS may impact your ability to absorb your medication and should be addressed/treated.
- If you take your medication with food/drink/coffee – Pretty much all types of foods and drinks (including coffee (8)) have been shown to reduce the absorption of thyroid medication if they are taken at the same time.
- The type of thyroid medication you are taking – Some thyroid medications are more difficult to break down by your intestinal tract. Other medications, such as Tirosint, contain very few fillers/dyes and are easy for your gut to absorb.
- If you take your medication with other over-the-counter supplements – Over-the-counter supplements which contain iron and calcium are notorious for binding to and inactivating thyroid medication. Do NOT take your medication at the same time as these supplements.
- Other medications you may be taking – Other medications, if taken at the same time as your thyroid medication, can cause absorption issues. For a complete list of these medications please see this article.
#6. Your Labs aren’t optimized
You can really think of this as an extension of #2 which has to do with your dose of thyroid medication.
Your dose of thyroid medication directly influences your thyroid lab tests.
And when I am talking about thyroid lab tests I am referring to much more than just the TSH.
I am referring to the combination of TSH, free T3, free T4, and reverse T3 (total T3 can be included here but it doesn’t necessarily have to be).
Any thyroid medication that you take by mouth will have a direct influence on these lab tests either for the positive or for the negative.
For instance:
As you take thyroid medication (of any type) you should notice that your TSH decreases.
This decrease is more prominent with medications that contain T3 thyroid hormone but any and all thyroid medications will cause a decrease in the TSH.
But in addition to influencing your TSH, your thyroid medication will also have an influence on the other thyroid lab metrics I’ve listed above.
If you are taking the thyroid medication levothyroxine then this medication should be causing all of the following changes to your labs:
- A reduction in the TSH
- An elevation in free T4
- An elevation in free T3 (hopefully)
- No effect on reverse T3
- An elevation in total T3 (hopefully)
Taking this medication SHOULD impact your thyroid lab tests in the following way. But just because it can impact them does not tell you anything about the degree to which it impacts them.
And the degree to which levothyroxine (or any other thyroid medication) impacts your lab tests has to do with the dose that you are taking.
In addition, there is a big difference between having a “normal” TSH and free T4 and having an “optimal” TSH and free T4.
The difference between these two conditions can be staggering and can potentially result in the difference between feeling well and feeling unwell.
Your goal as a patient taking thyroid medication should be to evaluate ALL of these lab tests and ensure that they are optimized (as opposed to the wide “normal” range provided by standard lab tests).
This optimization is complex but it is nonetheless very important.
You can learn more about why optimizing your lab tests (and thus your dose) is so important in this post.
#7. You have un-treated nutrient deficiencies
We’ve mentioned that medical conditions can cause symptoms that mimic hypothyroid symptoms in a previous section and now I want to talk about nutrient deficiencies which can do the same thing.
But, for this discussion, it’s important that you understand the difference between gross nutrient deficiencies and sub-optimal nutrient deficiencies.
Gross nutrient deficiencies are those which are easily diagnosed through standard lab tests and ones in which patients obviously have symptoms correlating with a deficiency in a specific nutrient.
This would be something like experiencing scurvy by not getting enough vitamin C.
These types of nutrient deficiencies are fairly rare and are hard to miss.
And when I talk about nutrient deficiencies I am not talking about these types of deficiencies.
Instead, I am referring to a more sinister deficiency which I refer to as a sub-optimal deficiency.
A sub-optimal deficiency is a minor deficiency in the nutrients that your body needs which may go unnoticed in your symptoms/lab tests because it only causes minor symptoms.
I find this type of deficiency to be very common among people in the United States.
This occurs even in the setting of nutrient-fortified foods due to numerous conditions including stress on the body and nutrient-depleted soil (9) which crops are grown on.
Furthermore, testing for nutrient deficiencies, in general, is actually quite difficult and standard lab tests are notoriously inaccurate (10) and insufficient.
So you may go to your doctor to get a standard B12, folate, and magnesium test which shows your levels are “normal” when in reality you are sub-optimal.
This is important because many of these nutrients play an important role in thyroid function!
Among the most important include: Tyrosine, Iodine, Vitamin D, Magnesium, Vitamin A, B12, B6, Zinc, and Selenium.
There are plenty of others that are also important but I find that thyroid patients tend to be deficient in these specific areas.
Treating these nutrient deficiencies with the right type of supplements may help improve your thyroid function.
They can do this by affecting other hormone systems (such as cortisol), reducing inflammation, and providing your thyroid with nutrients that it may directly be in need of.
I strongly believe that supplementation should be a part of MOST people’s lives (with or without thyroid issues) because it’s so difficult to get all of the nutrients you need from your diet alone.
The only downside to supplementation is that some people seem to benefit from supplements more than others and it’s difficult to identify who will see lasting benefits.
Because of this, it may take some element of trial and error on your part to figure out what you need to be taking temporarily and long-term.
#8. Your medications are interfering with your thyroid function
We’ve discussed how medications can impact how much thyroid medication you are able to absorb and this is important but there is another way that medications can impact thyroid function.
Some medications interfere with your thyroid by directly inhibiting or altering thyroid hormone metabolism.
Various prescription medications can do this by either inhibiting the release of thyroid hormone directly, reducing peripheral T4 to T3 conversion, or directly damaging your thyroid gland.
This can be confusing for patients, and rightfully so, but you should never forget that all medications carry with them potential side effects (both good and bad).
The following medications have been associated with thyroid inhibition at one or more levels:
- Diabetic medications (11)
- Blood pressure medications (12)
- Anti-seizure medications (13)
- Depression medications (14)
- And others…
You can find a more complete list of medications on this list here.
As a side note, just because you are taking one or more of these medications doesn’t necessarily guarantee that it IS interfering with your thyroid function.
These medications have the POTENTIAL to do this but there will always be some people who can take them without issue.
In addition, even if you are taking a medication and it is inhibiting your thyroid, doesn’t mean that you should necessarily stop your medication.
Some medications are necessary for life-preserving reasons (such as antiarrhythmics (15)) and thyroid damage may be a necessary (but unwanted) side effect.
It would be better to have some diminished thyroid function rather than dying from arrhythmia, for instance.
#9. You are overweight
Obesity (or just being overweight) is really a double-whammy for thyroid patients.
Not only does hypothyroidism lead to weight gain (this is undisputed) but obesity can also negatively impact thyroid function (16).
The worse your thyroid function is the more weight you will gain which will, in turn, worsen your thyroid function and so on.
The only way to stop this vicious cycle is to simultaneously address both your weight AND your thyroid at the same time.
Failing to do so may leave you with both the inability to lose weight and persistent hypothyroid symptoms.
To make matters worse, the traditional treatments for weight loss can also negatively impact your thyroid.
Therapies such as calorie restriction can lead to low T3, high reverse T3, and low total T3 levels.
Because this can be complicated, I’ve created a weight loss guide that details how to do this properly.
You can also check out these blog posts which offer plenty of information (including case studies of people who have lost weight with thyroid disease).
#10. You have sub-clinical hypothyroidism
This one is probably not as important as the others but it still pops up from time to time and so I think it’s worth mentioning.
The term sub-clinical hypothyroidism refers to a state of thyroid function which is somewhere between normal thyroid function and typical hypothyroidism.
But don’t let the term sub-clinical hypothyroidism fool you.
Sub-clinical is anything but sub-clinical.
Sub-clinical is meant to define a state which refers to abnormal thyroid lab tests but normal clinical symptoms.
But there’s one big problem with this idea.
Most people who have sub-clinical hypothyroidism are ALSO symptomatic.
And this is well-known, which has prompted more forward-thinking physicians to consider treatment in these patients.
Sub-clinical hypothyroidism is typically defined based on your TSH.
So the “standard” interpretation of TSH looks something like this:
- TSH from 5-10 mIU/L = Considered subclinical hypothyroidism
- TSH > 10.00 mIU/L = Considered true hypothyroidism
- TSH < 1.00 mIU/L = Considered hyperthyroidism
But newer guidelines suggest that optimal TSH function is probably less than 2.5 (17) and these studies recommend that this range should be tightened to account for this.
Newer guidelines would look something like this:
- Any TSH > 2.5 mIU/L = Potentially hypothyroidism
- Suppressed TSH mIU/L = potentially associated with hyperthyroidism (but not always)
- TSH around 1.0 mIU/L = Treatment goal which reflects euthyroidism for most healthy people
Unfortunately, you will find physicians who aren’t up to date and who use the old standard ranges that I referenced originally.
If you fall into these ranges then be sure to seek out appropriate care from a knowledgeable physician who is more willing to look at newer research.
#11. Your Genes are playing a role
Genes and the impact that they play on your overall health are becoming better understood each day.
And, it turns out that these genes are also very important for thyroid function and thyroid metabolism.
There are a number of critical enzymes in your body, known as deiodinases, which regulate the metabolism of thyroid hormone.
Small changes, or mutations, to the genes which encode these enzymes, may manifest in various ways.
For instance, and probably the most relevant to this conversation is the fact that some of these mutations can alter how you react or respond to certain thyroid medications.
There are many genes, and we are uncovering new mutations each year, but I’ve provided a list of just some of the most well-documented mutations and how they may impact your health below:
DIO2 (deiodinase type II):
- rs225014/rs12885300 (18) = associated with the development of osteoarthritis
- rs225010/rs225012 (19) = associated with mental retardation in iodine-deficient areas
- rs225014 (20) = associated with psychological well-being on T4-only medication
- rs225014 (21) = Preference for T3/T4 thyroid medication over T4 only medication
- rs225014 and rs225017 (22) = Increased risk of developing type II diabetes and worse blood sugar control with diabetes
- rs225014/rs12885300 (23) = associated with bipolar affective disorder
- rs225014 (24) = associated with hypertension/blood pressure
DIO1 (deiodinase type I):
- rs11206244/rs12095080 (25) = associated with changes to IGF-1 levels
You can test for some (or all) of these mutations with tests such as 23andme.
I would not recommend this as a standard for all people with hypothyroidism (at least not yet) as this information can be confusing and your doctor may not know what to do with the information that you give them.
Furthermore, just because you have the mutation in your genetics does not guarantee that it will manifest or impact how you respond to medications.
This concept is referred to as penetrance (26).
#12. You are Depressed/Anxious or Stressed
Depression, anxiety, and stress are all also other factors that can both cause symptoms which mimic hypothyroid states AND which also interfere with thyroid function directly.
Stress, in particular, seems to have a profound effect on thyroid function (27) in certain individuals.
Stress, of any type, prompts the release of a hormone known as cortisol.
This stress hormone is supposed to alter the physiology of your body to better allow for it to sustain or adapt to the stressful state you placed it under.
The cortisol system works very well but, like other systems, it has a limit.
Extremely stressful situations, or just repeated small stressors, can put a strain on this system and cause changes to how cortisol impacts your cells.
This can lead to conditions such as insulin resistance, weight gain, and even thyroid dysfunction.
Depression and anxiety, on the other hand, tend to mimic the hypothyroid state by causing symptoms such as fatigue, changes to your appetite, decreased motivation/activity, and potential weight gain.
In addition, there is clearly a link between your thoughts and your physiology which may also be playing a role.
More important than why or how these conditions interfere with thyroid function is the fact that they MUST be addressed if you have a thyroid condition.
I understand it can be difficult, especially as hypothyroidism will make you more prone to developing depression/anxiety, but it is nonetheless important.
I address depression/anxiety much like obesity in hypothyroid states.
Treat both simultaneously for the best results.
If possible, look for underlying conditions which may lead to depression/anxiety and address THOSE issues.
This is preferred over masking the symptoms with medications such as benzodiazepines and anti-depressants (which may actually negatively interfere with your thyroid).
Conclusion
My hope is that after reading this article you have a pretty good idea as to what is going on in your body and even if you aren’t sure, hopefully now you have some direction.
Navigating the waters of hypothyroidism can be confusing, I totally get it, but it doesn’t have to be impossible.
A slow and measured approach will lead you to a combination of therapies that result in you taking back your life.
Now I want to hear from you:
Are you someone feeling poorly while taking thyroid medication?
Are you someone who isn’t taking thyroid medication but still is experiencing hypothyroid symptoms?
Which of the items from this list do you think might be contributing to your symptoms?
Leave your questions or comments below to keep the conversation going!