Whenever I think about things that thyroid patients can do to potentially improve their health, supplementing with vitamin B12 immediately comes to mind.
Why?
Because there are not very many easy “wins” for thyroid patients.
Many of the therapies required to improve your overall thyroid status may require a prescription from your doctor.
And, as you probably already know, getting your doctor to prescribe certain types of thyroid medications can be difficult!
The good news is, though, that there are still several things that you can do to improve how you are feeling overall and addressing your Vitamin B12 status is one of those.
Unfortunately, this particular issue is filled with some pitfalls which can limit how good you feel if you aren’t taking the right type of B12, your dose is off, or if you have certain genetic issues.
Let’s dive into these issues so you can get a clear picture of how B12 deficiency impacts both your body and your thyroid.
Vitamin B12 Deficiency is Incredibly Common Among Thyroid Patients
If you are reading this and you are a patient with thyroid disease then there is about a 40% chance that you are suffering from Vitamin B12 deficiency (1).
That means that roughly 4 out of every 10 people with thyroid disease have this issue.
And when you consider that millions and millions of people have thyroid disease, this number is actually incredibly large.
But when was the last time that your doctor talked to you about Vitamin B12, tested you for B12 deficiency, or mentioned the symptoms of B12 deficiency?
If you are like most people, this might be one of the first times you are hearing about this issue.
But why is vitamin B12 deficiency so common among thyroid patients?
The reason is actually multifactorial, meaning that there are multiple conditions that contribute to it and they all stem from how low thyroid function impacts your body.
The first reason that hypothyroid patients suffer from B12 deficiency has to do with an autoimmune disease that attacks certain cells in your stomach which renders them damaged and non-functioning.
This leads to the inability to absorb B12 and thus deficiency.
Roughly 1/3 (one-third) of primary hypothyroid patients have evidence of these antibodies!
The connection between hypothyroidism and this autoimmune disease probably has to do with the fact that the majority of hypothyroid cases are caused by another autoimmune disease known as Hashimoto’s thyroiditis.
And we know that if you get one type of autoimmune disease you are much more likely to get another.
That’s one reason, but there are many others as well.
Other conditions such as intestinal overgrowth (known as SIBO), which is also incredibly common among hypothyroid patients (2), can reduce B12 absorption in the GI tract.
Furthermore, low thyroid function can slow down intestinal transit time which limits absorption capacity and leads to a deficiency in this way.
So now we have at least 3 different ways that thyroid patients can become B12 deficient ranging from the bacteria in their gut to the speed of their GI tract to direct damage from their stomach from their immune system.
Once you start adding these up, it’s easy to see why 40% of you probably have some form of B12 deficiency.
The question really becomes what can you do about it?
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Symptoms of B12 Deficiency Mimic Hypothyroid Symptoms
Aside from simply testing for B12 deficiency, you should also be aware of the symptoms associated with this condition.
One major hurdle that thyroid patients face when it comes to B12 deficiency is that it can be very difficult to differentiate between true hypothyroid symptoms, meaning those caused by low thyroid function, and symptoms related to low B12 levels in the serum and in the cells.
There is immense overlap between these conditions as you can see from the list of B12 deficiency symptoms listed below:
- Brain fog
- Fatigue or weakness
- Weight gain
- Heart palpitations
- Constipation
- Changes to your tongue
- Numbness and tingling
- Depression
Perhaps the best way to differentiate between these conditions is to adequately treat your thyroid function (based on the optimal thyroid lab levels listed here) so that you know your thyroid isn’t a factor in your symptoms.
From there you can then use B12 supplements or injections to replete your B12.
At this point, you should be able to differentiate between them based on which symptoms improve during your therapies.
I would generally recommend, however, that you do both things simultaneously because I don’t see the benefit in waiting if you are symptomatic.
Treating your Thyroid Doesn’t Always Fix your B12
Another important issue worth pointing out is that B12 deficiency and your thyroid are two completely separate conditions.
Sometimes, with certain diseases, if you can find the root cause you can not only fix your primary problem but you will also find that many of your other conditions suddenly and, seemingly miraculously, clear up as well.
Unfortunately, B12 deficiency and hypothyroidism are not quite like that.
Taking the right type and dose of thyroid medication, while it will certainly help you feel better and improve your overall symptoms, is probably not going to be enough to fix your B12 deficiency (even though you may be now absorbing more B12 after treatment).
Instead, you want to consider each of these conditions as separate which will require different treatment.
The good news is that the treatment for B12 deficiency is to take over-the-counter B12 supplements (or B12 shots which we will discuss below) and the problem is typically rapidly addressed.
But just remember:
Treating your thyroid is often not enough to fix your B12 levels.
Pitfalls in Testing for B12 Deficiency
How do you know if you have a B12 deficiency?
The first place you should look is at your
But there’s one major problem with this approach.
Your serum levels of B12 are notoriously inaccurate and are not necessarily a good measure of the general B12 status of your body.
Serum B12 levels can be misleading or just plain wrong.
And doctors know this! In fact, they’ve known this for quite a while.
It’s one of the reasons that other tests exist such as methylmalonic acid (MMA).
Methylmalonic acid is said to be more reliable as a test of B12 deficiency because it will build up in your body.

The only problem with the MMA test? It’s expensive.
In fact, it’s been said before that it’s better to treat as if you have B12 deficiency if you suspect it rather than testing for the expensive MMA.
This is basic physiology and information that most doctors should be aware of from medical school.
Despite this, I think it’s actually still valuable to run some basic tests if you suspect B12.
Among these tests include the serum level of Vitamin B12, a complete blood count (to check for anemia), thyroid lab tests (to check your thyroid), homocysteine (to check for B12 metabolism), and folate levels.
Even though you can’t necessarily trust your serum B12 to give you all of the information you need you can still derive value from the test.
For instance:
Imagine a scenario in which you are both B12-deficient and folate-deficient upon testing. But upon testing your serum B12 is decidedly ‘normal” or even in the midrange but your MCV is elevated suggesting that the average size of your red blood cells is abnormal.
In addition, you also find that your thyroid levels are abnormal.
Even though your lab tests aren’t a slam dunk for B12 deficiency, you can read between the lines and make the assumption that you are probably not getting enough B12.
If you suspect you have B12 deficiency then it’s probably a good idea to run a trial of B12 supplementation simply because taking B12 is safe as long as your kidneys are functioning.
But if you want to get more in-depth information, then running the tests I listed above is probably a good idea as well.
MTHFR Defects and Using the Right Type of B12
We can’t really have a conversation about B12 without at least mentioning MTHFR defects and mutations.
What is MTHFR?
It’s an acronym that stands for methylenetetrahydrofolate reductase (MTHFR for short) and it’s an important enzyme that helps your body turn folate into important products such as DNA, RNA, and other amino acids.
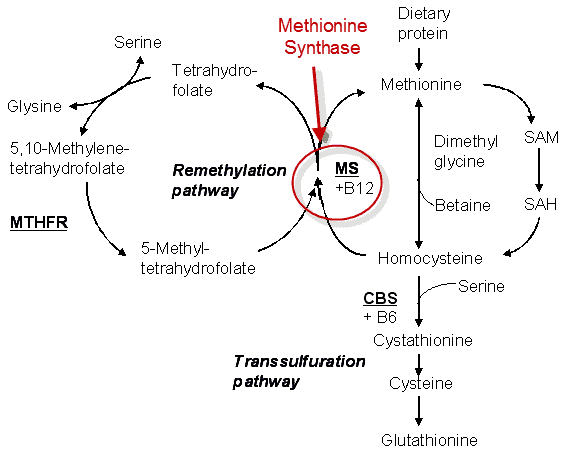
That’s what it’s supposed to do under normal healthy conditions. It turns out that there are a large number of people (anywhere from 20 to 40% (3)) who have small genetic mutations which impact how well this process works.
The presence of these mutations impacts how well your body metabolizes and utilizes folate and B12 and it also can impact your risk for certain diseases such as heart disease (4), high blood pressure, neurological issues, and birth defects.
We are not going to focus on the potential impact that the presence of these mutations has on your risk of disease but instead, we want to talk about how the presence of these mutations impacts what supplements you should or should not be using.
This is important even if you don’t know your MTHFR status or you’ve never heard of MTHFR before!
As I mentioned previously, approximately anywhere from 20 to 40% of people suffer from one or more of these mutations (5).
And where it’s most relevant to our discussion is how the presence of these mutations impacts how well your body can or can’t use certain formulations of B12.
Studies have shown that certain types of B12 including methylcobalamin, adenosylcobalamin, and hydroxycobalamin (6) are preferred over the more common and synthetic form of B12 known as cyanocobalamin.
The problem?
Cyanocobalamin is a cheap synthetic version of B12 which is often found in most B12 supplements!
The reason for this has to do with its cost. It’s far cheaper to mass-produce cyanocobalamin versus the other biologically active forms I listed above.
But this can lead to problems in your body if you suspect you have a B12 deficiency and attempt to solve that problem by using cyanocobalamin.
The reason for this has to do with the fact that these other forms of B12 are pre-methylated and, therefore, ready to be used by your body.
They don’t have to pass through the enzymatic phase that might be impaired if you have the MTHFR defect or mutation.
For this reason, it’s always preferable to use biologically active formulations of B12 even if you don’t know your MTHFR defect status.
Forms of B12 that are safe to use if you have hypothyroidism:
- Methylcobalamin
- Hydroxycobalamin
- Adenosylcobalamin
Formulations of B12 and folate that should be avoided:
- Folic acid
- Cyanocobalamin
My recommended hypothyroid B12 supplement contains only pre-methylated and activated formulations of B12 and folate.
You don’t necessarily have to use this version, however, but do be sure that you follow the guidelines listed above for the best results!
Can you take too Much B12?
Believe it or not, taking vitamin B12, even in high doses, is usually very safe.
The reason is simple:
Vitamin B12 is a water-soluble vitamin and your body eliminates any extra through your kidneys and through your urine.
So the risk of taking excessively high doses of B12 is mitigated as long as your kidneys are working (which is the case for many of you).
So, why even bring this up?
Because many doctors are not quite as familiar with B12 metabolism and its effects on your body.
In addition, almost every available over-the-counter supplement contains what would seem like very high doses of B12.
And these over-the-counter supplements, when taken orally, can cause your serum B12 level to spike up to a “high” level which may flag as abnormal.
This may cause your doctor to freak out and tell you that you are overdosing on Vitamin B12.
But is it actually a problem?
Most likely not.
Remember, we already went over the fact that you can’t necessarily trust your serum B12 as a marker of B12 status in your body (7).
Furthermore, there have not been any studies that show that B12 can become toxic or cause any problems (8) (as long as your kidneys are functioning (9)).
This doesn’t mean that taking B12 is always without side effects, however.
It’s possible that rapid repletion of B12 levels in your body may cause certain symptoms including a jittery sensation or a sensation of too much energy.
These side effects are generally very limited and tend to go away rapidly.
But, like anything, you want to make sure that you are using the right dose for your body.
Most standard supplements, my recommendation as well, include a sufficient amount of B12, folate, and other B vitamins.
B12 Shots vs Oral B12 Supplements
There are two main ways that you can take B12 supplements.
The first is through oral capsules or tablets of Vitamin B12.
The other is through a B12 injection which is injected subcutaneously or intramuscularly.
In my practice, I’ve used both forms and I’ve had success with both.
I personally believe that B12 shots work great, especially for those with hypothyroidism.
However, despite my own opinions and clinical experience, I should point out that clinical studies do not necessarily show that there is a difference between using the shots or using oral supplements (10).
In addition, because the shots are so expensive (compared to the supplements) and because there is a small risk of injection site issues (such as bleeding or infection) it’s often recommended that the shots be avoided.
Despite these differences, I still think that B12 shots can be far more effective than oral B12 supplements for certain people.
I don’t know exactly why it occurs, but I’ve seen numerous patients who take oral B12 supplements who aren’t responding but who respond incredibly well to B12 shots.
It’s possible that B12 shots are more quickly metabolized and enter the body quickly through the subcutaneous route which allows for rapid utilization and reduced breakdown in the liver.
Again, I’m not sure as to why certain people seem to respond better to B12 shots vs oral B12 supplements but it’s worth knowing.
If you are someone who hasn’t been responding well to your B12 supplements then you may want to consider a trial of B12 shots.
They are somewhat more expensive, but you can usually purchase them for around $10.00 to $15.00 per shot.
They also typically last much longer so you only need 1 shot each week if you choose to go this route.
Conclusion
If you have hypothyroidism and you are struggling to feel back to your normal self then it would be a good idea to evaluate your B12 levels and consider supplementation.
Don’t lean too heavily on your serum B12 levels, however, and make sure that you are supplementing with a pre-methylated and activated version of B12.
Both methylcobalamin and hydroxycobalamin should work, but be sure to avoid supplements that contain cyanocobalamin.
Lastly, if you are not responding to oral B12 then you may want to consider using B12 shots.
Now I want to hear from you:
Do you have the signs or symptoms of B12 deficiency?
Did you respond to oral B12 supplements?
Have you ever tried B12 shots?
Which one worked best for you?
Leave your questions, comments, or concerns below!