Your anti-TPO antibody levels mean that your thyroid may be functioning sub-optimally.
The presence of these antibodies indicates an inflammatory state in your body that needs to be treated.
You can focus on certain therapies to help reduce these antibody levels and improve your thyroid function.
In this guide, I will walk you through optimal ranges for thyroid lab tests (including thyroid peroxidase antibodies), the complete symptom list for patients with autoimmune thyroiditis, and 5 steps to reduce these antibody levels.
Let’s dive in:
What your anti-TPO levels mean for your Body
Maybe you’ve just found out that you have elevated anti-TPO antibodies, or maybe you are experiencing hypothyroid symptoms with “normal” thyroid lab studies…
In either event, it’s important to understand what these antibodies mean for your body.
The presence of anti-TPO antibodies in your bloodstream is an indication that you may have an autoimmune condition.
In this case, it’s an autoimmune condition targeted to your thyroid gland.
The presence of anti-TPO antibodies is an indication that your immune system is not working properly.
These antibodies represent your body mistaking your thyroid gland as an enemy tissue and an attempt to destroy that tissue.
This is what is meant by auto (meaning yourself) and immune (meaning immune system).

Putting this together means your immune system is attacking your own body.
Obviously, this isn’t ideal, and we are going to talk about how to diagnose, manage, and treat this condition throughout this article but I want to focus on a couple of other topics before we get there.
First, you need to realize that the presence of these antibodies indicates that your immune system is NOT working properly.
Autoimmunity is also associated with some degree of inflammation (this varies based on the individual but it is always present).
Autoimmunity and inflammation in your thyroid are important for several reasons:
1) Your thyroid controls multiple functions in your body including your metabolism (1) (Low metabolism leads to weight gain, fatigue, and a low body temperature).
2) Your thyroid helps influence other hormones in your body(low thyroid leads to hormonal imbalances like low progesterone (2)).
3) If this autoimmune condition, if left untreated, can result in permanent damage to your thyroid gland(this also means that not all cases of elevated anti-TPOs need to be treated).
4) Symptoms of autoimmune thyroiditis do not necessarily match regular cases of hypothyroidism(meaning it can be difficult to diagnose).
5) This autoimmune condition may result in episodes of hyperthyroidism (3) and episodes of hypothyroidism due to glandular damage
The presence of these antibodies changes management completely due to the reasons provided above.
This is actually a good thing because it means that you have a chance to treat the condition and manage some of the symptoms yourself.
It also means the earlier you get started to treat the condition the more of your thyroid gland you can save and protect.
- Bottom line: The presence of anti-TPOs in your bloodstream indicates the presence of autoimmunity and inflammation. This condition should be differentiated from regular hypothyroidism which means that the treatment for this condition is different.
DOWNLOAD FREE RESOURCES
Foods to Avoid if you Have Thyroid Problems:
I’ve found that these 10 foods cause the most problems for thyroid patients. Learn which foods you should avoid if you have thyroid disease of any type.
The Complete List of Thyroid Lab tests:
The list includes optimal ranges, normal ranges, and the complete list of tests you need to diagnose and manage thyroid disease correctly!
Hashimoto’s and Autoimmune Thyroiditis – why making the diagnosis matters
The presence of anti-TPO antibodies in your blood is an indication of autoimmune thyroiditis.
In a general sense, this means that your body is attacking your own thyroid gland (for reasons we will discuss further below), and the term autoimmune thyroiditis is meant to define this condition as a broad term.
The condition you may be familiar with is Hashimoto’s thyroiditis which is another form of autoimmune thyroiditis.
You can find the full list of autoimmune thyroiditis conditions here.
So why does the presence of these antibodies even matter?
It turns out that it matters quite a bit.
The presence of anti-TPO antibodies changes treatment completely and it means that more must be done to reduce inflammation and autoimmunity.
Unfortunately, many providers, physicians, and endocrinologists take the “wait and see” approach to managing these conditions.
In addition, many cases of autoimmune thyroiditis are missed because routine testing for TPO antibodies is not commonplace.
Most patients are told to do nothing until their thyroid gland stops functioning well before they are put on thyroid hormone medication.
This is unfortunate for many reasons which we will discuss below, but primarily because leaving the inflammation may lead to permanent gland damage over time.
This is why many patients with undiagnosed autoimmune thyroiditis need to be on thyroid medication.
The constant damage from their own immune system may result in permanent damage to their thyroid gland.
The good news is that not all patients with autoimmune thyroiditis need thyroid hormone (as long as they catch the diagnosis early).
The presence of these antibodies also indicates that you have several other problems in your body that may need to be addressed including (these problems often trigger the autoimmune component):
- Nutrient deficiencies (4)
- Gastrointestinal issues (like increased intestinal permeability)
- Hormone imbalances (5)
- Active inflammation coming from somewhere inside your body
- Potentially other autoimmune diseases (or an increased risk of developing other autoimmune diseases)
Treating these conditions can actually IMPROVE thyroid function and reduce your symptoms without taking any thyroid hormone.
This provides a huge opportunity for patients to actually help themselves, as long as they have some direction and know where/what to look for.
- Bottom line: Determining the difference between hypothyroidism and autoimmune thyroiditis is very important because the treatment is different for both conditions. The presence of autoimmune thyroiditis indicates that other organs and systems in the body are involved and must be treated for the best results.
Symptoms of autoimmune thyroiditis differ from regular hypothyroidism
Much like the treatment for autoimmune thyroiditis differs from regular hypothyroidism, so do the symptoms of both conditions.
Having elevated anti-TPO antibodies is often associated with diffuse and unusual symptoms that don’t necessarily correlate with traditional symptoms of hypothyroidism.
These unusual symptoms often lead patients and providers down the wrong path and make diagnosing autoimmune thyroiditis and Hashimoto’s more difficult.
To make this easier I’ve included these non-specific symptoms below.
Symptoms associated with elevated anti-TPO levels:
- General fatigue or sensation of being “run-down”
- Mild weight gain(usually 5-10 pounds)
- Flat affect or depressed mood, not feeling like yourself
- Mild difficulty with concentration or inability to focus
- Dry skin, cracked lips, dry & brittle hair, non-specific rashes or patches on the skin
- Mild constipation
- Mild fluid retention(especially in the face and lower extremities)
- Voice hoarseness or sensation of a “swollen throat”
- Reduction in sweating or inability to sweat
- Mild joint pain or muscle aches
- Changes to the menstrual cycle may include an irregular cycle, reduced/increased flow, etc.
As you can see these symptoms are very non-specific.
As a result, many of these symptoms tend to be ignored (usually by Doctors), leading them to test for non-specific conditions such as anemia.
Ultimately many of these symptoms get lumped into the category of depression, and many physicians may recommend the use of anti-depressants instead of the correct treatment to manage thyroid function and reduce autoimmunity.
If these symptoms are ignored, or proper treatment isn’t instituted then these symptoms may evolve into overt symptoms of hypothyroidism.
This process largely occurs due to thyroid gland damage.
The signs and symptoms above should be a warning that this process is happening and worsening symptoms indicate that the disease may be progressing.
While you have glandular damage it’s actually possible to have episodes where thyroid hormone pumps into the body due to the damage and may cause symptoms of hyperthyroidism.
Below I’ve included a chart that tracks the TSH and FT4 levels over time in autoimmune thyroiditis and Hashimoto’s disease.
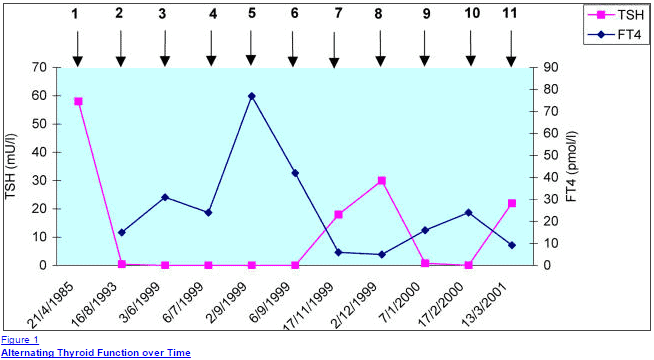
You can see that at times the TSH is incredibly high indicating a hypothyroid state, which then turns into a very suppressed TSH indicating a state of hyperthyroidism.
The symptoms between these states differ drastically.
While the TSH is high patients may experience the symptoms listed above in addition to the hypothyroid symptoms below.
While the TSH is low patients may experience symptoms of hyperthyroidism.
I’ve included a list of these types of symptoms as well to give you an idea of what type of symptoms you may be experiencing when hyperthyroid.
Remember that this episodic pattern can be missed unless you happen to check the TSH at the time you are symptomatic.
Hyperthyroid symptoms in patients with autoimmune thyroiditis and high anti-TPO antibodies due to changes in the TSH:
- Hot flashes or episodes of heat intolerance
- Mood changes but typically more anxiety
- Jittery sensation or sensation of “too much energy”
- Fatigue or episodes of low-energy
- Difficulty sleeping or episodes of insomnia
- Facial flushing or sensation of hot extremities
- Heart palpitations or sensation of a racing pulse (usually episodic and short-lived)
- Weight loss and increased appetite
These alternating symptoms of generalized non-specific symptoms, combined with episodic symptoms of hyperthyroidism make the diagnosis difficult to manage.
It’s important to realize that these types of symptoms do NOT occur in standard hypothyroid patients, making these symptoms important for both patient and physician to identify.
The presence of these symptoms should be a warning sign to look at antithyroid antibodies like anti-TPO.
But these aren’t all the symptoms that patients with autoimmune thyroiditis may experience.
In addition, these patients may also develop symptoms of overt hypothyroidism (the more traditional symptoms).
This typically occurs once the inflammatory component has “died down” and gland damage has set in.
To give you an idea of what these symptoms look like I’ve also included the more common symptoms of hypothyroidism that may occur.
Traditional symptoms of Hypothyroidism:
- Extreme fatigue and/or exhaustion(inability to do basic activities)
- Moderate weight gain of 20 to 30 pounds
- Overt hair loss, hair thinning, and hair breakage
- Changes to mood, predominately depression
- Menstrual irregularities and other conditions like PMS/PMDD
- Chronic and debilitating muscular/joint pain
- Chronic and daily constipation, development of other GI issues like gas/bloating, acid reflux, and low stomach acid
- + any of the other generalized symptoms listed above
Note that the presence of these findings usually represents that the disease has been around for some time and may have progressed.
The important part is to identify the presence of these symptoms and then seek treatment which we will go over further below.
- Bottom line: Symptoms of elevated anti-TPO antibodies may range from generalized and very non-specific, to episodic symptoms of hyperthyroidism. Over time these symptoms may progress to generalized hypothyroid symptoms as gland damage occurs.
Anti-TPO antibody levels and ranges – what is considered normal?
One of the most frequent questions I get asked by patients is something along the lines of this:
“Are my lab tests normal?”
Believe it or not, it’s actually pretty easy to determine if your labs are normal vs abnormal and I will walk you through it.
The first thing you need to realize is that there is a big difference between “optimal” and “normal”.
When you are evaluating your thyroid lab tests you want to look at the “optimal” lab values that I will be discussing.
These values will most likely differ from the “normal” ranges that your general physician will use when determining if your lab tests are indeed normal.
This results in much confusion among patients which leads them here to ask me if their tests are normal.
They tend to get conflicting information so let’s set the record straight.
First, let’s talk about your thyroid peroxidase antibody levels (AKA anti-TPO levels).

The presence of these antibodies is not normal and indicates a problem.
In some cases the presence and significance of anti-TPO antibodies (like in pregnancy (6)) are unclear, but one thing is for certain – it is not normal.
In the example above the presence of anti-TPO antibodies indicated a higher risk of pregnancy complications and mental health issues later in life, but didn’t necessarily correlate with thyroid function.
As a rule of thumb, let this be your guide:
If you have the symptoms I have listed above plus you also have abnormal thyroid lab tests or elevated TPO antibodies then you definitely have abnormal thyroid lab tests.
Symptoms + anti-TPO antibodies = poor thyroid function
To give you an example of what your thyroid peroxidase antibody levels might look like I’ve included a lab result from a patient of mine:

In this example, you can clearly see that the result is very abnormal.
The result is 1317 with a standard reference range of less than 6.
This is a classic example of a patient with elevated anti-TPO antibodies and a poorly functioning thyroid.
You can also see her corresponding TSH which is obviously abnormal as well.

In this example, a TSH of 7.024 and an anti-TPO level of 1317 confirm that her thyroid is indeed abnormal.
Unfortunately, not all cases are as straightforward as this, which is why I will go over the other optimal thyroid lab studies below and help explain why you may have “normal” thyroid lab tests but still be symptomatic.
- Bottom line: The presence of elevated anti-TPO antibodies is always a problem. In the presence of the symptoms listed above, it is an early sign of thyroid dysfunction and should be treated aggressively.
Normal thyroid lab tests but still have hypothyroid symptoms?
This idea of “optimal” thyroid lab tests extends beyond just anti-TPO levels.
Unless you evaluate your thyroid lab tests entirely and with the “optimal” levels in mind, you will end up undertreated and may remain symptomatic.
Part of this problem is due to the reliance upon the TSH as the de facto lab test to determine thyroid function.
The current (and insufficient) treatment paradigm can be summed up in basically one sentence:
Give Levothyroxine or Synthroid to the patient and monitor the TSH to “normal” levels.
It turns out that thyroid hormone management is not quite that simple and several studies have shown that treatment based on TSH ultimately leads to low levels of T3, reduced quality of life, and weight gain due to a slower metabolism (7).
When you look at all the data out there and our current treatment paradigm it’s easy to see why many hypothyroid patients go under-treated and misdiagnosed.
Because of these reasons, it’s very important to have a basic understanding of what defines “optimal” thyroid lab tests and use these values to determine the need for further management (and to determine if your tests are indeed “normal”).
Complete thyroid lab panel + optimal ranges:
- TSH: Your TSH should be less than 2.0, healthy levels are generally below 1.0(this only applies if you aren’t on thyroid medication already)
- Free T3: Should be in the upper 50% of the reference range to be optimal (doesn’t apply if you are on thyroid medication)
- Free T4: Should be in the upper 50% of the reference range provided by the lab(doesn’t apply if you are on thyroid medication already)
- Reverse T3: Optimal levels should be as low as possible(applies on or off of thyroid medication)
- Anti-TPO antibodies: Optimal levels should be non-existent or as close to 0 as possible depending on reference ranges(applies on or off thyroid medication)
- Thyroglobulin antibodies: Optimal levels should be as close to 0 as possible(applies on or off thyroid medication)
Part of the problem with diagnosing hypothyroidism is due to the body’s amazing ability to preserve serum thyroid levels under situations of extreme stress.
In addition, when it comes to hormones and serum levels, very small changes in blood levels can mean drastic changes in terms of function which results in symptoms in patients.
Combining these two factors it’s easy to see why reliance upon one test (generally the TSH) is a recipe for misdiagnosis when treating hypothyroid patients.
Here is an example of a set of lab tests that were considered “normal” but in reality are very suboptimal.
This patient also presented with hypothyroid symptoms including weight gain, fatigue, a slow metabolism, and hair loss.

You can easily see that all of these thyroid lab values fall within the “normal” range, but when you compare her to the “optimal” levels provided above you get a completely different picture.
Her Free T4 is low at 1.28 and her reverse T3 is quite high at 18.8.
This pattern is classic for what is known as low T3 syndrome or non-thyroidal illness and it is well recognized even by conventional medical sources (even though most endocrinologists and PCPs are not willing to treat it).
I’ve provided an image copy from emedicine.com which outlines the need to evaluate all of these lab tests and even shows that T3 levels can help in diagnosing certain patients with Hashimoto’s by identifying this pattern.
You can see the complete article here.
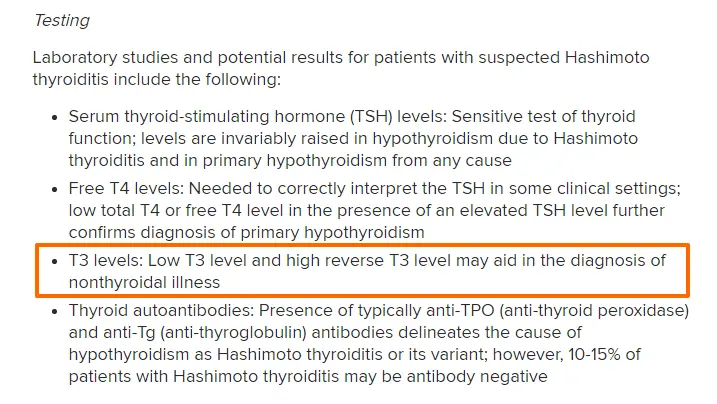
Unfortunately despite the fact that this condition is well recognized in patients with high levels of anti-TPO antibodies not much is done by physicians to treat it, and even fewer physicians are even willing to order the right tests.
Because of this, it is very important to find physicians who are knowledgeable about these thyroid lab tests, willing to order them, and willing to treat them if present.
I’ve written about the connection between low T3 and weight gain and how to properly address the condition previously.
Other diseases associated with Autoimmune thyroiditis and elevated anti-TPO antibodies
Not only will high levels of anti-TPO antibodies damage your thyroid, but it also is important to identify because the presence of this autoimmune disease increases your risk of developing other autoimmune diseases.
Studies have shown that patients with Hashimoto’s and autoimmune thyroiditis conditions have a very large increase in developing other diseases like Celiac disease (8), type I diabetes mellitus, pernicious anemia, and even adrenal insufficiency.
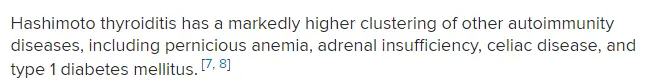
For this reason, the early detection of thyroidal antibodies becomes very important.
Treating and reducing the immune and inflammatory components of this disease can help reduce the risk of developing these other autoimmune diseases.
The presence of TPO antibodies in your blood should prompt your physician to order other tests to evaluate your autoimmune status.
This is particularly important in the case of Celiac disease which is so often undiagnosed and underappreciated (much like thyroid disease!).
Below I’ve included an example of a patient of mine who had elevated anti-TPO antibodies on initial testing (along with other abnormal thyroid tests) and further evaluation of her antibodies to gluten revealed she also had antibodies to the gluten protein.

You can see above the high titers to tissue transglutaminase (9) and gliadin antibody, both of which can be markers of the condition of Celiac disease.
It’s always very important to identify gluten sensitivity in patients because the removal of gluten can be curative (10) in this autoimmune disease (which can’t necessarily be said for other autoimmune diseases).
It’s also been shown that there is a strong connection between the GI tract, the immune system (11), and even the thyroid (12).
The presence of gluten in the diet sparks an inflammatory state (13) which may weaken the immune system and further reduce thyroid function (14).
Luckily, as long as it is identified, the removal of gluten is enough to drastically improve this process.
But this can give you an idea as to why it’s critical to order the right tests and get on the right treatment.
What causes anti-TPO levels to increase?
Now that you have an understanding of why your anti-TPO levels are important, we need to talk about what causes them to increase.
This is an important step because, as you might recall from earlier in this post, the immune and inflammatory component is treatable.
So if we can target the cause of the increase in these antibodies we might be able to actually lower them and then improve your condition overall.
It turns out that the cause of elevated TPO antibodies in each person will likely be different and will require some degree of “digging”.
Having said that, there are definitely some factors that remain consistent in most patients with elevated TPO antibodies.
#1. Low vitamin D
The first is low levels of Vitamin D.
Studies have shown there is a link between low levels of vitamin D (15) and the development of Hashimoto’s thyroiditis.
Recall that Hashimoto’s is a form of autoimmune thyroiditis and elevated anti-TPO antibodies indicate this condition is present.
These studies show that the lower the Vitamin D is the longer and worse the symptoms of Hashimoto’s become, the worse thyroid function becomes and the higher antibodies rise.
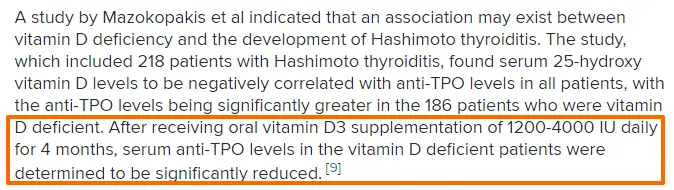
his likely has to do with the effects that Vitamin D has on the immune system (16).
Autoimmune conditions represent a problem in the way that your immune system understands what is “good” and what is “bad”.
When this system is off balance your body may create antibodies against its own tissue which results in various symptoms.
Increasing Vitamin D may be one of many ways to increase thyroid function and reduce both the autoimmunity and inflammation in autoimmune thyroiditis.
#2. Increased intestinal permeability
As I mentioned previously the gut has a strong influence on your immune system.
When diseases cause intestinal issues or inflammation it disrupts the tight junctions in the GI tract which are supposed to shield your body from breakdown products from food, bacteria, etc.
Poor diet, high stress, and nutrient deficiencies can weaken this protective membrane in the GI tract and lead to a condition known as increased intestinal permeability (17).
Increased intestinal permeability leads absorption of food products, bacteria, etc. that shouldn’t be absorbed into the bloodstream.
You can see an example of what I am talking about in the image below:
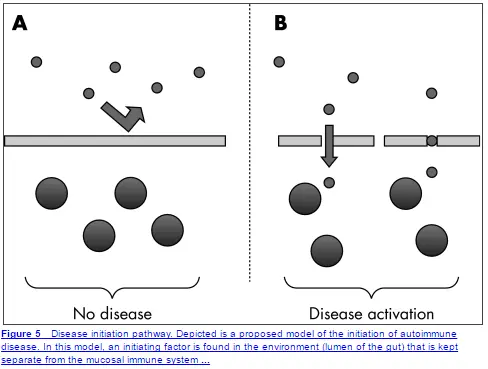
This image depicts what should be happening to a healthy intestinal membrane that blocks the absorption of everything but nutrients.
When this membrane is damaged you can see particles passing through the membrane and triggering disease states.
This whole process and condition are what is known as “leaky gut”.
Once the abnormal particles are absorbed they can trigger autoimmune conditions through a process called molecular mimicry (18).
What happens is that some of these food particles look very similar to parts of your body.
Your immune system creates antibodies to these particles which then cross-react with some of your own tissues leading to autoimmune disease.
This effect is frequent enough that it may be the underlying cause (19) in MANY cases of Hashimoto’s and autoimmune thyroiditis.
What you need to understand is that various factors influence this protective barrier.
High levels of stress, a diet high in processed foods, gluten sensitivity, and a lack of nutrients have all been shown to reduce the effectiveness of this barrier which may trigger high anti-TPO levels.
#3. Inflammation (especially gut inflammation)
Generalized inflammation is bad for many reasons, but in this section, I want to focus on GI inflammation.
You already know and understand the important role that the GI tract plays in immunity, but what you may not know is its role in thyroid function in general.
Inflammation in the gut leads to reduced T4 to T3 conversion, and reduced absorption of nutrients, and may predispose to conditions that can then trigger increased intestinal permeability (AKA leaky gut).
For these reasons, it’s important to identify and treat any GI-related problems that may be present in your body.
If you have any of the following symptoms you may be predisposed to develop autoimmune thyroiditis and high antibody levels:
- Constipation
- Diarrhea
- Irritable bowel syndrome
- Inflammatory bowel disease
- Acid reflux
- Low stomach acid
- SIBO/SIFO, or gas/bloating
- Functional abdominal pain
- Intestinal dysbiosis
Basically, if you are not having bowel movements regularly and if you have any of the symptoms or conditions listed above then you may be at risk.
Treating and reducing these inflammatory conditions will be necessary to reduce your risk and treat your antibody levels.
#4. Poor diet
Diet has been shown to influence both the immune system and inflammatory levels.
Diets high in processed foods (and industrial seed oils) have been shown to directly alter your immune system and predispose certain patients to develop autoimmune diseases (20).
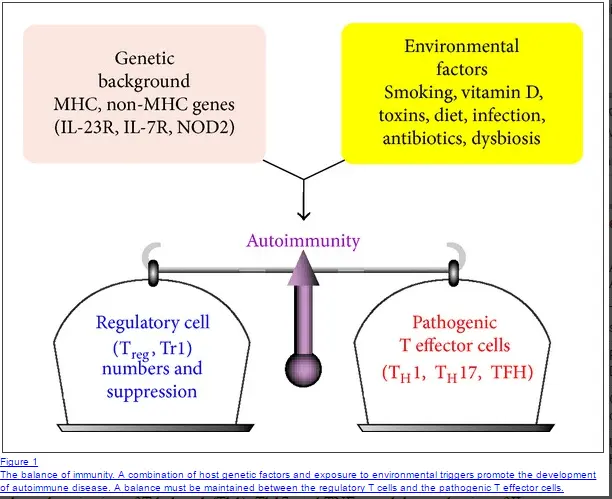
In certain individuals (those with certain genetics) changes in diet can actually trigger autoimmunity all by itself.
Environmental factors like stress, poor, diet, and nutrient deficiencies can actually alter your genes and shift the immune balance toward autoimmunity (21).
#5. High stress
Stress plays a huge role in the development of autoimmune diseases.
It’s been shown that up to 80% of patients report high levels of emotional stress prior to the onset of autoimmune disease (22) (all types but especially Hashimoto’s).
This is also confirmed in my own personal patient base in which I have seen the same thing.
For most cases of Hashimoto’s and autoimmune thyroiditis, there is a triggering event related to a stressful situation.
This stress can be emotional, physical, traumatic, etc.
The death of a loved one, a particularly difficult breakup or divorce, pregnancy, a medical illness in loved ones, etc. may all qualify as triggering events.
It’s important to realize that stress likely influences other factors that predispose the body to develop autoimmune disease, so mitigating stress levels is critical to lowering antibody levels.
Treatment options for patients with high anti-TPO levels
So what are you supposed to do if you have high anti-TPO antibody levels?
It turns out that there are several things you can do to lower these antibody levels.
The treatment is especially important because your physician may take the “wait and see” approach to treatment.
Basically, many doctors may not even try to treat your antibody levels until they have caused glandular damage and thyroid hormone replacement is required.
Luckily there are several therapies that you can do (some on your own) to help reduce inflammation and autoimmunity.
Note: for best results, it’s wise to use a combination of these therapies and stack them together. If you take just 1-2 supplements, for instance, you will be limiting your progress.
#1. Supplements
We’ve already discussed how certain nutrient deficiencies (low levels of vitamin D) can predispose to developing autoimmune diseases.
This should give you an idea of the importance of nutrients and supplements in treating these conditions.
Now we need to discuss how certain nutrients can reduce inflammation and have even been shown to lower TPO antibody levels.
Supplements to reduce inflammation and autoimmunity:
- Zinc: Zinc has been shown to reduce inflammation, boost T4 to T3 conversion (23), and act as an anti-inflammatory agent in the body. Couple this with the fact that many patients are zinc deficient and zinc supplementation becomes a no-brainer for hypothyroid patients. Use Zinc in combination with Selenium.
- Selenium: Selenium also acts as an anti-inflammatory agent and can boost T4 to T3 conversion. In addition, it has also been shown to reduce TPO antibodies in some patients with Hashimoto’s (24). The combination of zinc + selenium is particularly potent and I generally recommend using both simultaneously. Make sure that you use 50-150mcg of selenium each day and avoid using doses in excess of 400mcg per day to prevent toxicity.
- High-quality multi-strain and multispecies probiotics: Probiotics can help reduce inflammation in the GI tract and help repopulate the GI tract with anti-inflammatory bacteria to help promote T4 to T3 conversion. Probiotics should be considered standard therapy in patients with high TPO antibodies. Use probiotics daily (both with meals and in between meals) for 6 months for best results.
- Vitamin D3: Replacing low Vitamin D levels can help promote immunity. But make sure not to take Vitamin D3 without vitamin K2. The balance between these two fat-soluble vitamins is necessary for the best results. Aim for a Vitamin D level in the mid-range and supplement as necessary (usually 2,000-5,000 IU per day).
Supplements to improve thyroid function:
- Liquid Iron: Iron is required for proper thyroid hormone function and low levels should be replaced to achieve optimal levels. High iron levels can cause problems, however, so read this guide to determine if your iron levels are “optimal”.
- Magnesium glycinate: Studies show that the hypothyroid state causes your kidneys to excrete more magnesium which makes many hypothyroid patients magnesium deficient. Replacing magnesium levels can help improve thyroid function, improve your mood, reduce muscle/cramps, and increase energy levels.
- Iodine: Iodine is required for proper thyroid hormone production. Using the combination of iodine plus selenium can help improve thyroid hormone production and may help reduce the symptoms of hypothyroidism. Make sure to start out with a low dose and combine it with selenium. Some patients may react negatively to iodine so monitor your symptoms closely.
You can also check out a more detailed guide on which supplements to take if you are hypothyroid here and which supplements to take if you have Hashimoto’s here.
#2. Medications
In addition to using supplements, there are some medications that can be used to help reduce inflammation.
The medication I am referring to here is known as low-dose naltrexone.
I’ve already discussed how LDN can help with weight loss in the past, but here I want to focus on its ability to reduce inflammation.
Through largely unknown mechanisms, LDN has been shown to reduce inflammatory states (25) and can be used as a novel anti-inflammatory medication.
Some studies have shown that LDN may result in the remission of some autoimmune diseases (26).
It should be pointed out that LDN does not work for every person.
For this reason, it’s helpful to at least consider a trial of the medication, especially in patients who have multiple autoimmune conditions, weight loss resistance, and/or elevated anti-TPO antibodies.
In my experience, roughly 30-50% of patients obtain significant benefits from using LDN.
Fortunately, even for those who use it and don’t get any noticeable benefit at least, there is no harm in using the medication.
I’ve successfully used LDN in the past in patients with weight loss resistance and Hashimoto’s, you can read case studies here.
#3. Hormones
Believe it or not, certain hormones in your body are necessary for proper immune function.
The hormones I want to focus on today are the androgens.
As you may know, women tend to get autoimmune diseases more frequently than men do.
Part of the reason for this discrepancy between the sexes is felt to be due to testosterone levels in women vs men.
Higher testosterone levels have been felt to be somewhat protective against the development of autoimmune diseases.
In addition, studies have shown that testosterone replacement (27) therapy has a positive effect on several autoimmune diseases (28).

What is interesting from my point of view is that almost every patient I treat who has high thyroid peroxidase antibodies also has a corresponding low testosterone level.
Some of this may be due to thyroid hormone and its effects on testosterone levels, but I have also noted improvement in autoimmune diseases with testosterone replacement.
If you have a diagnosis of autoimmune thyroiditis it’s important to get the following labs tested (and again make sure that you are evaluated with the “optimal” ranges in mind):
- Free and total Testosterone: If your levels fall within the bottom 50th percentile of the reference range then you might consider testosterone replacement therapy. You can read more about how to use testosterone cream here, you can also find symptoms of low testosterone in this post as well.
- DHEA (29): DHEA is a precursor hormone to testosterone and estrogen, but still classifies as an androgen in the body. DHEA is also involved with the immune system and low DHEA levels may predispose certain patients to develop autoimmune diseases. Unlike testosterone, DHEA is available over the counter and can be supplemented. Be careful when supplementing with DHEA, though, as it can potentially turn into estrogen metabolites. Start with 25mg every other 1-2 days as tolerated (make sure it comes in the micronized form to promote absorption).
#4. Diet
We’ve already discussed the importance of diet and how it impacts inflammatory levels and the immune system.
In this section, I just want to provide you with several diets that you should consider if you have elevated TPO levels.
Changing your diet should really be one of the first steps you take.
Changing your diet is something that you are in control of and it can have a huge impact on your status overall.
Other factors are not in your control: what thyroid medication you take, your dose, etc.
Because of this, it’s important to take advantage of the variables that you can.
With that in mind, I’ve provided 3 diets that I have used successfully in my clinic:
- Gluten-free + dairy-free: We’ve already discussed how gluten can impact immunity and removing gluten (even if you are gluten antibody-negative) has the potential to help you considerably. Dairy is removed because many people cross-react to both gluten and dairy.
- Paleo diet: The paleo diet is a great starting point as well. There are many guides and recipes online that can help get you started. The only potential issue with the paleo diet is the relatively limited amount of carbs that it allows. Some alterations to your carbohydrate intake may be necessary if you start on the paleo diet.
- Autoimmune protocol: The AIP diet is a more restrictive form of the paleo diet and removes other food groups like nightshades. Because this diet is more restrictive than the others I generally don’t recommend patients start here unless they have multiple autoimmune diseases.
You can read more about how to pick the best diet for you if you have Hashimoto’s in this detailed post.
#5. Avoid endocrine disruptors
Endocrine disruptors refer to various chemical compounds that get absorbed into your body and may interact with hormone functions.
Unfortunately, endocrine disruptors are very common nowadays and are found in various forms of plastics, containers, and even on receipts.
These chemicals can be absorbed through your skin, get into your bloodstream, and impact thyroid function.
Endocrine disruptors (EDCs) have been shown to lower free T3 levels without having an impact on TSH (30).
The effects of these chemicals are often missed unless the T3 is actually tested.
Actively avoiding these chemicals is necessary if you want to improve your thyroid function.
Fortunately, several steps can be taken to dramatically reduce the impact of these chemicals:
- Drink out of glass containers(avoid plastic containers)
- Drink filtered water only
- Stop touching receipts(have the cashier place them in the bag)
- Avoid hand-me-down plastic toys
- Eat organic foods and grass-fed meats
- Check your cosmetics for added chemicals (putting EDCs on your face is a good way to rapidly absorb these harmful chemicals)
Following these simple steps is an easy way to avoid these chemicals.
For some patients, it may be necessary to detox these chemicals more actively because they can be stored in the fat (we will discuss this concept in another post).
Recap & Final Thoughts
The presence of anti-TPO antibodies is never a normal sign.
The presence of these antibodies combined with hypothyroid symptoms may indicate autoimmune thyroiditis.
If you are experiencing hypothyroid-like symptoms then you should have a complete thyroid lab panel checked which includes antithyroid antibodies.
Due to the various issues with diagnosing and managing thyroid abnormalities, it will be important for you to have a basic understanding of how to diagnose and manage your condition.
Because autoimmune thyroiditis indicates both an inflammatory and autoimmune condition, it is treated differently from hypothyroidism.
For best results, patients should focus on a combination of supplements, diet, stress reduction, and hormone replacement to reduce this inflammatory state.
Doing this early may help to preserve thyroid function long term.
Now it’s your turn:
Are your TPO antibodies elevated?
Are experiencing any of the symptoms of hypothyroidism or hyperthyroidism?
Leave your comments below!
Scientific References
#1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4044302/
#2. https://www.ncbi.nlm.nih.gov/pubmed/9846161
#3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1140938/
#4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1542505/?page=1
#5. https://www.ncbi.nlm.nih.gov/pubmed/17261796
#6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4518419/
#7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4790206/
#8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2111403/
#9. https://www.ncbi.nlm.nih.gov/pubmed/10445548
#10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3002532/
#11. https://www.ncbi.nlm.nih.gov/pubmed/23426535
#12. https://www.ncbi.nlm.nih.gov/pubmed/20351569
#13. https://www.ncbi.nlm.nih.gov/pubmed/23253599
#14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4802023/
#15. https://www.ncbi.nlm.nih.gov/pubmed/23337162
#16. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3166406/
#17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1856434/
#18. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3266166/
#19. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1774342/
#20. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4034518/
#21. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3945069/
#22. https://www.ncbi.nlm.nih.gov/pubmed/18190880
#23. https://www.ncbi.nlm.nih.gov/pubmed/8834378
#24. https://www.ncbi.nlm.nih.gov/pubmed/11932302
#25. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3962576/
#26. https://www.ncbi.nlm.nih.gov/pubmed/24558033
#27. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2724009/
#28. https://www.ncbi.nlm.nih.gov/pubmed/3097058
#29. https://www.ncbi.nlm.nih.gov/pubmed/3097058
#30. https://www.ncbi.nlm.nih.gov/pubmed/26414233



How do I purchase all the supplements you have recommended for off the scale antibodies?
Hey Sue,
If you click on the name of the supplement it will take you directly to my recommended brand of supplement. I only recommend supplements that I have used on my patients successfully.
Fantastic publication, as usual! Thank you for all your effords, Dr. Childs.
Hey Daniela,
No problem and I’m glad you enjoyed it.
I have Hashimoto’s and have had a thyroidectomy and after 16 years, still can’t find a doctor that can help me. I am willing to travel if needed and do whatever it takes to feel better. Can I please get my name on a waiting list.
Hey Erica,
I’m sorry to hear about your situation but unfortunately I don’t have a waiting list at this time.
Dear Erica
I’m really sorry to hear about your problem. I do suffer from the same disease, though. I live in Iran and I was diagnosed with hyperthyroids when I was in school- about 13 years ago.. i was happy that I could eat everything and lose weight… i was a child I know… my Endoc, one of the best in his field, had me on the list of idoein surgery. I wasn’t ready for that and i prolonged the process.. all my mistake.. i didnt listen to my doc and didn’t take the med regularly. to make the story short, it had a serious effect in my brain and i finally went under radioactive surgery. I started gaining weight the following day, again being foolish, i didn’t follow the treatment regualrly and gained 14 kilos within one year, i have ALL the symptoms dr Childs has mentioned;)) but I saw my doc yesterday, he was very angry with me and i promised myself to listen to him this time… just the day before yesterday, i admitted to myself that i needed help and that i wasn’t ok… my anti Tpo was 51!!!!!!!!!!!! Shown in the blood test:) and my TSH was 20:) you can come to Iran if you are willing to travel, I can guarantee that my doc is really good- no offense to dr Childs- the problem was that I didn’t listen:)
Dr Childs,
Thank you so mich for your post. It was really helpfull.
Hi Rosa
Were the meds your doctor prescribed Thyroid Hormone replacement like Thyroxin? If so the problem with hormone replacement meds, is once you start taking them your body stops producing the hormone naturally. If you stop taking meds your body has no hormone and then you become sick, as your body has stopped producing hormone naturally
I’m not a medical professional, but this is what I’m led to believe after speaking to doctors and research on hormone replacement. This probably why you are on meds for life once you start. (Forgive me if I’m wrong)
I am trying to avoid going on medication. I have very high anti TPO and high TSH.
Hi Andy,
That is true, thyroid medication will suppress the ability of your body to produce thyroid hormone naturally, but the suppression is only temporary and it isn’t necessarily a big problem if your thyroid is not able to produce that thyroid hormone on its own.
Have you had your hormone levels checked
Low testosterone perhaps
Moringa helps with energy
I too have hashimotos
I find your articles to be the most informative, factual, and useful out there among all the hashi gurus. You are correct in saying that most of us have a hard time finding what optimal Levels should be in printed literature today. I love how you usually add those within your emails.
Hey Shannon,
I hope you find them helpful. It’s difficult to discuss diseases like hashimoto’s when the disease can vary drastically from patient to patient, which can lead to a lot of confusion.
After 2 years of asking my Endo finally gave me a script for LDN, however it is for .5 mg. Will I see any benefits from such a low dose?
Hey Doreen,
Maybe, but probably not, it just depends on your body and your metabolism.
How have you been on the new prescription?
I have a great doctor although not as good as you I don’t believe , but I did have high RT3 , got it down way down and my FT3 is optimal but my hashimoto antibodies have not gone down the whole 4 years since diagnosis. could it be because I looked for a doctor to help me for 15 years and the attack on thyroid was just too much to recover fully?
Also does a undiagnosed and unmedicated hashimotos for over 15 years cause so much damage that my metabolism can only handle 1000 calories
Hey JJ,
All of those things are possible, but not not likely. Instead they are probably due to other hormone imbalances, suboptimal thyroid levels, etc.
Dr. westin,
I appreciate all of the information on your website-I was diagnosed with Hashimoto’s Thyroiditis in October of 2012, I went through Two Endo’s, and now, I am working with my Primary Doctor-She is very open to natural Supplements for the Thyroid, and she is switching me from Levothyroxin to Synthroid-No synthetic-Costs more, but I’m worth it. These symptoms are miserable-I will also start taking a pre-probiotic, along with selenium and Zinc. I do take Vit D3 with K2(5,000, Fish Oil, Calcium, CoQ10, Multiple for 50 Plus(Powder form-Nutrametrix). I havenot had a chace to take a look at the Hashimotos Diet yet-I have eliminated dairy, Soy, artificial colorings, Sugar, wheat, from my diet. Any suggestions about me growing my hair back. Thanks, Carla L.
Hey Carla,
I am creating a post on how to help grow back your hair and it will probably be ready within the next 1-2 weeks.
Awesome! I cannot wait for your post on how to grow back hair.
Dr. Westin
Fantastic article. Very informative. I am appreciative of all the information you provide.
Hey Claudia,
No problem, I’m glad you enjoyed it.
This is a very detailed report you make on TPO. Thanks.
Hi Amit,
No problem! Hope it helps.
Dr. Childs,
Why in the paper you have mentioned that the optimal references for TSH, T3 and T4 do not apply if we are on a thyroid medication?
In case on thyroid medication what will be our target – symptom free condition or sth else?
In addition what kind of D vitamin should be measured 25OH or 1,25OH in order to be supplemented properly. Do we really need vit D supplements. According to some new studies (Tim Spector “The Diet Myth”, 2013) vit D supplementation could be dangerous in some aspects?
Thank you in advance!
Hey Daniela,
I haven’t really shared how I base dosing recommendations off of thyroid lab tests, so this interpretation is much different than for those not on thyroid medication already.
And yes, that’s why I only recommend the use of Vitamin D with Vitamin K2 and in smaller doses.
I have never commented on a website before, but this time it’s a must. I just want to sincerely thank you for writing in a manner that’s easy to understand and not over my head. I have been trying to educate myself on hypothyroidism and hashimotos for over 30 years and have never understood it. You make it so easy to understand and I find myself wanting to read more. Thank you, thank you, thank you, maybe there is hope to these issues.
Hey Molly,
Thanks for stopping by and I hope it helps!
Hello Dr. Westin, Thank you for helping so many of us sort out this Thyroid Hormone mess. Your explanations of what’s happening are so much better, to the point and easier to comprehend than anything I have read.
I too have been years trying to deal with this thyroid and hormone problem for changing doctors in search of someone knowledgeable. Only recently my newest doc has ordered the Hasimotos antibodies test.
First time I have had a doctor order this, but after reviewing the test she said everyone has thyroid antibodies and these numbers are too low to worry about??? Is this true? She also said she wants me to get a PAP test and Mammogram before giving me compounded hormone cream as a precaution since there is family history of cancer.
I had taken compounded hormones from my previous doctor who has since retired. I think it did make me feel better I have been off them for some time now.
Could you please give me your opinion regarding results below? and cancer risk with compounded hormones if you have a family history of cancer?
Thyroid Peroxidase Abs 16.8 ref range <35
Thyroglobulin Abs 10.3 ref range <115
Other test results show:
Reverse T3 9.2 range 8-25
T3 Free 2.5 range 1.8 – 4.6
T4 Free 1.04 range 0.9 – 1.7
TSH 3.690 range 0.27 – 4.2
Total Testosterone <2.50
Testosterone Free <0.02
Progesterone 0.24
Estrone (E1) 13.7
Estradiol (E2) <5.00
Pregnenolone 51
I have terrible fatigue, can't sleep through night,losing hair etc. all the classic symptoms of hypothyroidism.
Thank you for your input it is greatly appreciated!
Sheree
Hey Sheree,
The best thing you can do for your health is find someone who is knowledgeable about hormones and thyroid testing/treatment, you will probably have to look outside of the insurance model for the best care.
Hi Sheree,
Just following up on your post here. I am going through similar symptoms now and my doctor keeps telling me everything’s “normal.” My mom had a complete thyroidectomy because she had cancer. My TPO (thyroid peroxidase) is 900. I still don’t know why I am being treated here. Did you end up getting treated?
Thanks,
Elsa
Been following most of what your suggesting. Being a male Hashimotos patient makes things a little different for us. Im being treated by. VA Endo who works with me. I follow my labs closely and do see a Functional Doctor outside of the VA. Thank you for your reasearch and info. Do you jave a mailing list could you please add me. Thanks again, Earl Tallman
Hey Earl,
No problem and I hope it is helpful, and I agree that males are much different. If you haven’t already you can check out this post as well: https://www.restartmed.com/testosterone-weight-loss/
Dr. Westin- Great read especially after I was told today by a doctor that there is no cure for elevated antibodies or Hasimotos!I was diagnosed with Hasimotos in Oct. 2016. I’ve come across several websites (and yours being one of them) that it can be reversed through healing ones gut and reducing the inflammation. I took some baby steps and stopped gluten, eggs, dairy and soy. Within 48 hours I could feel the reduction of inflammation, clearer thinking and reduced heart palpitations to the point of non existence. However I still get the Hypo/Hyper swings but not as frequent or as bad. I also take a small amount of Nature Thyroid of which this MD told me that it may be the cause of my problems. My antibodies were at 34 and 6 weeks later at 27.(The test were done before I eliminated the foods) I have another test coming up so it should be interesting to see where the antibodies are at now.
Thanks again for a hope that I can regain my health and get back to running the way I use to!
Hey Heather,
No problem and I hope it helps, good luck on your recent tests and keep us updated.
Dr. Childs….I was diagnosed with Hashimoto’s in October 2016, Peroxidase at 4429 and antiglobulin at 880, I have been on the gluten/dairy free and just has Armour uped to 30mg. My TSH numbers are all over the place the last 6 months from 7.94 to 2.0 and also A1C showing that I am prediabetic. I have been trying to get my DO to prescribe LDN to help lower the antibodies but she will absolutely not even consider LDN. I have heard many good things and would like to try. Suggestions on how to get LDN? Do you do consults? It is soooo very difficult to find someone who is genuinely interested in Hashimoto’s. I know I am not alone and many are worse off than me but I want to be pro active. I have developed chronic hives that I cannot get under control and allergist is now wanting to treat with Xolair. I feel hopeless that I will ever find someone who REALLY can help. Thanks from a grandma who wants to be around for a long time for my granddaughters.
Hey Pamela,
You definitely want to find someone knowledgeable near you that can help you further. Going it alone will end up wasting precious time in your life and leave you feeling terrible for longer than necessary, you may need to search outside of the insurance model to find proper care.
Where have you been the last year of my life!? 🙂 where do you practice? Do you do telemedicine or Skype appointments? If no do you recommend a provider in Portland, OR? I am so grateful I found your blog. Thank you for all the tips.
Hey Heidi,
Unfortunately I am not accepting patients and I don’t know anyone who practices like me that I can refer you to.
Actually I have been watching and reading about Dr. Westin for a few months now and then I believe from his site somewhere I was able to find out more information as to where I could go and be treated. I was disappointed that he does not take patients, but I did find this site to be helpful to find one that maybe close to him and the approach that he takes. He is great, so this is just a suggestion. I have been looking a long time and this is the closest I can find.
Functional Medicine Doctors:
https://www.functionalmedicine.org/practitioner_search.aspx?id=117
You can search on this list to find a doctor in your area! Good Luck
Hey Nancy,
Thanks for providing that info. I would point out that nowadays the quality of care from those that practice “functional medicine” has been somewhat variable, which is why I have been hesitant to promote that website here. As always, just make sure you do research prior to making your first appointment to ensure that you are getting proper care.
I am so confused on T4. I am on 90mcg of NP Thyroid and T4 is always flagged as low. Since I am on the NDT should I be concerned about low T4? Is there a link for optimal levels for those of us on NDT? Still gaining weight and unable to lose anything despite walking 2 miles per day. Doctors I see insist that it has nothing to do with the thyroid.
Hey Stacy,
I haven’t discussed how to interpret lab values if you are already on certain types of thyroid medication. I may outline this in a future post, however.
I would love to know more about optimal lab values while on meds – so much conflicting info out there! really enjoy reading the blog entries and definitely wish you were accepting patients!
I tested positive for thyroid antibodies 1 year ago yet the thyroid levels were normal. I also had HIGH testosterone (go figure?) Fast forward a year later, my TSH was 5.12. Then I eliminated gluten, soy , and corn from my diet and a month later my TSH was at 1.2 Now, I basically am at a crossroad, to continue gluten free or to even go grain free. I have reduced dairy but not eliminated it. I have a question regarding the supplements you recommended. How much k2 should one take to off set the Vitamin D? Also, do you think it’s necessary to take Magnesium when taking Vitamin D? I noticed I was getting anxiety and insomnia and so I added more Magnesium and it seems to have gone away. I’m not sure if that was from the antibodies or the lack of magnesium from taking vitamin D. Also, for selenium I read about all these possible side effects from it. Is there a blood test to show if you really need it or to stop taking it? The one I found has 200mcg… should I take it every other day to start?
Hey Tania,
It sounds like you might benefit from some guidance either through a nutritional coach or provider who can help guide you further. They will be able to answer all of these questions and guide you further because the answers to your questions are highly variable.
Hi Dr. Where can I meet you ?? Where do you live and what’s your clinic address I need to meet you urgently.
Hi Halima,
Unfortunately, I am not accepting new patients! Sorry about that.
Dr. Childs,
First, THANK YOU for writing such an informative post!! Like many, I am trying to come to some understanding of my lab results and if my Graves’ Disease is truly in remission or not. I live in Ontario, Canada and I have since left my endocrinologist who sees me only once a year and only performs the TSH blood test. I had a very severe case of Graves five years ago with nodules found as well–I have been in remission for two years by way of my TSH lab work and am not on Tapazol. With that being said, we know our bodies well enough to know when something is not right. I have asked both my GP and my endocrinologist for thyroid tests to see where I am at the five year mark. My endocrine said no to everything but the TSH and my GP has really no understanding of why I am asking for what I am asking. My GP did go ahead with the blood work: : TSH: .80 mIIU/L, Free T4: 10.7 pmol/L, Free T3: 4.4 pmol/L, Thyroglobulin Antibody: <10 kIU/L and Thyroperoxidase Antibody 90 kIU/L.
What does it mean to have Thyroperoxidase antibodies? Does it mean I am coming out of remission?
These are the only tests I have been given. Are there others that should be performed?
My endocrine said that none of these tests should have been performed including the ultrasound for my nodules. I have had issues with severe bloating and am running out of food to eat –I have taken out gluten and corn, dairy, and sugar as this all leads to issues with my stomach and inflammation in my body. Both the endocrine and GP say that food and chemicals have nothing to do with my auto immune and that there is nothing I can do in order to protect myself or be proactive in my health. I'm at a loss as everything I read these days has to do with food and endocrine receptors and micro biome. Any help regarding my lab work and pointing me in the right direction would be greatly appreciated. Thank YOU again for writing this blog post. We all need to be our own advocates but a little support such as your blog posting means a lot for all of us who are trying to find some answers. Cheers.
Hey Jennifer,
Ordering the right tests is useless if your physician isn’t willing to act on them.
That is exactly right. Can be very frustrating. We will just stand up, advocate for ourselves, take our health back and follow our gut instinct by listening to our bodies. Which is probably telling us to clean out our gut lol. We will be a plastic free home from now on, after reading up on endocrine disruptors this week. All thanks to Dr. Childs for his amazing work. Praying for us.
Yendi
Do you know of any Doctors in Dallas Tx?
Hi Roxanne,
Unfortunately I do not know anyone in that area.
Hello,
I live in the Greater Toronto Area in Ontario, Canada. I have elevated levels of antibodies and normal TSH (with some symptoms of hypothyroidism). My endocrinologist says he does not treat high antibodies, only abnormal TSH. After reading your very informative article, I was wondering if you know of any doctors in the GTA (Toronto, Mississauga, Brampton) that are willing to proceed with treatment when anti TPO levels are high but TSH is within normal range?
Thank you,
Ivana
Hi Ivana,
Sorry I don’t know anyone in that area, physicians who practice this way are quite rare and I don’t have a list of them.
I have lost 20lbs in the past 1 1/2 months and 10″ total through out my body thanks to you.
Thank you for saving my life since finding your blog just 7wks ago!
As an active duty military spouse, I am the main care giver to our 3 beautiful children who are 5 years old and under. I really need to be at the top of my game, which should not be this difficult at only 32 years of age. Our baby is only 7 months and nursing, thus so important to protect her and what she is getting from my body to not hurt her system.
Long story short, long list of symptoms I will spare you from as well, but I must tell you that I have been DEVOURING your blog. Post after post, page after page of notes, overwhelmed by sometimes tears or sadness, frustration, fear but also relief. That somebody gets it and is a decent enough human being to take such time and care, in providing us all that are starving for help, with much needed and rarely found information. I no longer felt so alone upon reading the comments from others and even found myself praying for them as I start to see way worse off and longer enduring situations.
Found your blog the week of April 17th and on Sunday, April 23rd I started the AIP diet. I am still on AIP though I do add some dairy in greek yo form and little cheese and also eggs ok. Gluten was/is my kryptonite.
In the first 8 days I lost the first 10lbs!!! All that swelling and inflammation.
20lbs total in only 7 wks and 10″ through out my entire body.
Had my Doc order your complete Thy panel. Verified the results with your optimal Ref Range levels. Did the Rt3 ratio as well. Got my meds switched to Tirosint for t4 at 125 (now 100) and for t3 Cytomel though only at 5. (Thats all she will do) I would rather have NDT but with gut issues that I am still (and are) healing (leaky gut, yeast/candida) not doing that yet until flora adjusted. Super low Vit D, 600 TPO yikes, adrenal fatigue, I am sure my poor liver needs support too.
Well as you can imagine my body continues to amaze me and healing now thanks to you and the supplements you also recommend. Though I think my biggest scare right now is making sure I am not taking anything that is going to harm my baby who nurses still all day long. For example, I am testosterone low. Hello estrogen dominance… no surprise there I am sure. So would like to use progesterone cream and saw palmetto but of course the research for taking palmetto while nursing a precious infant just dont exist lol for obvious reasons. So sometimes really overwhelming moving forward alone but at least I have gotten somewhere. Would love to take iodine drops but read not good call with a nursing babe. Love selenium though doing that. Getting Vit D3/K2 tmrw, hoping for a liquid form for my tongue.
Seeing a wellness holistic super well educated doc to clean out my gut with some standard process supps.
As you can imagine I will spare you the many symptoms but of course adrenal fatigue, low Vit D, 600 TPO yikes. Most likely estrogen dominant and testosterone low.
Anyway seriously sorry for all the info. You must get soooo many people trying to get a second of your time. Bless you heart. I hope these humble and probably very poorly written words (I am tired- also not a suprise) will encourage somebody and most importantly just want to say Thank You. Two very small words that do not do justice to all you do.
Extremely grateful, singing your praise wherever I go.
Yendi Parker
Hi Yendi,
Thanks for the kind words, I’m glad you’ve found it helpful.
Thank you for the information. I am going to try your recommendations.
Hi Tina,
You’re welcome, I hope you find it helpful. Keep us updated on your progress.
I have just been diagnosed with Graves Disease, but I don’t know if that is correct. Here is what I know of my test results:
T3 is 185
T4 is 2.0
TSH less than 0.01
TPO AB 318
I am about 15 lbs overweight, i have trouble losing weight, I have a slight tremor in my hands, trouble sleeping, itchy eyes. I exercise daily be walking, lifting weights and basic workout. I am a vegetarian, I love chocolate, I drink a few glasses of wine a week. Also I am a 62 year old female with one kidney as I was a living donor. I appreciate your input. Respectfully, Stella
Hi Stella,
The treatment for Graves’ is different than what I’ve outlined here. If you undergo radioactive iodine ablation or a thyroidectomy then some of this information would apply.
Hi Dr. Childs,
First, thank you so very much for your blog. It’s an incredible wealth of info and has given me so much hope. I found I have elevated antibodies (86 when 59 is norm and 11 when 4 is norm) in May and have been on AIP diet for 7 weeks. I am adding in the supplements you suggested.
How long does it take for the average case of low antibodies like mine to see improvement? I have read it takes 6 months to heal the gut and another 6 months to lower antibodies?
Also, do you ever see tendonitis as a part of Hashimoto’s? Mine improved a ton on AIP but is flaring right now.
Hi Win,
If you are on the right track then usually antibodies will drop within a few months.
And yes, I do see tendonitis with Hashimoto’s quite frequently.
Hi! I’m pretty confused about my lab results, everything is normal except my TPO which is 9 … i have lots of symptoms of thyroid issues, anxiety, difficulty sleeping, fatigue, and hair loss.. I also have tested positive for gluten and dairy intolerances. I am working with a naturally oriented practitioner who isn’t into sharing diagnosis I guess, but she put me on an immune boosting regiment to help. I just want to know, is it likely an autoimmune disorder?
Hi Julie,
Depending on the reference range for your TPO antibodies you most likely have autoimmune thyroiditis.
I really need to figure how to explain this to my doctors. I found one good doctor in North Carolina who told me I have autoimmune thyroid disease, meaning I have anti TPO antibodies and other concerns (along with typically being low on VIT D.) Even with supplements at times I would have to take 10,000IU for a few months. Anyways, Since I have moved to various states, all of these other docs just tell me I am fine, I have panic disorder. I have anxiety/OCD that has NEVER been to the heights that they are now and these doctors won’t listen that it is my physical health. My latest reading of the anti TPO antibodies alone were “11”. Thyroglobulin Antibody says “<1.0 IU/mL ” out of 0.0-0.9 (So what does this “<1.0″ mean?”
I have been having every symptoms from extremely worsening anxiety/OCD, advancing vitiligo, weight loss, amenorrhea, it hurts to the bone to be cold, can’t eat food comfortably without digestive enzymes but sometimes my appetite is ravaging. My emotions swing however they want. I’m at my whits end here.
Hi Bri,
It’s well documented that patients with elevated antibodies but “normal” thyroid studies still experience many symptoms of hypothyroidism and tend to improve on thyroid hormone replacement.
I Doc. Great explanation. I’ve more than 13000 A-TPO, a record, and whould be great to talk with you but…why don’t you have a waiting list at this time? You don’t give medical consultations?
Hi Marath,
I have a full patient load currently and we stopped accepting patients on the waiting list when it became apparent that it would be 6+ months until I had openings. It didn’t feel right for me to ask patients to wait that amount of time when they are suffering.
Dear doctor, I understand. Not wanting to abuse your goodwill, three questions: I like to run and with Hashimoto I feel worse and worse, I use hydrolyzed whey without gluten and lactose before running, I do good or bad to run and take protein? I have been using Levothyroxine for 2 years now, should I try to switch to Armor? And the question of 1 million dollars, have you ever met someone who had A-TPO above 1000 or 10,000 and who actually managed to return to normal values and stop the thyroid attack? Best regards and thanks for you work.
Hi thank you for your sharing
I have a better view of my condition now.
I got some question to ask is stress/anxiety a factor to cause TPO level to be high?
Or is it TPO high that is why it cause stress/anxiety?
Does it mean that if my TPO and T4 level back to normal
I will be more energetic and also able to handle stress/anxiety better?
Lastly how can TPO
affect the our eyes?
Medication for TPO, hyperthyroidism(carbimazole) and hypertension( propranolol). Will these medication or just the thyroid disorder itself have any side effect if my wife and I want to have a baby?
Side effect I mean our fertility chance and the health of our baby.
Hi Dr.
I have enjoyed your articles! I believe I have had an issue with my thyroid for years. I have gone to my PCP numerous times with concerns. I have a stable for 2 years multinodular goiter with small nodules on both sides, I have had most of the symptoms including a real significant weight gain almost 38 lbs which has happened in tbe last 6 months or so, i eat good and exercise. I went to an Endocrinologist last year my TSH was low and my antibodies were negative. I just had blood work done 2 weeks ago my TSH was .485 and my T4 was 1.08 PCP said it wasn’t necessary to test antibodies. I go see her in a few weeks. I developed carpal tunnel in last October and had both surgeries done 1 on 5/25/17, 1 on 6/22/17. I have at least 10 or more of the symptoms. I just don’t where to go from here so I would appreciate some advice! I am 39 year by the way! Thank you!
Hi Marcey,
You should look beyond thyroid studies and into other hormones such as estrogen, leptin, insulin, testosterone, insulin, etc.
Dr.Childs,
Thank you for responding to my question. I have an appointment with an Endocrinologist on Oct.11th and will discuss things with him. I will contact my PCP and get those tests done that you recommended. I know it may be hormonal but is it also possible it is my thyroid?
Hello, I am 22 years old and my tsh=8.8 and anti- TPO= 65,3..are these results very bad? What can you told me about my prognose? Thanks a lot!
Hi Natia,
Depending on your symptoms it is very likely that you have some degree of thyroid dysfunction (based on labs alone).
Hello,
Great article!!! Here are my lab. results. Could you please advise?
TSH – 1.00 mU/L (0.34-5.60)
FT4 – 10.56 pmol/l (7.47-21.11)
anti-tpo – 290 IU/ml (less than 9 IU/ml)
anti-tg -2.1 (< 2.2-4.9)
Thank you so much in advance!
Hi Rosey,
Those labs are incomplete, so there isn’t much to say just looking at those. I would recommend that you get a complete thyroid lab panel so you have a better idea what is going on.
Is my thyroid working normally in your opinion? Are the antibodies worrisome?
I would highly appreciate any comment from your side…Whatever you can understand from my lab.results.
Thank you
Hello. Just to clarify, my TPO came back 13, TSH 2.87. Does this indicate my thyroid isn’t functioning well? Lots of symptoms 🙁 Thanks for the info.
Hi Shannon,
You can’t really make that assertion based on 1 set of labs. It’s certainly possible, however.
Hi Dr.Childs,
I went to my Dr for a referral and she wanted to do a wellness check up and decided to check my thyroid and antibodies. My TPO came back at 900. I was wondering if it takes a long time (years) for an antibody count to get that high or if it’s something that can happen relatively quickly?
Thank you!
Hi Stephanie,
Your antibodies can shoot up that high relatively quickly, so the number really doesn’t give you a measure of how long they have been present.
Hi,
I am a 48 yr old female with a high TSH, my grandmother had her thyroid removed due to growths on it. Thinking I could have a genetic predisposition, I asked my doctor to have me tested for Hashimoto.
I just got my TPO ab results back and it was, 590.6.
On a scale from 1 to 10, how worried should I be?
I have an ultrasound today and my worry level is about a 12.
Thank you!
Hi again,
I got a call from my doc who said my TPO was normal range for someone who has a family history of thyroid disorders. What on earth does that even mean?
Thanks so much.
Hi Dr. Childs,
Everything I’ve read here has really resonated with me, and it’s so nice to have somewhere to turn. Last year at Xmas I was feeling terrible, the doctors finally sent me for thyroid testing in May.. Where they discover a multinodular goitre, and hashimotos 🙁 I’m only 33 and am still breastfeeding my son… All my levels are “normal” except TPO- I’ve lost over half of my hair, and am at a complete loss. My endocrinologist and family doctor both believe in the wait and see approach… Any recommendations for quality endos in Calgary Alberta Canada ??? Thanks for this post, it’s life changing
Hi Holly,
Unfortunately I don’t know anyone in the area!
Very interesting information. I have been complaining for years that there was something wrong and finally found a doctor who listened and ran the TPO Antibody test with my semiannual TSH tests. Well, the TPO came back at 866, the TSH was so low it didn’t even register. I asked him to run this after learning about the difference hypothyroid diagnoses and Hashimoto’s would certainly answer many question. He still says the treatment is exactly the same but I have to know the latest truths. I have been fighting for more than 20 years and I’m not ready to give up yet. Medicare doesn’t cover a lot anymore but what you have here is definitely a good start.
does being a dental assistant has anything to do wih this disease ? using xrays for over 18 year?
Hi Alex,
There may be some connection between the two, you can read more here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2935336/
Thank you for writing this. It was very helpful! I was recently diagnosed with hypothyroidism and my anti TPO antibodies were at 4 in my last two blood tests. Would you consider that to mean I also have Hashimoto’s even though I’m technically in the reference range (0-9)?
Thank you so much Dr. Childs.. my thyroid hormones are normal but my anti TPO level are so high, with low vitamin D and vitamin B12. Reading this now i know what to do.. thnk you again
Hello,
I was diagnosed with Hashimoto’s in 2009 and take Levothyroxine. I have been experiencing all the symptoms: gained 25 pounds in the last year, fatigue, brain fog, and mood changes. I also have rheumatoid arthritis and type one diabetes for which I take Enbrel and insulin… I recently moved to Florida and asked endocrinologist to test TPO antibodies but he refused saying they will always be present since I have already been diagnosed with Hashimoto’s. My understanding is that when my T4 and TSH is “in range” but I’m still highly symptomatic it would be helpful to see just HOW high the antibodies are as increasing medication could help reduce antibody levels (I know they will always be present but could they not be reduced?) I would appreciate any feedback!
Thank You,
Carole Pritchard
I’ve been suffering with hypo symptoms for over 10 years. Blood work always comes back “normal range”.
*My TSH is 2.66 so high according to your optimal levels
Free T3 is 3.1 so in the upper 50%
*Free T4 is 1 so low according to your optimal levels
*RT3 is 15.8 so midrange not low
*Anti TPO is 28 so higher than it should be
*Thyroglobulin antibodies are 15 so higher than it should be
BUT reading the part about hormones you said: “What is interesting from my point of view is that almost every patient I treat who has high thyroid peroxidase antibodies also has a corresponding low testosterone level.”
Mine are high… so what does that mean?
Total testosterone: 42 (range 10-76) midrange
SHBG: 18 (range 18-166)border low
*Free testosterone: 1 (range .04-.53) high
*Bioavailable testosterone: 24.8 (range 1.2-15) high
DHEA (serum): 5.45 (range 1.3-9.8) midrange
My estradiol is on the lower side, prolactin on the higher. So what does that mean?
First – great article at explaining antibodies.
My levels
Thyrogloubin Antibody 19.400 Iu/ml 0.00-115.00
Thyroid peroxidise antibodies 43.6 Iu/ml 0.00-34.00
Thyroid Stimulating Hormones 3.32 miu/L 0.27 – 4.20
Free Thyroxine 16.6 Pmol/l 12.00-22.00
Total Thyroxine 106.5 Nmo/l 59.00-154.00
Free T3 4.69 Pmol/l 3.10-6.80
Reverse T3 16 Ng/dl 10.00-24.00
Reverse T3 ratio 19.08 15.01-75.00
Hair loss for 21 months at this stage. those results are from month 18, that was the first time I had more than the tsh and t4 tested.
When all my troubles started, I had stress for a month which was bad. But it was immediately followed by what I thought at the time and still do not know if it was or not a ‘flu’
it affected my throat, not my nose and not my chest. I caught it in Dublin in early February 16. (at that time there were several deaths from swine flu in Dublin) a child I was in the company of had what we believe was ‘a flu’ I got it from them.
I couldn’t swallow anything at all so for a week I was bed ridden, could eat nothing could barely swallow water with the pain. Lost the stone rapidly. Was like an anorexic by the end of the week.
Couldn’t eat properly because of the throat and loss of appetite for a couple of weeks. took about 2 months to put the weight back on and get appetite back.
I didn’t go near the dr, (never did before this) just rested at home and let it run its course.
I have since over the past 2 years discovered I have a struggling tsh and raised antibodies heading towards hashimitos as a GP told me yesterday. I also discovered h pylori infection (6 weeks ago) stomach pain over the past 2 years along with hair loss. I reckon the stress and loss of weight lowered my stomach acid enough to let it run wild. Prob had the h pylori infection for years and years but was kept under control by my stomach acid.
My question is could that bug or whatever it was have been the trigger? Could I have initially had sub acute thyroiditis? I didn’t get tested until 5 months after the flu when hair loss was noticed. and my tsh and t4 level was
Test Date 03 June 2016
Serum free T4 level 19.4 Pmol/l 12.0-22.0
Serum TSH level 3.18 mU/l 0.3-4.5
Are antibodies present in sub acute thyroiditis at the level mine is currently at?
I get retested in 4 weeks to see if they have decreased with the eradication treatment which was successful.
recently I feel pain in my left and right kidney area. going to ask for tests to be done on it to see if there is an infection. Had a scan done on them 6 weeks ago and they said that I had no kidney stones, but there was white blood cells in urine and red blood cells. (could the red blood cells (which you couldn’t see) have been from my period? It had started that day. But was wearing a tampon.
is there any chance my results could be sub acute thyroiditis with raised antibodies due to the gut infection which was never dealt with?
Hair loss is the biggest issue still ongoing, finer disappearing from everywhere. Will it grow back if I get treatment? also lighter, shorter periods, lack of sweating and numerous other more minor ailments, but consistent with thyroid problems.
Questions
My question is could that bug or whatever it was have been the trigger? Could I have initially had sub acute thyroiditis?
will hair grow back?
what treatment do I need?
do you think the antibodies at the range they are at will likely go lower with the h pylori removal?
ior am I Hashimotos and that is it?
Please respond, I need a knowledgeable person’s (dr) feedback, all endos, gps, derms I have seen (9 in total) all said thyroid not a problem. I know something is wrong. I have no options left.
Ferritin is 50
awaiting vitamin d results today
B12 is 699 active b12 is 68
getting a range of other nutritional tests done by a doctor who has already told me there is nothing wrong next week.
please help/advice
My 16 year old daughter was just diagnosed with a thyroid antibody level of 283. The blood work was done by an obgyn that we saw due to very painful, irregular periods. The symptoms during her period include low grade fever, extremely painful cramps, nausea, extreme fatigue (sleeping 15 – 16 hours a day) and general body aches. I’m in the process of making an appointment with an endocrinologist and researching this at the same time. I just got the lab results this morning.
So far I haven’t come across anything that describes the symptoms as only being during a woman’s period. Is there a significance to this and are there any special tests I should ask for?
Thanks for your article. Since my diagnosis in late Sept 2017 I have struggled to understand what this means. I have high thyroid antibodies with a functioning thyroid. You laid out my symptoms exactly which in itself was validating. My endo and GP wanted to put me on anti depressants and wait and see. Instead I found a Functional Medicine practitioner and have been working with her. Went a on 10 day cellular cleanse, then a 21 day replenishment cleanse. Symptoms did not go away. She then put me on HRT and LND. I have a bit of a problem getting used to the LDN. The dosage is 1.5, I had to stop after the first few days because the symptoms came back with a rage. Then started again and felt much better. Unfortunately I had 4 days where I didn’t have the drug and have to start again and it’s rough going. The Pharmacist said to give it a week. I was able to get my GP interested enough to do some homework and she suggested an every other day dose. I just wondered if you could expanded on dodges. I am petite. I am following a the paleo, wheat, corn, soy , sugar and dairy free. But I do need some carbs so I eat gluten free oats. How long does it take to start feeling well?
Hi Dr. Childs Thanks so much for your CONCISE AND CLEAR article. This was very eye opening! I have been diagnosed with Hashimotos but am not in treatment other than lifestyle modifications. In your example of the patient that had “normal” but in reality suboptimal levels, was there an error in your explanation? I noticed you highlighted Free T3 and Reverse T3 but you talk about her Free T4 being low and her Reverse T3 being high. Did you mean her Free T3 was low? Can you give examples of where all these ranges SHOULD be for clarification? I don’t understand “Optimal levels Should be in the upper 50% of the reference range provided by the lab” Thanks!!
Hi Dr Childs I am very grateful for the extensive information you so generously provide. After years of struggling with an endocrinologist who “new best” I trusted my research and have been actively making the necessary changes and getting results. My Peroxidase Ab are 18 Tg Ab <20. Last blood test we measured Anti -Tg 2.8 andAnti – TPO *11.7. I suspect this is due to gluten products creeping back into my diet and for 2018 I will finally ditch the dairy. Hoping to start losing the extra kilos (15) by careful reduction of carbs. I found my T3 levels were affected when I tried ketogenic diet.
I am now on natural thyroid and it has helped.
Hi,
I had the Avise tests in February 2016 and I’m confused by the results: <244 anti thyroglobulin IU/mL and <33.4 perodoxidase
That seems high but their reference ranges are Negative at <280 and <60 respectively. Although it seems they’ve changed those ranges now on sample tests on website. I don’t get the “less than” symbol is it different than a solid # or does it simply mean 243.1-243.9 somewhere. Ranges I’ve read elsewhere are nowhere close to that high. I’ve been telling docs it’s not normal to feel how I feel everyday for decades. I have severe symptoms at this stage along disabilities due to sleep apnea, DDD since teens, Ray aids, PVCs, and much more. C-RP tests etc prove inflammation but all test “within normal limits” or “ not severely elevated/reduced enough” to get an answer. What do think of these test result #s??? Thanks so much for any advice!
Hi Christina,
I’m not familiar with Avise tests so I can’t really give you an opinion on how accurate they are. The less than signs are there to simply indicate that anything higher is considered abnormal while anything lower is optimal, labs often use this over the traditional reference ranges for antibody tests.
I was diagnosed with hypothyroidism following my pregnancy 30 yrs ago but never tested for antibodies. Was treated for 26 yrs with Levothyroxine only. Switched to 90 Armour Thyroid 4 yrs ago. Now have very low TSH, elevated T3 (5.5) and rT3 (15). TPOab=41 with negative Thyroglobulin antibodies. I have made some diet changes and am supplementing with Vit D, A, K2, Progesterone, vit E and milk thistle but am still unable to maintain a consistently normal body temp.
I am confused by the antibody results….. Do I have hashimotos and is it possible to lower the antibodies further?
Hi Angie,
Each lab has a different range which is considered “normal”, if the result for TPOAb was flagged as high and you have symptoms of hypothyroidism (for instance being on thyroid medication) then there is a high chance you may have Hashimoto’s. It may be possible to lower your antibodies further through various treatments but you wouldn’t know until you tried.
My 13 year old daughter had a TSH of 7.5 in February 2017 TSH of 9.7 2 11/30/17 and on 12/15/17 her TSH went done to 3.34 but her Thyroid Peroxidas Antibodies are 82 flagged as H and her thyroglobulin AB is 29.9 flagged as High. Her resting heart rate has been 108 for the past six months but has dropped this week as well to 79. Dr say thyroid is enlarged. With the new test results he said not treatment lets re-test in 3 months. My understanding is this is the exact wait and see approach you are referring to and that an autoimmune is present in her blood results. I’m not comfortable with not addressing the autoimmune at all. Thank you for the information. Any feedback would be soooo appreciated.
Maxey
Hi Maxey,
It would be worth evaluating this blog post for more information on what steps you can take to try and lower her antibody levels. You can read more about that here: https://www.restartmed.com/tpo-antibodies/
Hello,
my name is farah, I’m 23 years old female
my TSH level is 5.795 and the ref range is ( 0.55-4.78 )
my (Anti TG) Abs level is 94.8 IU/ml and my Ab (Anti TPO) level is 89.9 IU/ml.
my Dr. has described to me Euthyrox 50 one tablet for 2 months and then make the FT3 AND FT4 AND TSH tests again.
Do you recommend me to do a diet and take supplements to help with the Euthyrox ?
if so please state the supplements you do recommend.
note that my FT3 AND FT4 levels are normal.
thank you in advance
Hi Dr Child’s, I just had blood work done after feeling sick for months to a year. Thyroid issues run in my family, and my mother took synthroid for years before passing from another auto immune disease. I have had painful Gi issues all year, my head is cloudy and forgetful, even moments of slurring, balance issues, lightheaded, EXCESSIVE sweating and thirst, severe anxiety, trouble sleeping, thinning hair, irritability. I have terrible joint, digestive, and muscle pain even though I take 300mg of tramadol xr daily. It is very very uncomfortable lying down every night… I wake up all night covered in sweat to the point my clothing is wet. I literally become slick to the touch all over and it disgusts my boyfriend because the sheets are soaked in my sweat every night. I have a low basal body temperature.
My tpo ab results are 118 ref intv 0-34
Thyroglobulin ab 39.6 ref intv 0-.9
T4 free direct .94 ref intv .82-1.77
TSH 1.68 ref intv .45-4.5
Vit D 25-hydroxy 33.8 ref intv 30-100
Lipase serum 14 ref intv 14-72
Negative celiacs
My Dr says these results “look fine” , and I am really uncomfortable with her answer and no clinical explanation. I am exhausted by these issues effecting my quality of life .. especially in my youth as a mother. Your article is the best thing I have found … please, what is your recommendation? I just want to get better, and live a happy life. Thank you so much Dr. Childs.
I am 34 years old, and
My TPO and TG antibodies declined from triple digits to single digits when I changed my diet to paleo/AI paleo and lost almost 30 pounds; I eat mostly grass fed meats and organic produce as available. At the same time, my liver enzymes, triglycerides and glucose levels normalized. Cholesterol decreased but is still a bit high. My changes seemed to have had positive results in a short period of time, about five months, but I am curious about this: Do the antibodies also decline when your thyroid becomes excessively damaged and dysfunctional, unrelated to other factors or causes? Great article.
Hi Leah,
Yes, thyroid antibodies may fall in late stage Hashimoto’s after significant thyroid glandular damage has occurred.
Hello, I have 0.03 TSH and 43 ANTI TPO. My brothers used to suffer from Hashimoto’s, developed nodular gland and had is thyroid removed. My other brother had hid Thyroid removed as well because of follicular cancer. What could my test results indicate?
Question? Can i reverse these high antibodies. My TPO was 52 in a range from 0-32. My thyroglobulin antibodies were 5.8 in range of 0.0-0.9…reverse t3 was 21 and both t3 and t4 was top normal. TSH was 2.9 and last text was 1.2 …testosterone total was low and free was bottom normal. Sometime it’s low. One time i was prescribed HCG and the day after i could feel it hitting a sweet spot. For once i could Keep my head up and could lift weights strong. But i started to get anxiety. I have always suffered from anxiety and depression. But not this bad. And i was a personal trainer. So after i train i feel sick and flu like for a few days after. I’ve have cortisol serum levels and they came back normal. Saliva were always low normal. I know It’s a lot to read. But i want to have my old life back. I’m only 36 and have spent most of my days laying down now. I did experience high stress before these symptoms all got worse. Would testosterone treatment help? Both at quality of life and reversing autoimmune thyroiditis? I tried 100mgs a time before for low t(via dr) but it causes bad anxiety and i didnt Even want to leave the house. Another Dr said that was too high and should start lower and build up. 20mg 3 times a week to start out. I have Low normal SHBG. They also said NDT with it. But i didnt Like how i felt On it. Plus my thyroid is still functioning. An help to start would be awesome! I know You can’t do too much medical advise. But at least point me in the right direction. Thanks
My thyroglobulin antibodies came back high at 299 iu/ml. Ive been telling Drs. for years somethings not right. They never tested this before. Now what? I have horrible IBS, depression and fatigue. ive been taking levothyroxine for years. Ultrasound diagnosed thyroiditis. I dont know what plan to follow. Please help.
Thank you
Hello, I have been on thyroid meds for 4 years. Doctor let me switch to natural thyroid meds a year ago. A few symptoms have improved such as the extreme joint pain and constipation since that switch. I believe the little bit of T3 in the dessicated pig thyroid is responsible for the improvement. I take 90 mcg or 3 pills a day. TSH is mid range. Free T4 is at the lowest of the normal range and free T3 is mid range. Those labs appear normal even though I’d like to see the free T4 higher. My thyroid antibodies, both thyroglobulin and thyroperidase are high (382 thyroglobulin when <40 is normal and 202 thyroperidase when <35 is normal). I eat very close to paleo and exercise 4 to 5 times a week, weight lifting and HIIT/tabata style bootcamps. Should I be pushing for a) further testing b) more meds. I am 15 ibs over weight despite my healthy active lifestyle and I just don't feel healthy (extra weight is all on my mid section and upper body, hair still falling out, trouble sleeping). Shouldn't the medication have lowered the antibodies? If I still have symptoms does it mean I'm not "optimal"?
Hello, if thyroid antibodies (thyroglobulin and thyroperidase) are really high even though TSH, free T4 and free T3 are in the normal range, does this mean a) I need higher /different meds b) I need more tests? I’ve been on meds for 4 years. (Levo for 3 years and now desiccated pig thyroid for 1 year). I feel a bit better in natural meds but I still have symptoms such as inability to lose weight, hair loss and joint pain even though I live a really healthy and active lifestyle. I eat basically grain and sugar free and no processed food. Exercise 4 to 5 times a week. Shouldn’t meds have lowered the antibodies? I don’t feel healthy despite my efforts and meds. Shouldn’t I feel better on meds? It’s seems like a silly question I know. Should I go back on Levo and request T3? I feel like I’m on the thyroid roller coaster in hell and I always end back at the beginning feeling how I felt 4 years ago!
Hello! My mother and sister have HT. my TSH is 1.23 and my anti-TPO is 39, plus i have a goiter and am symptomatic (weight gain, hair loss, fatigue). Is it completely out of the question to start Levothyroxine?
My TSH level was in 2000 9,41, ATP 94. In 2008 TSH normal, in 2018 january 9,351 and in march 2018 7,662 (after a diet without gluten/diary,sugar). But antibodies ATP 1098. (antithyroglobine 77) All those years I didn’t have any symptoms of hypothyroïdie.And still now I don’t have any symptoms. Should I have an autoimmune problem?and should I have it treated? no other problems ,no ilnesses and no problems with bloodtests otherwise. Thanks you, Peter
I have been battling idiopathic chronic urticaria for 4 years. One MD tested thyroid antibodies and tpo/antithyroid globulin was 100 times the normal. Thyroid function was normal yet, I am covered with urticaria. Please guide.
Hello. My TSH, t4, and t3 are all in the normal range with the being .76. My peroxidase antibodies are 19. Would you recommend thyroid meds?
I had my thyroid checked at the end of last year, my TPO is over 600.
I have been taking Adderall for about 3 years. Out of nowhere, my fingertips started peeling & when I got my hands wet, they (fingertips) looked like id been swimming for hours….completely waterlogged. One dr. said Raynauds, a dermatologist gave me clobetasone (sp?).
But previous to all this I had a genetic test was done that said I have MTHFR mutation!
Now my fingertips are dry & crusty and they tingle.
WTH?! I give up
Dr. Childs,
My TPO level is at 60. I had a nuclear uptake test and it was normal (no uptake was seen). I have pretty bad symptoms of muscle aches, joint pain, stiffness and cold intolerance. I was told by my endocrinologist that just test it every year. This does not help my discomfort. What do you recommend for these symptoms?
Hi, thanks for an awesome article. I really appreciate the clear information. You asked for our results so here they are in() are the “ranges” -:
Thyroid
TSH 5 mU/L (0.4-4)
Anti-thyroglobulin ab 440 U/ml (<60)
Anti-thyroid peroxidase ab 5600 U/ml (<60)
T4 14 pmol/L (10-20)
T3 4.3 pmol/L (2.8-6)
As you can see my t3 & t4 is within "optimum" range and my general health is good. But my autoimmune indicators are way off the charts. 440 and 5600 respectively (recommended <60). I'm just under 50 years old, male, and live a reasonably active life. I travel for charity (community empowerment) in remote regional areas usually tropical and have picked up many of the mosquito viruses and other things which have probably stressed my immune system. Also, a period of extreme deficient diet in remote Africa about 10 years ago which put my metabolism into a starvation mode and took 12 months to recover from. So I can appreciate some of those physical and other emotional stresses may have been a trigger. I do have some aches and pains And possible arthritis possibly From the viruses (including but not limited to… Ross River, dengue, Balma forest, chikungunya, unspecified mysterious Amazonian ones as revealed by DNA virus signature testing when they tried to work out which dengue I had had)… But looking at the results and given a test I had 5 years ago (only for TSH which was 4.5 at that time) indicates an ongoing autoimmune issue yet still functioning thyroid… Is it fair to say I need to really do something to correct the autoimmune issues? My diet is generally pretty good. Mostly whole unprocessed food. Mostly vegetarian fresh and homemade. Limited wheat. Some milk yogurt. Rice-based carbs mostly. Other Probiotics. So I can eliminate a few things but it won't be a drastic change in my diet. I will also look into getting those other tests you suggest to better evaluate the situation. Eg testosterone and gluten antibodies Etc. Is there anything else I should be looking at with such high TPOAB? Is this article still generally applicable for men and in particular when not really presenting the normal health issues of weight gain, excessive fatigue (over an above what one would expect from someone who has had all those fatigue related viruses) and other general symptoms? Thanks for your learned and informative advice.
Hi,
Age 43, stressful life, exhausted all the time…
Just got my results. T3 2.42, Free T4 1.20, TSH 3.05. Anti TG 336.1, Anti TPO 229.1. Based on your article the hormones are normal and it is most probably an autoimmune issue. As I understand it could be triggered by other affected organs in the body. What kind of tests would you recommend to see where the problems are. Is there a blood test that basically shows everything or that is impossible, or cost a fortune?
Kind regards,
Peter
Hello Dr. Childs,
I was recently diagnosed with anetoderma which can have an underlying systemic cause. After rounds of blood tests, the only abnormal tests were my TPO of 888.5 IU/ml and TSH of 1.72uIU/ml. My antiphospholipid panel were all on the higher end of normal ranges. I bounce between symptoms of hyper/hypothyroidism often. I am waiting for my first Endo appointment but wanted to see your thoughts on those levels. I also am a 32 y/o mid-level triathlete. Can my training be effecting my thyroid and symptoms?
Thank you in advance.
Dear Westin, Thank you very much for your post: I have to start saying that after a lot of reading found on the internet this is very well written and very helpful. I came across these thyroid issues very recently and started checking a lot of information. In my case I was diagnosed Hypothyroidism subclinical, I don’t have symptoms but my antibodies anti-TPO are over 1300UI. This is what is being worried me most, my T4 levels are still fine and TSH is around 7. I am really looking for something to drop down and hopefully remove my autoimmunity activity. I was considering already a supplement of Selenium/zinc and vitamins A, B, C and E. After reading your post I am absolutely convinced. As I moved to a country without a lot of sunlight, I had started already taking D vitamin.
Although I don’t experience really GI disturbance symptoms; I know very well the importance of the gut microbiota in immunity and inflammation and I’m willing also to start taking some probiotics. Would you recommend me any in particular?
Also, in your experience what are the chances to really drop the levels of the auto-antibodies?
Best regards
Hi,
Brilliant post, very informative.
My blood tests have shown normal thyroid function but GP says Antibody test should be 50 and it is 297.
I have a 2″ by 2″ nodule on left thyroid and a few small nodules on right.
He said we will just do yearly blood tests to check thyroid function.
It’s very frustrating trying to get him to take it more seriously.
This is a great post! My 9-year-old daughter has both antithyroglobulin antibodies and antithyroid peroxidase antibodies. Her TSH and free T4 are normal for now. Does the information in this article apply to someone of her age? Her PCP is doing the “wait and see” approach. She’ll have another blood draw in a few months to see if anything has changed, but I’d love to get her levels lower. Any advice would be great.
Hey, thank you for this informative post. I just had results back:
Anti TPO 2377.63
T3 1.06
T4 5.2
TSH 18.94
Should I be worried?
I used to have an overactive thyroid and had Graves disease a few years back. I stopped taking meds 2 years ago (personal reasons).
Thanks for the info! I’m a man, 30 years old.
My results:
TSH – 3.2031
free T4 – 13.53
free T3 – 3.97
anti-tpo – 749.03
The main symptoms are thirst, weakness, fatigue, small muscle pains, bags under eyes. In addition, I am concerned about vitiligo (10 years) and seborrheic dermatitis (1 year). I suspect that all this is related to autoimmune problems.
Your message has explained a lot. Thank you.
Hi Ant,
It is definitely possible that many of your symptoms may be attributed to autoimmune disease.
Hi I have had evidence of transient thyroiditis during pregnancy and even though my thyroid has become back to normal without any thyroid medication I still have a anti tpo positive at 447. I have had low vit d and been diagnosed with fibromyalgia and have evidence of mild connective tissue disease. Symptoms of lupus according to my specialist too. I do have a lot of symptoms and I am only 27 and struggle with a lot. Do you have any advice please thank you
Hi Sophie,
I would take a look at this article which may help you understand your situation a little bit better: https://www.restartmed.com/postpartum-thyroiditis/
The presence of thyroid antibodies may indicate that you have Hashimoto’s or that you haven’t quite recovered yet from your postpartum thyroiditis.
I just recently had a thyroid test done. Everything was ok except my TPO antibodies were 235. Does this mean I have Hashimoto’s? Dr wants to put me on a low dose of thyroid. Should I do this? All my other levels were good.
Hi Brenda,
You can have elevated antibodies and not have Hashimoto’s. It doesn’t seem like a good idea to use thyroid medication if you feel great and your lab tests are normal (at least that’s not how I would proceed). If you can identify inflammation in your thyroid gland through some other test then it’s likely you have Hashimoto’s, but you can’t really say that for sure at this point.
Hi Dr. Childs
I was wondering if you might be able to share any suggestions with me regarding my TPO level. Sorry for the lenghty message, i am really worried, and i am struggling to get any advice off my doctor.
I am a 32-year-old male, who was diagnosed with Hashimoto’s 6 weeks ago. Back then, my readings showed normal T3 and T4 levels, but a TSH level of 6.03. My TPO level was above 1300. Apart from the diagnosis, I am fit and play sport regularly.
I have prescribed 25 mg of levothyroxine daily. I have been following an AIP diet (finding very difficult)– cutting out dairy but having the odd cheat day a couple of times in the month (my wife loves chocolate). I have also been taking selenium and probiotics daily, with a 50,000 iu vitamin D3 tablet once every 2 weeks.
I had another series of tests 4 weeks after the first tests, and my results showed normal T3 and T4 levels, as well as an improvement in my TSH, which came back as 2.1. However, my TPO level was still above 1300. I also have a slight goiter appearing over where the left thyroid is located (between a pea and olive size). I have noticed some swollen painless lymph nodes under my jaw in the last couple of weeks that are still present (pea size).
I have also had an ultrasound which showed me having multi nodules on the goiter with spongiform echoplex on both thyroids, but apparently no signs of anything sinister.
I realize that only being on the levothyroxine for 6 weeks, and testing out these supplements and new diets might not be long enough yet to see a drop in my TPO level. I am just wondering what your opinion is on me being on such a low dosage of thyroxine, and how long would you normally expect it to take to see improvements in the TPO level? I requested a trial of LDN from my doctor (endocrinologist), but she was very dismissive of this, and wouldn’t prescribe it, which I was disappointed about.
I recently lost my mum to cancer and I think a lot of this may be down to the high-stress levels I have been under for the last 12 months.
I move to China in 2 weeks, and I know it will be very challenging to avoid soy and gluten, hence why I am wondering if being strictly gluten-free is strictly essential. I have just received my results back from the Imu Pro 300 allergy test I had, and dairy has flagged up as a major allergy, but not gluten or soy.
Any advice or opinion from you would be greatly appreciated.
Kind regards,
Matt
Hi Matt,
If you are on the right track, in terms of therapies, you should notice a drop in your antibodies usually within 6-8 weeks.
Hello Dr. Childs,
I’ve been suffering from many hypothyroidism symptoms for many years, my lab tests are within the normal ranges (but far from the optimal values).I’ve been prescribed 50 mcg of levothyroxine for the last year in order to improve these symptoms. The symptioms improved for about 3 months only when I first started the medication.
Recently, I had thyroid antibodies tested.
My anti TPO levels are normal (1.48 IU/ml, normal lab range <5.6), while Anti Thyroglobulin levels are high (100.82 IU/ml , normal lab range <4.11)
I was told that only anti TPO levels matter, and that high anti Thyroglobulin levels doesn't indicate any problem.
Do I need to have more tests?
Please advise.
Hi Imane,
You may benefit from looking at thyroid function tests (free T3, TSH, free T4, reverse T3 and so on) because that can help determine if you need thyroid hormone.
Thank you for this great article. Any advice on treating children with positive antibodies?
Hi recently had a blood test that revealed TPO >1000. A positive ana result 1.160 homogeneous and an anti-ds DNA of 8.0 possible SLE/connective tissue disease. I have many symptoms that seem related to my thyroid but also other symptoms that could mean something else. Any suggestions?
Hi Jennifer,
The first place to start is with a complete hormone and thyroid lab panel. You can learn more about which tests are required here: https://www.restartmed.com/thyroid-tests/
Have mild hypothyroid labs. The doctor immediately prescribed Synthroid, but I read the side effects and they mimic most of my symptoms. I don’t want to live what is left of life fat, bald, and miserable.
Hi Wendy,
I would recommend that you read this article which really explains how levothyroxine/Synthroid is supposed to work and how it may impact your symptoms (in a positive way): https://www.restartmed.com/levothyroxine-side-effects/
In the previous post, I neglected to mention I have celiac disease. So I feel Synthroid is a drastic step at this point and would like to consider other approaches. On GF diet, but recent travel may have introduced gluten into my system.
Hi Wendy,
In terms of natural therapy I would take a look at this article which should help you quite a bit: https://www.restartmed.com/hashimotos-diet/
So if I understand you correctly, the optimal number of antibodies is not necessarily in the reference ranges but as close to 0 as possible? Why?
Hi Barbara,
Antibodies are an indication that your body is producing something meant to attack and kill your own tissue. You generally want to have as few of these antibodies floating around in your body as possible.
My son just got his labs done. NOT on any meds. TSH 2.63, Free T4 1.7, Free T3 3.2, TPO 15 , Thyroglobulin Antibodies less than 20. I was diagnosed with Hashimotos in 2010 and so I have gone through the fun roller coaster. My son is 19 year old, very healthy but had mono when he was a junior in high school due to rigorous varsity football training. The doctor of course wants him to come in due to the TPO and Thyroglobulin , I would assume we caught this as Early detection of a auto immune thyroid issue? Any ideas and thoughts? I had him start taking Adrenal Complex and he is taking Standard Process Thyrotropin. He is also taking Protandim. I just had him go on a no grain/no gluten diet. He is is very lean in good shape . Any additional ideas?
Wonderful article. I suspect that I may have seronegative Hashimoto’s. All doctors I have seen are very conflicted about it, and each one says a different thing. Where may I have more good info about this type of Hashimoto’s and further tests or an explanation for why I might not have autoantibodies?
Also, does seronegative Hashimoto’s imply that there are no autoantibodies attacking and destroying the thyroid gland?? It would be amazing if you could shed some light, thank YOU!
Hi Anna,
You can diagnose autoimmune thyroiditis (of any type, even seronegative) with a thyroid biopsy and sometimes with a thyroid ultrasound. You most likely will not find anyone willing to biopsy your thyroid for this condition, though, because they don’t feel that the diagnosis will change treatment or management.
Dear Dr. Child,
In the last 4 years I was suffering from several symptoms of hypothyroidism. I always felt that something is wrong but my laboratory results were always negative for TSH – that is the only measure a standard analysis includes in Hungary (I also went to have thyroid US, but it was normal). In the last few weeks I red several articles about how difficult to diagnose this problem and analyzing free T3/T4 and anti-TPO also must be done to get the full picture. Finally I found that my anti TPO is 61.25 – this is not extremely high but still, not 0.
My question is if you have any connection in Hungary, do you know any Hungarian colleagues that you could recommend. Unfortunately, all doctors I saw in the last few years did not do anything.
Thank you
Best Regards,
Krisztina Gyurkó
Hi Krisztina,
Unfortunately, I do not know anyone in Hungary! I am sorry about that. It does sound like you are on the right track, though.
Hello doctor!
I’m writing you my lab results, hopefully you will have time to answer.
My endoc and my gynecologyst both have different opinion on my condition, an then here I am, reading across the net and forums, and having a third opinion..
My primary consern is whether I should start taking medications since I’m planning on getting pregnant and I’ve read that having this condition undiagnosed and untreated can be obstacle.
Two years ago I was diagnosed with subclinical hypothiroidism, my TSH and fT4 levels were border and my ATPO were normal. On ultrasound, the gland was isoechogenic, not homogeneous.
I went on checking my hormon levels for some time, meanwhile I was taking selenium supplement. After a year or so, I felt better and stoped everything.
Now, another year later, my symptoms came back, I started feeling like my gland was chocking me, my throath felt inflamed,I started feeling pressure in my left side from time to time(I haven’t experienced being awoken by high heart rate though, although it happend before) etc.
With my friend, I went on checkup that involved quantum medicine.
There I told I was deficient on vitamin A,D3, B1, B6, B12(low border), E, folic acid, Cinc, Selenium.
My iodine levels were in normal range.
According their parameters I had elevated thyreoglobulin and fT4.
After this I went and did propper lab testing. Meanwhile, I started taking everything mentioned above, as supplements(two months by far).
My results were following:
TSH 6.80 mIU/L 0.27-4.2
FT4 20.52 pmol/L 12-22
FT3 4.85 pmol/L 3.1-6.8
ATPO 39 IU/ml <34
ATG <20 IU/ml <40
What is your opinion on my diagnose, should I ask to be on medications?
Mr. Childs,
I just wanted to say that this is an incredible article.
TPO is the only elevated result that I’ve had. I have had symptoms which is what prompted me to get tested in the first place.
Results of other testing –
I have:
Low Vitamin D
Extremely low DHEA (I am only 28!)
Low minerals (zinc etc)
Possibly SIBO – getting tested soon.
I am working with a dietician who has given me the proper supplements and who will be testing me for SIBO as well. It is my hope that with diet change and continued supplements, I will see a stabilization or eventual decrease in my antibody levels.
Everyone, please get your DHEA and Vitamin D levels checked! Being on supplements for these for 4 months has completely eliminated some of my symptoms (such as brain fog).
Thanks
Lauren
Hi Lauren,
Glad you enjoyed it and thanks for sharing!
Hello Dr Childs.
Is it possible that numbers that are still within “normal” range (Tpo antibodies of 15 for example, tsh of 2.66, free t4 of 11) could be causing my recurrent miscarriages? I have 2 healthy small children and then all of a sudden have had three miscarriages (some as late as 13 weeks) back to back this year (still going through the most recent). I have some symptoms of hypo and it runs In my family but can’t seem to get doctors/OBs/midwives to listen to my concerns about thyroid possible being an issue as they say all “normal” range. Is it worth keeping pushing on this issue with them? To put this all more briefly, is there any good evidence that suboptimal thyroid levels can cause recurrent miscarriage?
Hi Amy,
Is it possible? Yes. Is it likely? Probably not. There is anecdotal evidence that pushing for higher numbers is ideal for certain women, but I’m not aware of any clinical studies showing this. You can find more information here:
https://www.restartmed.com/thyroid-and-pregnancy/
https://www.restartmed.com/tsh-levels-during-pregnancy/
Last April my primary care physician did a routine exam and blood work. My anti TPO-Ab was a 146 IU/mL. An ultrasound was ordered and results showed my thyroid was heterogenous and enlarged on the right side. I was referred to an endochonologist who said yes your levels are high and your thyroid is enlarged but see me in a year unless things change. A few days ago as part of my routine exam, I asked my primary care physician to do another thyroid workup. Now my anti TPO-Ab is at 210 IU/mL and my TSH level is a 3.89 uIU/mL (noted as high). My total T4 is 6.0 ug/dL and total T3 is at 109 ng/dL. My primary care wanted to know why I wasn’t seeing the endochronologist at least every 6 months. I am concerned that doing nothing will allow my body to continue to attack and damage my thyroid. Your thoughts?
Hi Cindy,
This is the classic “wait and see” approach that I discuss in articles such as these: https://www.restartmed.com/hashimotos-thyroiditis/
I would suggest reading that article so you can advocate for your own health in the future.
Hello, Dr. Childs,
I just had my TPO checked and it was 19.4 IU/mL. I’ve been gluten, dairy and sugar free for almost two months now. My question is, had I gotten this checked before making these dietary changes do you think it would have been higher?
Hi Shannon,
It’s possible but there are many people who undergo dietary changes such as the ones you described which do not have an impact on their antibody level.
Thank you, Dr. Childs. I have one more question. My PCP did not order the complete set of thyroid lab tests you recommend. She did not order Reverse T3 or Total T3. I plan to ask her to order these, but my question is do all the other tests have to be redone so that they are all taken from the same snapshot in time, or can I just ask her to order those two? The other tests were done on 5/3/19.
I have hypothyroidism and have been taking Nature Throid for 5 years and just switched to Armour. My antibodies have always been <1. Recently I my TPO antibodies was 6.85 and then 2 months later 10.83 (0-34).
Am I developing Hashi?
thank you!
Hi Dr. Childs
Its refreshing to read this article explaining TPO related thyroid issues clearly and in depth. A lot of other information out there is brief and suggesting meds are the only option.
My TSH level have been increasing over the last year and now at 12. My anti TPO is 1210. FT4 has stayed around 15 and FT3 has increased to 6. I had an ultra sound on Thyroid, which showed lobes asymmetric 9cc on the right and 3cc on left. Feel slight hypothyroidism symptoms or maybe its symptoms of antibodies attacking thyroid
I’m trying to avoid hormone replacement meds. Already taking Thyroid supplement with selenium, zinc etc. I also take vit D3 supplement, eat healthy and exercise regularly. Docs saying hereditary and only a matter of time.
Do you think I still have chance of lowering TPO and TSH and staying of meds or am in risk of damaging thyroid?
All advice really appreciated!
Thank you for the article!
Best regards
Andy
Hi Andy,
There is always a chance but the fact that your TSH is increasing is not a good sign as it indicates thyroid gland damage. If you want to take the natural approach then you need to be very aggressive starting right now.
Dear Dr.Childs,
Thank you very much for your article. That was very useful for me.
My TSH level has dropped from 4.5 to 2.8 in the last three months with more levoxine pills and an improved diet. My anti-TPO is reported as>500. I use levoxine 100 mcg (levothyroxine sodium) once per day. Please guide me on how can I decrease my anti-TPO and whether I can reduce the use of this drug?
Hi Atefah,
Please see this article for more information on that topic! https://www.restartmed.com/tpo-antibodies/
Thank you so much for the wonderful resources that enable patients to be their own informed advocate! I just received blood test results with ANA 1:320, TPO= 18, TH=1, RT3=18, T4=.9, T3=2.7. Is it possible I have another autoimmune disease or likely just Hashimoto’s?
Hi Mary,
It’s certainly possible but you’ll need more investigative efforts to figure out if that is the case or not. The tests listed here don’t really give much information on that front.
Hello Dr. Childs,
I have hyperthyroidism with Grave’s antibodies. Currently it is 123 (under 140.) For the past several months, I noticed the antibodies level slowly crept up from 83.
My T3 and T4 levels are slightly under 50%. Once my T3 and T4 started normalizing my doctor slowly weaned me off of Methimazole.
I was on the autoimmune diet for several months. Now I have introduced nightshade, rice, but still off dairy and gluten. What else could I do to normalize my antibodies?
Hi Liz,
Please see this 1-hour podcast episode I did with Dr. Osansky which outlines several treatment options for those with hyperthyroidism and Graves’ 🙂 https://www.restartmed.com/how-to-prevent-thyroid-surgery-and-radioactive-iodine-ablation-therapy-dr-osansky-and-dr-childs/
This article has me nearly in tears as it has validated everything I have been going through as a result of Hashimoto’s Thyroiditis. Endocrinology has told me TPO only needs to be tested once for diagnostic purposes and that the only treatment needed is thyroid hormone replacement to achieve euthyroid. The euthyroid state in his opinion revolves solely on TSH being the only lab to check and keep within the reference range. In my very frustrating experience endocrinology doesn’t understand how much havoc the autoimmune portion of it can cause patients. On the other side, despite specializing in autoimmune conditions, rheumatology won’t take patients with Hashimoto’s Thyroiditis being the sole autoimmune condition. They’ve all just referred me back to endocrinology.
I am extremely blessed to have a primary care provider who actually does look at all of the labs and promotes all of the supplement and diet recommendations you have in this article. Unfortunately following the recommendations does make some difference for me, but I still suffer from almost all of the symptoms you’ve listed above plus one I didn’t see mentioned.
When my TPO rises I experience global edema. It is much worse in my face and lower extremities but it is global. During this time my thyroid gland itself becomes so inflamed I have to be very careful of how I eat and take medication because I have difficulty swallowing. I also suffer from chronic back pain related to fractures in my thoracic spine that have caused permanent nerve damage and some moderate spinal cord displacement. When my TPO rises my back pain is nearly impossible to manage and severely limits my abilities to do even the basic ADLs let alone any of the recreational and social activities I love to do. The fatigue I experience rivals the fatigue I had when I had mononucleosis nearly 20 years ago further limiting my abilities to be an active, productive person. Out of all of symptoms the absolute most terrifying one I have when my TPO rises is encephalopathy. I don’t recognize when this happens I have to rely on friends and family members to tell me I’m not ok to drive, work, or do anything that requires a clear mind. I experience brain fog, my gait becomes ataxic, my speech becomes slowed and slurred, I experience anomic aphasia, and when the swelling comes down I have zero recollection of anything that happened during that period of time. There was a time when my neurological symptoms were so bad they drug tested me at work. I have had extensive work ups performed by neurology including lumber puncture, MRI/MRA, a head CT without contrast, a CTA of the brain, a standard EEG, a three day ambulatory EEG, and some unique blood tests that I can’t remember off the top of my head at this time. Unable to find any problems they can treat in their specialty, neurology has discharged me from their service and has wished me well.
At the moment I am not euthyroid. My T3, T3 reverse, and T4 are all in the optimal range but my TSH is suppressed below normal. As soon as my TSH hits the normal reference range my TPO begins rising and I become symptomatic. Even when my TSH is suppressed I live every day with mild to moderate symptoms.
I have read some recent (within the last 5 years) peer reviewed studies out of Europe and one out of the University of Chicago that have shown drastic improvements in symptom reduction with an elective thyroidectomy in patients with high TPO levels despite being euthyroid. At least one, if not the majority, of the studies followed these patients for a lengthy period of time postoperatively to ensure their perceptions of improvement couldn’t be attributed to a placebo effect. Of course there is an inherent risk with any surgery, and I am well aware of the risk of cutting or damaging the recurrent laryngeal nerve, especially with a heterogeneous thyroid gland, but for a long time I have been thinking that because all else has failed my only two options are to wait for however long it takes the autoantibodies to destroy my thyroid or find someone willing to take my thyroid out. I have been on the Hashimoto’s roller coaster for three years, and it has upended my life. Have you read any of those studies and if so what are your thoughts on elective thyroidectomy for those with severe symptoms despite diet modification, use of recommended supplements, and appropriate medications for hormone replacement?
Hi Angie,
I have not read those studies but I live in a completely different world than the people who would research such a topic. In my view, Hashimoto’s is not only a treatable condition but one that can be actively managed through lifestyle changes, medications, and hormone replacement. In my world, those with Hashimoto’s feel better and would never even think about getting a thyroidectomy for a condition whose side effects and symptoms can almost completely be mitigated with the right approach.
This is the divide, though, between how I approach a disease like Hashimoto’s and how conventional doctors do.
Before thinking about getting a thyroidectomy I would strongly recommend reading the comments and experiences of women and men who have already had it done. You will find that most of them regret it. For instance, the average person gains 20 pounds after the removal of their thyroid and continues to experience symptoms like fatigue and depression.
The idea that you can simply replace lost thyroid hormone with one dose of levothyroxine after thyroid removal is not a reality for most people. But that’s just my opinion based on my experience, I would recommend you do your own research.
Unfortunately, you are not likely to find the type of care that you want in the conventional system. I would recommend looking at this resource for more assistance in finding a competent doctor to manage your thyroid: https://www.restartmed.com/how-to-find-a-doctor-to-treat-your-thyroid/
Hi Dr. Childs,
I was curious to know if testing for the anti-TPO antibodies can ever come back wrong. Or if there is a specific kind of testing that should be done to get the most accurate reading. I recently had testing done and it said my antibodies were almost zero. Which is great. But I was diagnosed with Hashimoto’s thyroiditis about 5 years ago. My thyroid hormones are very suboptimal. Which I’m assuming is why I still feel symptomatic.
Really appreciate the article. I was actually able to read my labs properly because of it. Thank you!
Hi Natalie,
Yes, that can certainly happen. It has been estimated that anywhere from 5-10% of labs are spurious (or inaccurate) when they are drawn. For this reason, it’s always a good idea to double-check a lab result that isn’t in keeping with the big picture.
In terms of accurate thyroid lab testing, you really need to look at all labs in context with one another. Here is an article that outlines my recommended thyroid lab tests: https://www.restartmed.com/normal-thyroid-levels/
Thank you for this detailed article. I was diagnosed 15 years ago with Hypo and this year have gone on a pendulum from hyper back to hypo. They finally tested my TPO at its 1865. I am definitely going to adjust my diet and then keep digging.
Hi Elizabeth,
That sounds like a good idea! You can find some natural treatment options for lowering TPO antibodies here: https://www.restartmed.com/tpo-antibodies/
Hi Dr Childs. I’ve never commented on something like this before, but thought I would today. I was diagnosed T1d 4 years ago (just 2 weeks after my 30th birthday.) Last year they did a thyroid test.
My Free T4 was .81. My TSH 3.52. My TPO AB came back at 1,974.5. (holy moly!!) I KNEW that something was off. Symptoms : Debilitating fatigue, anxiety, brain fog, ocd, mood swings, insomnia, heavy/irregular time of the month, increased sensitivity to heat/cold, brittle/thinning hair, heart palpitations/fast beat, acid reflux, pain in my neck, sore joints/muscles and very low bps (like 84 over 50 ish range). These tests have been done by both my PCP and Endo, yet neither one wants to treat for anything since “My other #’s are in low but pretty ok range still.” I don’t understand with TPO-AB levels like that, the T1d, and all the symptoms why they will not treat or diagnose Hashimotos? The biggest thing is the tired/lack of motivation. It’s HORRIBLE. I can have 5 energy drinks or coffees and still want a nap! (Not that I WOULD, but ya know…) What should I do here? Find another Dr? Push them to test again? Treat at home with…. suppliments that would help until? I’m just blown away.
– Appreciate your time friend.
*Merinda
Hi Merinda,
It may seem confusing but the reason they won’t diagnose or treat you is that they don’t have any treatments to offer aside from thyroid medication and they only give that to you when your numbers decline to a certain level. That’s just the nature of how doctors look at Hashimoto’s thyroiditis and why patients who are diagnosed with it seek out additional help and treatments. It’s always worth trying things like diet, supplements, exercise, stress reduction, etc, if you have any thyroid disease because those therapies are pretty much never harmful and only have the potential to help. You can find some natural therapies here: https://www.restartmed.com/natural-thyroid-remedies/
Dr Westin Childs,
Like so many people I have diagnosed with Hashimoto’s disease. Eight years ago, I had melanoma in my scalp and then endured 5 weeks of head/neck radiation which probably impacted my thyroid. I have no symptoms of Hashimoto’s. I energy level is great, feeling generally good, exercise regularly. Doctor’s have prescribed all formulations of thyroxine and I even tried NP thyroid, all of which made me ill and actually induced symptoms of hypothyroidism; they were like a poison to my body. I have recently been taking supplements and feel incrementally better ( because I have not felt bad). I have seen several endocrinologists, but since I am not taking synthetic hormones, they will not treat me. Any suggestions? There are actually been studies and articles published synthetic hormones cause problems for people, especially those who have had head or neck cancer and results in a lower quality of life. Thanks for your time.
Hi Michael,
Yes, if you can’t (or won’t) take conventional medications then your only option becomes natural therapies. You can learn more about the various therapies and how effective they are for managing thyroid disease here: https://www.restartmed.com/natural-thyroid-remedies/
Dr Childs,
Sure wish you were practicing! You sound very knowledgeable and more importantly it sounds like you care about the quality of your work, something my endo seems to lack.
I am suffering most hyperthyroid/Grave’s symptoms, but when tested my endo says everything is in range.
The problem is, tests were all run in sub-optimal conditions
* Run in the afternoon, non-fasting
* I was taking a multi with higher than normal 300mcg Biotin (1000% RDA) and 150mcg Iodine (100% RDA)
* I take 40mg Propranolol, concerned that could have affected results
So I do not trust the results, and the results don’t agree with my sufferings
1. Is 300mcg Biotin enough to affect the antibody results?
2. Is 150mcg Iodine likely to affect results?
2. Can 40mg propranolol affect results?
3. Can you clarify what you mean by “antibodies should be non-existent or as close to 0 as possible”. If I am within the reference range, is that considered “close to 0”?
anti-TPO antibodies = <5, range <9 (intlUnit/mL)
Thyroglobulin Antibody = <1, range <4 (IntlUnit/mL)
results state clearly: Biotin supplements may falsely DECREASE this analyte.
Thank you for your time, and your site. You are helping many!
I had papillary cx of thyriod with total Thyroidectomy in 2010 and iodine ablation. All follow studies for the first 8 years have been negative. I have not seen endocrine provider since 2018. Blood test for total antibodies thyroid globulin came back elevated at 65. Does this mean my cx has returned.
Hi Cherie,
Not necessarily, but it would be a good idea to get checked out.
Hello. My recent experience is swinging from hypo to hyperthyroidism from most recent blood panel results June 30, 2023 with TPO antibody at 648 and
With TSH at .086.
I spent thousands of dollars last year June to December treating hypothyroid totally with supplements and dietary restrictions. Numbers came down nicely.
Now it seems I’ve swung to opposite side and previous specialist seems not interested in helping me figure this out.
What can you do to help?
PS. After completing program with specific supplements etc, I’ve had to go on my own with supplements. I’ve maintained the dietary boundaries (no gluten, no dairy, no processed).
It’s a mystery, help please.
I’m NOT interested in conventional medical help. And the previous doc is MD certified but appears restricted to what he only wants to treat (hypothyroid)
This was interesting but perplexing for me. I had recent tests as I’m convinced my thyroid is not working properly. I’ve had hypo symptoms for many years but my tests are always in “normal” range and I can’t get treatment. I’m on LDN for rosacea, but it has helped improve hypo symptoms a little, although not weight loss. I had both TPO at 12.6 Kiu/L and thyroglobulin antibodies at 12.3 kiu/l. I did not stop LDN for the test. My tsh is 1.47 miu/l free t3 1.47 pmol/l free t4 1.445 ng/dl. My ferritin was lower 33.6 ug/l folate serum 8.7. B12 44.8 pmol/L.
Hi Kit,
I would recommend reading this article for more insight on thyroid lab tests and when they are actually normal: https://www.restartmed.com/normal-thyroid-levels/